47
Pediatric Macular Surgery
Mark K. Walsh  Antonio Capone
Antonio Capone  Jr.
Jr.  Michael T. Trese
Michael T. Trese
Pediatric macular surgery offers a unique and interesting set of challenges relative to adult macular surgery. Not only is there a reduced margin for error but the pathology can be fundamentally different than that seen in adults. With this extra challenge come potentially great rewards, as improved vision can dramatically affect the lives of our young patients for many decades.
With regard to the various indications for macular surgery in pediatric patients, most of us are probably most familiar with traumatic macular holes and submacular surgery for choroidal neovascularization (CNV). In addition to these two topics, we will also cover surgery for combined hamartoma of the retina and retinal pigment epithelium (RPE) and the recently described “posterior hyaloid contracture syndrome” seen most frequently in retinopathy of prematurity and familial exudative vitreoretinopathy.
COMBINED HAMARTOMA OF THE RETINA AND RETINAL PIGMENT EPITHELIUM
Combined hamartomas of the retina and retinal pigment epithelium (CHRRPE) are rare tumors that are thought to be congenital in nature (1). In 1973, Gass described seven cases (five in children, two in young adults) he believed to be hamartomatous malformations involving the pigment epithelium, retina, retinal blood vessels, and overlying vitreous (2). Hamartomas are benign lesions composed of an overgrowth of mature cells that occur normally in the affected area. These combined hamartomas have varying clinical appearances. They are often pigmented with minimal elevation and demonstrate vascular tortuosity with associated vitreoretinal interface abnormalities. Unlike choroidal melanomas, for which they are often confused, CHRRPE mainly involve the retina and RPE versus choroid. Additionally, rarely do choroidal melanomas demonstrate marked vascular tortuosity in lesions of comparable size, nor do they demonstrate vitreoretinal interface abnormalities or epiretinal membrane formation in general. Ocular complications of choroidal melanoma including retinal detachment, subretinal hemorrhage, vitreous hemorrhage, inflammation, and glaucoma are not typically associated with CHRRPE (1). CHRRPE lesions may grow in some instances, though (3).
CHRRPE may be classified by both location (lesions on the disc, adjacent to the disc, macular, or midperipheral (2) and predominant tissue subtype (melanocytic, vascular, or glial (1). It is the glial subtype with prominent epiretinal proliferation that may be most amenable to macular surgery. In the Macula Society Research Committee report on CHRRPE, 47 of 60 (78%) patients with CHRRPE (all unilateral cases in this series) were noted to have vitreoretinal interface change and/or epiretinal membrane formation. Twenty-four percent of patients for whom follow-up data were available lost vision, presumably from progressive distortion of the retina. Of note, Gass hypothesized that in some cases of CHRRPE, the epiretinal tissue is so intricately interwoven with the underlying dysplastic retina that surgical peeling may not be possible (4). In a report by Shields et al. (5), 10 of 11 (91%) patients with CHRRPE had preretinal membrane by optical coherence tomography (OCT), none of which were intertwined with the tumor tissue.
In the Macula Society report, three out of the 60 patients had vitreous surgery to remove the epiretinal membrane. One of the patients had improved vision following surgery (from 20/200 to 20/40), while the other two had no change in vision. Based on two adult cases of CHRRPE who had undergone epiretinal membrane peeling without visual improvement, McDonald and colleagues (6) concluded that the role of vitrectomy and membrane removal in CHRRPE cases appeared to be limited. Both of their cases had longstanding poor vision prior to surgery which may have impacted their postoperative visual outcomes. In contrast, Sappenfield and Gitter (7) reported both subjective and objective improvement in vision after vitrectomy with membrane peeling in an adult patient with longstanding poor vision. Mason and Kleiner (8) reported a woman with CHRRPE who on first exam had 20/30 vision that deteriorated to 20/400 secondary to increased epiretinal membrane with an associated full-thickness macular hole. One year later, vitrectomy with membrane peeling with perfluoropropane gas tamponade was performed. The hole closed and vision improved to 20/100. Mason (9) reported a 20-year-old woman with CHRRPE whose declining vision improved from 20/400 to 20/60 after vitrectomy with membrane peel.
In terms of surgical intervention in children with CHRRPE, the literature is rather sparse. Konstantinidis et al. (10) discuss two cases of CHRRPE, one in a 12-year-old girl and the other in a 14-year-old boy, both of whom demonstrated progressive visual decline. Both were noted by OCT to have a thickened posterior hyaloid and epiretinal membrane inducing vitreomacular traction. Vitrectomy with membrane peeling was performed in both cases with improvement in vitreomacular traction and macular distortion noted on OCT and improvement in vision from 20/100 in both cases to 20/40 and 20/25, respectively. Standard three-port pars plana vitrectomy was performed in both cases. Tight adherence of the posterior hyaloid necessitated the use of the vitrector, end-grasping forceps and horizontal scissors to remove in both cases. Multiple layers of epiretinal membrane were noted in both cases and internal limiting lamina was peeled in one of the two cases. Stallman (11) performed vitrectomy with membrane peel on a 10-year-old girl whose vision had declined from 20/100, 3 years earlier, to 2/200. He also performed standard three-port vitrectomy, but in contrast to the previous two cases, here the membrane was removed easily in one single sheet. Nine months postoperatively the vision had improved to 20/40.
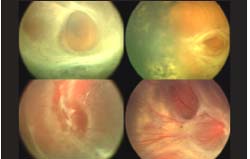
At William Beaumont Hospital, we have recently reviewed our surgical experience in pediatric patients with CHRRPE (in preparation). From 1999 to 2007, we performed vitrectomy with membrane peeling in 11 eyes with CHRRPE in 10 patients (bilateral in one case without known systemic association; see Figs. 47-1 and Figs. 47-2). In cases deemed more complicated preoperatively, plasmin was used to help facilitate removal of the posterior hyaloid and epiretinal membranes. Surgeries were performed in both 3-port and 2-port fashion. Patient ages ranged from 18 months to 14 years and follow-up ranged from 6 to 42 months. Six out of 11 (55%) eyes underwent plasmin enzyme-assisted vitrectomy while the other five were done without plasmin assistance. Eight out of 11 (73%) lesions were restricted to the macula and all showed significant epiretinal proliferation. Four out of 11 (36%) eyes had recurrence of epiretinal membrane, for which 3/4 underwent repeat vitrectomy with membrane peeling. No surgical complications were noted. Eight out of eleven (73%) eyes showed improvement in visual acuity while the other three showed stabilization. Four out of six (67%) plasmin cases showed improved vision.
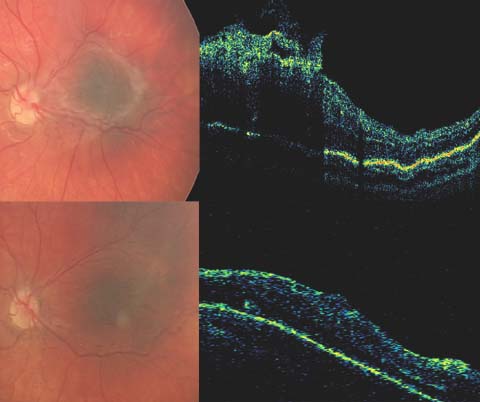
Figure 47-1. Pediatric combined hamartoma of the retina and retinal pigment epithelium (CHRRPE) surgery. Preoperative fundus photo and optical coherence tomography (top) and postoperative (bottom) images from an 18-month-old with CHRRPE. The patient underwent plasmin enzyme-assisted vitrectomy with membrane peeling. Postoperative images show improved macular architecture with absence of epiretinal proliferation.
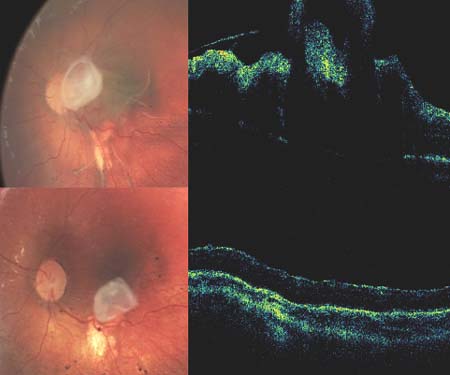
Figure 47-2. Pediatric combined hamartoma of the retina and retinal pigment epithelium (CHRRPE) surgery. Preoperative (top) and postoperative (bottom) fundus photos and optical coherence tomography images from a 2-year-old with CHRRPE. Although some epiretinal proliferation was not removed, notice the improvement in macular architecture.
If our 11 pediatric surgical cases are added to the three other cases reported in the literature, 11/14 of these eyes have had visual improvement after vitrectomy with membrane peeling, while the other three eyes had stable vision. Certainly, in the pediatric population, CHRRPE lesions with significant epiretinal proliferation and retinal distortion leading to decreased vision should be evaluated for vitrectomy with membrane peeling, and consideration should be given to plasmin enzyme assistance.
PEDIATRIC MACULAR HOLE SURGERY
Macular holes in the pediatric population are typically seen following trauma, typically closed globe direct mechanical contusion injuries (12). The pathogenesis is unclear although vitreous and posterior hyaloid traction on the retina probably plays a role.
In traumatic cases, some macular holes seem to evolve, although most tend to occur immediately at the time of insult. In addition, traumatic macular holes are thought to spontaneously resolve more frequently than idiopathic macular holes. Lai et al. (13) reported a case of traumatic macular hole in a 12-year-old boy following soccer ball contusion. This hole was associated with a retinal detachment, both of which spontaneously resolved by 3 weeks following the injury with vision improving from 20/150 to 20/80. Carpineto et al. (14) reported a traumatic macular hole in a 10-year-old child that resolved spontaneously at 18 weeks. Vision improved from 20/200 to 20/25. Mitamura et al. (15) reported 11 cases of traumatic macular holes, 7 of which closed spontaneously. Of the holes that closed spontaneously, young age was a common feature (ranging between 8 and 17 years), as was small size of the hole (0.1–0.2 disc diameters), no posterior vitreous detachment (PVD), and good final visual acuity. All of these patients that had spontaneous closure had improvement of at least two lines of visual acuity, with five of the patients improving to 20/20. The duration of the macular hole prior to closure ranged from 1 to 12 months (mean of 5.4 months). Yamada et al. (16) also reported spontaneous closure of two small traumatic macular holes in children. Yamashita et al. (17) also reported on the spontaneous closure of traumatic macular holes in eight out of 18 cases. Seven of the eight cases were in children and closure occurred within 4 months in all cases. Seven of the eight cases also involved holes 0.2 disc diameters or smaller. Larger traumatic holes in children may spontaneously close, too (18).
Kuhn et al. (12) evaluated 17 eyes that had undergone vitrectomy with internal limiting lamina (ILL) peeling with gas tamponade for traumatic macular hole. Seven of their cases were in children (less than 18 years old). Average time to surgery in these pediatric cases was 1.3 months. All of these children had closed holes and improved vision postoperatively with follow-up times ranging from 3 to 21 months.
Wachtlin et al. (19) performed vitrectomy with platelet concentrate adjuvant and SF6 gas tamponade in four children with traumatic macular holes from 1 to 5 months after the trauma. All holes closed and vision improved by four to seven lines (20/25–20/100 final visual acuities) with a mean follow-up of 35 months.
Margherio et al. (20) first described the use of autologous plasmin enzyme assisted vitrectomy (e.g., see Fig. 47-3) with membrane peeling and gas tamponade for traumatic macular holes in children. Plasmin was used to facilitate posterior hyaloid separation. They described four children (all less than 14 years of age) who all improved by four to eight lines postoperatively. Final visual acuities ranged from 20/30 to 20/60 with two eyes developing transient posterior subcapsular cataracts and no eyes requiring reoperation. Chow et al. (21) also reported surgical success with vitrectomy with plasmin assistance (in six of seven pediatric patients) and gas tamponade without the use of other adjuvants such as transforming growth factor-beta or platelet concentrate. Six of seven holes closed postoperatively; one chronic hole present for almost 3 years did not. Four of seven eyes showed improved vision at last follow up with the other three unchanged. No patients were excluded from their review including those with choroidal ruptures.
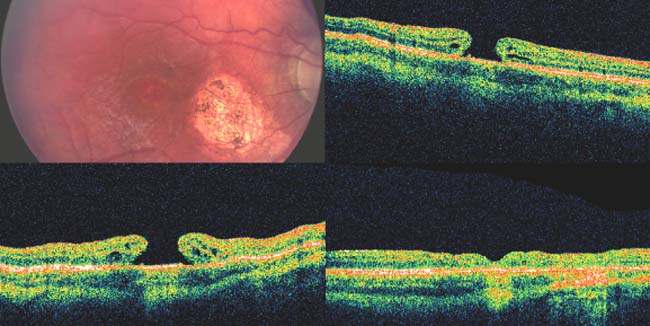
Figure 47-3. Pediatric macular hole surgery. Optical coherence tomography (OCT)and fundus image (top) of a chronic (2.5 year) traumatic macular hole in a 10-year-old boy. He underwent plasmin enzyme assisted vitrectomy with membrane peeling and gas tamponade, but his hole remained open postoperatively as seen in repeat OCT (bottom left). His hole closed after a second vitrectomy surgery with repeat membrane peeling (bottom right). Despite anatomic success, his vision did not improve, likely related to the chronicity of the hole.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


