Pathology of Glaucoma
Christine E. Callahan
Joseph W. Sassani
The glaucomas are a diverse group of disorders that cause a characteristic optic neuropathy, resulting in loss of neuroretinal rim tissue, distinctive optic nerve head cupping, and visual field loss. The intraocular pressure (IOP) in glaucoma is usually elevated above normal values, and this increase in IOP is believed to lead to alterations in optic nerve structure and function. However, IOP elevation does not need to be present to make the diagnosis of glaucoma, and patients with typical optic nerve structural alterations and visual field loss in the presence of normal IOP are diagnosed as having low-tension or normal-pressure glaucoma. Conversely, patients with elevated IOP in the absence of detectable secondary abnormalities in optic nerve structure and function are classified as ocular hypertensives. The glaucomas are, therefore, a group of syndromes that require for diagnosis characteristic abnormalities in optic nerve anatomy and function rather than an elevated IOP.
Epidemiology
The worldwide prevalence of glaucoma is estimated at nearly 66.8 million, representing the second most common cause of vision loss in the world.1 In the year 2000, there were an estimated 937,000 blind Americans older than 40 years of age.2 In this population, glaucoma was the most common cause of blindness in Hispanic Americans, accounting for 28.6% of cases. In black Americans, glaucoma was second to cataracts as a cause of blindness, accounting for 26% of cases, and in white Americans, 6% of blindness was caused by glaucoma.2 Primary open-angle glaucoma (POAG) affects >2 million people in the United States, and this number is expected to climb to >3 million people in the year 2020.3 The overall prevalence of POAG in the U.S. population age 40 years and over is estimated to be 1.86%, with 1.57 million white and 398,000 black persons affected.3 Black patients had almost three times the age-adjusted prevalence of glaucoma than white subjects.3 Further data on the incidence and prevalence of glaucoma will be presented as individual syndromes are discussed.
Classification
The following is a useful classification of the glaucomas, constructed with reference to the anatomy of the anterior chamber angle as well as to specific pathophysiologic and etiologic factors:
Normal outflow
Hypersecretion glaucoma
Impaired outflow
Congenital glaucoma (developmental)
Primary glaucoma
Angle closure
With pupillary block
Without pupillary block
Open angle
Secondary glaucoma
Angle closure
With pupillary block
Without pupillary block
Open angle
Variable outflow
Normal-pressure (low-pressure) glaucoma
Normal Outflow
Hypersecretion Glaucoma
Hypersecretion glaucoma is rare and is said to have no antecedent cause.4 It is characterized by a normal outflow facility accompanied by elevated IOP, presumably secondary to increased production of aqueous humor. It affects mainly middle-age women, particularly those having neurogenic systemic hypertension. The histology of the trabecular meshwork is said to be normal. Some authors question the existence of hypersecretion glaucoma as a discrete entity.
Impaired Outflow
Embryologic Development and Glaucoma
Cells of the neural crest, which arise at the margins of the embryologic neural plate just before the closure of the neural tube, contribute to large portions of the eye, orbit, and head. Specific ocular tissues that may be derived from the neural crest include corneal stroma and endothelium; sheaths and tendons of the extraocular muscles; anterior iris stroma; iris melanocytes; ciliary muscles; choroidal stroma; meningeal sheaths of the optic nerve; orbital bones; ciliary ganglion; sclera; intraocular vascular pericytes; and portions of the trabecular meshwork, including endothelium. Neural crest cells also contribute to important structures of the orbit and head, including the meninges, pituitary gland, bones and cartilage of the upper face, dental papillae, and connective tissue supporting cells of the orbit.
As several studies have assessed,5,6,7,8,9,10,11 the neural crest cells are believed to move into the developing eye in three waves that pass between the surface ectoderm and the lens. The first wave of cells differentiates into the corneal endothelium by the eighth developmental week and produces the trabecular meshwork and its endothelium. The second wave infiltrates between the corneal epithelium and endothelium to form keratocytes. The third wave produces the iris stroma. Subsequently, the iris pigment epithelium is derived from neural ectoderm.
The anterior chamber is formed at approximately 7 weeks. The anterior chamber angle is demarcated by week 15 as the cells that will become the corneal endothelium meet the anterior surface of the developing iris. Neural crest cells develop into the trabecular meshwork cells, which from week 15 to the eighth month of gestation differentiate and deposit the trabecular beams. At the end of the third month of gestation, Schlemm’s canal and vascular endothelium, derived from vascular mesoderm, have developed, and the future ciliary processes are covered by epithelium, derived from two layers of neuroectoderm.12,13
The widespread contributions of neural crest–derived cells in the embryology of the eye have given neural crest a central role in the pathogenesis of several forms of glaucoma. Congenital and developmental anomalies that involve the neural crest cells are termed neurocristopathies. These abnormalities in neural crest cell migration and differentiation may explain many of the developmental abnormalities of the face and head associated with various glaucoma syndromes. Table 1 attempts to correlate anterior segment disorders with the presumed abnormality in neural crest cell function. This table will be referenced later in this chapter as several glaucoma syndromes are discussed.
Table 1. Classification of Anterior Segment Disorders Based on Neural Crest Origins | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||
Congenital Glaucoma
The term congenital glaucoma designates glaucoma that is detected in the neonatal and infantile periods. The incidence of congenital glaucoma is approximately 1 in 10,000 births.14 Usually, it is sporadic; however, autosomal inheritance has been reported.15,16 Recent studies have demonstrated an association between autosomal recessive inheritance of congenital glaucoma and mutations in the CYP1B1 gene at the GLC3A locus.17,18,19 Congenital glaucoma is bilateral in 64% to 88% of cases,20,21 and most affected persons are boys (60% to 70%).15 It is diagnosed within the first year of life in 86% of cases, with 40% diagnosed at birth and 34% between birth and 6 months of age.15
There have been many theories relating to its pathogenesis. The surface of the trabecular meshwork in congenital glaucoma has been described as having a peculiar sheen on gonioscopic examination. This finding has suggested to some authors the presence of an abnormal mesodermally derived membrane, Barkan’s membrane, covering the surface of the trabecular meshwork and preventing the efflux of aqueous. The effectiveness of goniotomy surgery and the ineffectiveness of miotics in the treatment of congenital glaucoma have been cited in support of this theory. There is, however, little histologic proof for this theory.
Until recently, the anterior chamber angle was thought to arise through a process of cleavage of mesodermal tissue. Arrest in this process was said to result in an “embryonic” configuration of the anterior chamber angle (Fig. 1). This immature angle is characterized histologically by an anterior insertion of the iris root on the ciliary body, anteriorly displaced ciliary processes, and insertion of the ciliary meridional muscles into the trabecular meshwork and the presence of mesenchymal tissue in the anterior chamber angle.15 Although an “embryonic” anterior chamber angle is found in congenital glaucoma, it is also seen in age-matched persons who do not have the disorder (Fig. 1). Further, difficulties in interpreting histologic sections in this age group are compounded by the few truly meridional sections encountered in the usual serial sectioning of the globe. Thus, sectioning artifact enhances the appearance of an “embryonic” configuration in the anterior chamber angle.
More severe abnormalities in the mesodermal cleavage process were thought to result in the anterior chamber cleavage syndromes: Axenfeld, Rieger, and Peters syndromes.22 Axenfeld anomaly is characterized by posterior corneal embryotoxon (anteriorly displaced Schwalbe’s line) and iris adhesions to Schwabe’s line. When Axenfeld anomaly is associated with glaucoma, it is termed Axenfeld syndrome. Rieger anomaly may include posterior embryotoxon, iris stands, corectopia, polycoria, and ectropion uvea. Rieger anomaly may also be associated with hypoplasia of the malar bones, congenital absence of some teeth, and mental retardation. When glaucoma is found in association with Rieger anomaly, it is termed Rieger syndrome. Ophthalmic findings in Peters syndrome include central or paracentral annular corneal opacity, iris stands, cataract, microcornea, cornea plana, sclerocornea, aniridia, colobomas of the iris or choroid, and glaucoma due to dysgenesis of the angle. Of particular public health importance is the recently recognized association of Peters’ syndrome and fetal alcohol syndrome, which is secondary to maternal alcohol ingestion early in the first trimester of pregnancy. It is the most common known cause of mental retardation in the United States.23 Affected infants have a characteristic appearance that includes microcephaly, microphthalmia, a poorly developed philtrum, short palpebral fissures, a thin upper lip, and flattening of the upper maxillary area. Approximately 90% of children with fetal alcohol syndrome have additional ocular abnormalities,24 which in addition to Peters’ anomaly may include optic nerve hypoplasia,24,25,26 tortuosity of retinal blood vessels,24,25 strabismus,24,27 and ptosis.24
The anterior cleavage syndromes now are recognized as being caused by abnormalities in neural crest development.28 The recognition of the contribution of neural crest–derived cells in the embryology of the anterior chamber angle may provide the means for unifying several glaucoma syndromes, particularly those associated with congenital glaucoma.
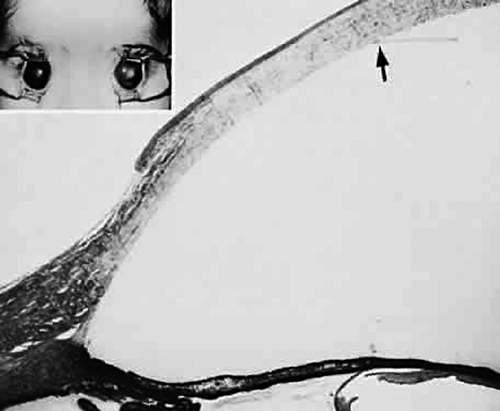
A syndrome of congenital glaucoma associated with iridotrabecular dysgenesis and ectropion uveae has been described.29 In these patients, the iris pigment epithelium proliferates onto the anterior iris stroma in utero so that congenital ectropion uveae is present (Fig. 2). Glaucoma may be present in infancy or may develop later in life. Histologically, the central corneal stroma is normal; however, there is posterior embryotoxon with iris processes. Migration and hyerplasia of the pigment epithelium onto the anterior iris surface is accompanied by endothelialization of the iris surface peripheral to the area where pigment epithelium is present. Angle closure with iris adherent to a normally differentiated trabecular meshwork also is seen. The iris stroma is hypoplastic. The relation of this syndrome to the anterior chamber cleavage syndromes and to the iridocorneal endothelial (ICE) syndrome has not been established. This syndrome may bridge the groups of disorders characterized in Table 1 as secondary to abnormal crest cell migration and proliferation.
Both ocular and systemic disorders may be associated with congenital glaucoma. Table 2 outlines other ocular disorders that may be associated with congenital glaucoma. The possible relation of abnormalities in neural crest cell migration to the developmental disorders in the table remains to be established. Congenital glaucoma is a common feature of several systemic disorders, summarized in Table 3. The multiple ocular anomalies and systemic disorders associated with congenital glaucoma suggest the probability that multiple factors may result in impaired aqueous outflow.
Table 2. Ocular Disorders Associated with Congenital Glaucoma | ||
|---|---|---|
|
Table 3. Systemic Disorders Associated with Congenital Glaucoma | ||
|---|---|---|
|
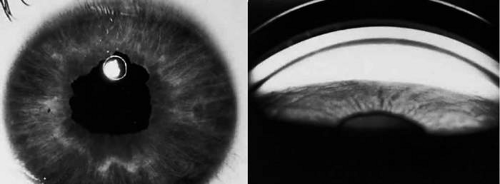
Prolonged elevation of IOP results in characteristic histopathologic changes in the eyes of children 10 years of age or younger. These effects are independent of the specific etiology of the IOP elevation. Ocular stretching, particularly at the corneoscleral limbal region, results in limbal ectasia and the clinical appearance of buphthalmos (Fig. 3). If the thinned and stretched limbus also is lined by uvea (e.g., with peripheral anterior synechiae), a limbal staphyloma is present. When this area extends posteriorly to involve the ciliary body region of sclera, it is called an intercalary staphyloma.
The stretching of the entire anterior segment of the globe is also reflected in corneal enlargement. The 95% range of normal corneal diameters is as follows: age 1 month, 9.4 to 11.0 mm; 6 months, 10.5 to 11.7 mm; and 12 months, 10.8 to 12 mm.30 A corneal diameter of 11.0 mm or less is found in only 24% of patients with primary congenital glaucoma younger than 3 months of age and in only 9% of those older than 3 months of age so afflicted.31 Progressive corneal enlargement ruptures Descemet’s membrane and produces Haab’s striae. These breaks, which are usually horizontal in the central area and concentric toward the limbus, are generally in the lower half of the cornea and are usually associated with corneal edema (Fig. 3).
As in adult glaucomas, optic nerve cupping is a characteristic and diagnostic finding in congenital glaucoma. However, in congenital glaucoma, cupping is an early finding and is frequently reversible in its early stages.
Late manifestations of congenital glaucoma include fibrosis of the iris root and trabecular meshwork; disappearance of Schlemm’s canal; and generalized atrophy of the ciliary body, choroid, and retina.
Primary Glaucoma
Angle-closure Glaucoma (Narrow Angle; Acute Congestive)
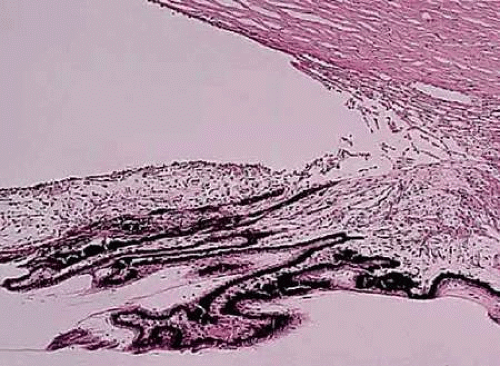
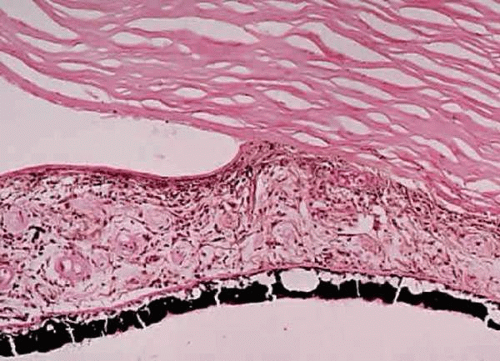
Primary angle-closure glaucoma (PACG) results from an anatomically anomalous anterior segment of the globe (Fig. 4). This configuration predisposes to the apposition of the iris to the surface of the filtering trabecular meshwork. Occlusion of the filtering trabeculum by the iris results in obstruction to aqueous outflow and subsequent IOP elevation, which may be precipitous (Fig. 5).
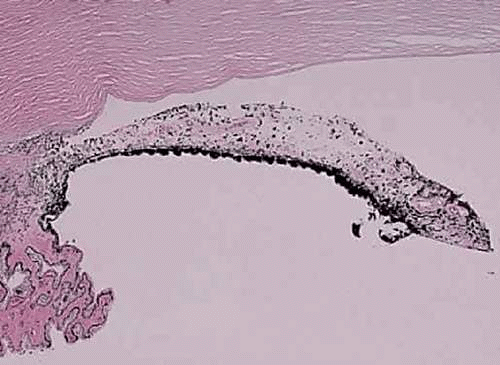 Figure 4. Photomicrograph illustrating an anatomically narrow anterior chamber angle configuration in a “crowded” anterior segment most characteristic of hyperopic persons. (H&E, 10×) |
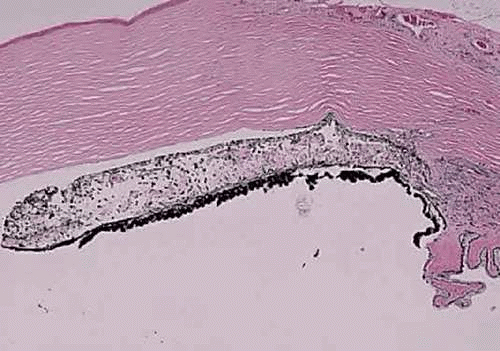 Figure 5. Peripheral anterior synechiae seen in patients with untreated angle closure or treatment delay and angle closure. (H&E, 10×) |
Quigley and Broman have performed extensive research regarding the epidemiology of angle-closure glaucoma. It is projected that in 2010, there will be in excess of 15 million people with angle-closure glaucoma, and this number is predicted to rise to 21 million by the year 2020.32 The highest incidence of angle-closure glaucoma is found in China, India, and Southeast Asia, accounting for an estimated 47.5%, 23.7%, and 13.6% of angle-closure glaucoma in the world.32
The anomalous anterior segment that may lead to PACG causes either classic pupillary block–mediated closure or a nonpupillary block mechanism of closure. Eyes that display a pupillary block mechanism have a shallow anterior chamber, increased lens thickness, and decreased axial length. The resulting congenital anatomic predisposition to angle closure is compounded by further lens thickening resulting from advancing age. In such persons, when the pupil is dilated to the midposition, contact between the pupillary border and crystalline lens occurs and resistance to the passage of aqueous between the lens and iris results in relative accumulation of aqueous posterior to the iris, thus causing a forward ballooning of the iris (bombé). This pupillary block then permits the iris to contact the filtering trabecular meshwork and effectively close the filtering angle.
The nonpupillary block mechanism of PACG is due to a plateau iris configuration. In these patients, the anterior chamber is of near normal depth centrally; however, the peripheral iris has an unusual contour and an extremely anterior insertion on the ciliary body. Dilating the pupil in these patients causes the iris to be drawn up toward the filtering trabeculum, without pupillary block precipitating the event.33,34 The ultrasound biomicroscope has demonstrated the presence of anteriorly placed ciliary processes in patients with plateau iris.35,36
Prior to an attack of PACG, the trabecular meshwork is normal. After repeated attacks, often at a subclinical level, the anterior chamber angle, although open, may become damaged through sclerosis or fibrosis. This damage to the trabecular meshwork may simulate chronic open-angle glaucoma. Similarly, patients with normal-tension glaucoma (NTG) should be examined carefully to confirm that that subclinical attacks of angle-closure glaucoma are not the cause of optic nerve damage, as interval IOPs might return to normal levels.
When IOP rises suddenly, as in acute angle-closure glaucoma, swelling of the iris root and occlusion of the anterior arterial circle of the iris or of one or more of its branches may result in occlusion of the arterial supply to the iris stroma and secondary iris necrosis. Subsequently, segmental iris atrophy, usually in its upper half, may be seen. Extreme atrophy occasionally results in a full-thickness iris hole that may cure the pupillary block. Histologically, there is marked atrophy of the stromal layer of the iris and a varying degree of pigment epithelial atrophy. Iris sphincter ischemia during the period of acute IOP elevation compounds the attack by fixing the pupil in the mid-dilated position and may render it unresponsive to topical miotics, which are usually given to break the attack. Later, secondary dilator and sphincter muscle atrophy may result in an irregular pupil. This muscular atrophy or iris necrosis can be demonstrated histologically (Fig. 6).
The lens also is affected by an attack of angle-closure glaucoma. Glaukomflecken are anterior subcapsular, tiny gray-white lens opacities seen after an attack of acute angle-closure glaucoma37 (Fig. 6). They probably result from interference with lens epithelial cell metabolism, either through a direct pressure effect or through alterations in the normal constituents of the aqueous during the angle-closure attack. Histologically, tiny areas of adjacent subcapsular cortical degeneration are seen accompanying small areas of epithelial cell necrosis.
Visualization of the optic nerve during an attack of angle-closure glaucoma frequently is limited because of corneal edema. However, if the cornea is cleared with topical glycerol, optic disc edema often is present.
The treatment of PACG is to make an opening in the iris, either through a cutting procedure (iridectomy) or with the aid of a laser (iridotomy).38 The goal of these procedures is to create a pressure-relief communication between the anterior and posterior chambers of the eye so as to prevent the buildup of pressure behind the iris, thereby eliminating iris bombé. If peripheral anterior synechiae are forming, or if iridotomy fails to correct the angle closure, and plateau iris is suspected, laser gonioplasty may be required.39,40,41
Open-angle Glaucoma (Chronic Simple Glaucoma; Idiopathic)
POAG is a bilateral condition that by definition includes a glaucomatous optic neuropathy and a filtration angle that is open on gonioscopic examination. POAG may be asymmetric in presentation with variability in time of onset, IOP, and severity of disease when eyes are compared. The diagnosis is, to some extent, one of exclusion because secondary causes must be ruled out before the diagnosis is made. It is projected that in 2010, there will be in excess of 10 million people in the world with open-angle glaucoma, and this number is predicted to rise to 12 million by the year 2020.32 The highest incidence of open-angle glaucoma is in Europe, China, India, Africa, and Latin America, accounting for an estimated 23.9%, 18.6%, 18.4%, 13.9%, and 12.0% of the open-angle glaucoma in the world.32 The incidence of the disorder shows wide racial and ethnic variations. It is documented to be a severe problem among blacks, of whom more than 11% are affected by age 80 years.42
POAG is considered to be a genetically determined disorder. In patients with POAG, 50% have a family history of the disorder.43 The exact mode of inheritance is not definitely established for most glaucomas; however, some juvenile and adult open-angle glaucomas have been mapped to the long arm of chromosome 1.44,45,46
The nature of the obstruction to aqueous outflow in POAG is not known, although it is commonly believed to be located in the area of the juxtacanalicular connective tissue adjacent to Schlemm’s canal.47,48,49,50,51,52 Unfortunately, few early cases of POAG have been examined histologically. One must be cautious in interpreting specimens from more advanced cases, because the histologic findings may reflect secondary effects due to elevated IOP or from the medication used to treat it. Even greater caution must be used in interpreting specimens removed at surgery for glaucoma, as surgically induced artifact may interfere with accurate assessment. Thus, reports of sclerosis of the trabecular meshwork, compression of Schlemm’s canal, or changes in the number of macrovacuoles in the endothelial lining of Schlemm’s canal may, in fact, reflect end-stage glaucomatous changes or may be artifacts related to fixation and surgical trauma.
The relation of changes in the trabecular extracellular matrix, including acid mucopolysaccharides, glycoproteins, glycosaminoglycans, and collagen fibrils, to the pathophysiology of POAG remains to be determined.53,54,55 A significant decrease in the number of trabecular endothelial cells, when compared with that found in age-matched controls, has been reported in patients with POAG.56,57 This finding can be viewed as an acceleration of the usual age-related decline in the number of trabecular endothelial cells.57,58 Similarly, in POAG, some authors have reported histologic evidence for premature accentuation of the usual age-related development of the scleral spur, characterized by compaction of the uveal meshwork against the scleral roll, hyalinization of the adjacent ciliary muscle, and atrophy of the iris root.58
In the normal person, an age-related decrease in aqueous facility of outflow is accompanied by a parallel decrease in aqueous production. The net result is a quantitative balance between aqueous production and aqueous outflow. POAG can be viewed as an imbalance in the usual parallel relation of these aging changes. POAG itself may represent a multifactoral problem with a final common pathway of elevation in IOP.
Secondary Angle-closure Glaucoma
Secondary angle-closure glaucoma (SACG) can be subdivided in a manner similar to PACG as follows:
SACG with pupillary block
Untreated PACG
Phacogenic
Phacomorphic
Secondary to lens subluxation or dislocation
Posterior synechiae induced
Inflammatory
Aphakic or pseudophakic pupillary block
Ciliary block/Malignant glaucoma
SACG without pupillary block
Secondary to sheetlike cellular or vascular proliferations in the anterior segment
Neovascular glaucoma (rubeosis iridis)
ICE syndrome
Epithelial downgrowth
Stromal ingrowth
Endothelialization of the anterior chamber angle
Secondary to anterior displacement of anterior segment structures
Postoperative complications/Iatrogenic
Tumor or cyst related
Retinopathy of prematurity
Persistent hyperplastic primary vitreous
Anterior rotation of the ciliary body, inflammation, and uveal effusion
Miscellaneous
Iridoschisis
Fuchs’ dystrophy
Cystinosis
Untreated Primary Angle-closure Glaucoma
Untreated angle-closure glaucoma results in the formation of peripheral anterior synechiae in which the peripheral iris is permanently adherent to the trabecular meshwork, resulting in chronic angle-closure glaucoma (Fig. 5). Even without the formation of synechiae, repeated subclinical attacks of PACG may damage the trabecular meshwork, giving rise to a secondary open-angle glaucoma (SOAG). Histologically, peripheral anterior synechiae, which may be broad based, are seen (Fig. 5).
Phacomorphic Phacogenic Glaucoma
Phacomorphic angle-closure glaucoma usually is seen in the final stages of lens cortex liquefaction. Sudden osmotically induced lens swelling displaces the iris anteriorly, inducing pupillary block. To a more modest degree, the lens probably plays a contributory role in inducing pupillary block in most cases of PACG. Occasionally, a more gradual chronic angle closure with peripheral anterior synechiae formation can result from lens-induced anterior displacement of the iris. Depending on the asymmetry of cataract formation in a given patient, there may be a significant difference in the anterior chamber depth when each eye is compared in phacomorphic glaucoma.
Phacomorphic Glaucoma Secondary to Lens Subluxation or Dislocation
In disorders of lens subluxation and dislocation, an abnormally mobile lens may shift position, block the pupil, and precipitate angle closure. Lens subluxation or dislocation may result from several causes. Blunt trauma may rupture zonules resulting in phacodenesis, subluxation, or frank dislocation of the lens. As shown in Table 4, several ocular conditions and systemic syndromes are associated with abnormal lens mobility.
Table 4. Ocular and Systemic Conditions Associated with Abnormal Lens Mobility | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||
Of particular importance to the clinician is the significant incidence of lens subluxation in pseudoexfoliation (PXE) syndrome. Significant angle closure may occur in some patients with the syndrome. Nevertheless, individuals with PXE may also exhibit extremely elevated IOP in the absence of angle closure.59 An occludable angle has been reported in 9.3% of PXE patients.60 The small lens in the Weill-Marchesani syndrome may dislocate into the anterior chamber, causing an unusual inverse pupillary block configuration.
Some disorders associated with increased lens mobility may be life threatening: Marfan syndrome is associated with aortic root dilation and aortic dissection, homocystinuria may lead to thromboembolic events and death due to anesthetic complications,61,62,63,64,65 and traumatic lens dislocation may occur as a result of physical abuse and the patient may have associated life-threatening injuries.
Posterior Synechiae–induced Angle-closure Glaucoma
Posterior synechiae usually are inflammatory adhesions between the iris and the lens. Less commonly, such adhesions may form between the iris and vitreous face (aphakic pupillary block) or between the iris and an intraocular lens (pseudophakic pupillary block). All such glaucomas result in iris bombé secondary to these adhesions preventing the passage of aqueous from the posterior to the anterior chamber. All are treated initially by pupillary dilatation to try to break adhesions. If pharmacologic pupillary dilatation fails, laser iridotomy or laser pupillary mydriasis may be required.
Ciliary Block (Malignant) Glaucoma
In ciliary block glaucoma, the lens or vitreous face becomes incarcerated in the ciliary ring, forcing misdirection of aqueous into the vitreous compartment. A cycle of increasing compression of the lens or vitreous face into the ciliary ring and anterior iris displacement, followed by increasing misdirection of aqueous into the vitreous compartment, is established.66,67 Ultrasound biomicroscopy has confirmed the pathophysiology of this entity.68,69,70 Changes or abnormalities in vitreous permeability also may play some role in its pathogenesis.71
Ciliary block glaucoma is a dreaded complication of cataract extraction, iridectomy, filtration surgery, and glaucoma seton implant placement, particularly in patients with a history of chronic angle-closure glaucoma, although spontaneous attacks have been reported.72,73,74 Its onset may follow shortly after surgery or occur after many years.75 Malignant glaucoma has resulted from laser suture lysis after filtration surgery76,77 and yttrium aluminium garnet (YAG) laser posterior capsulotomy after cataract surgery.78 Initially, it was hoped that the avoidance of traditional surgical iridectomy through the use of laser iridotomy would prevent malignant glaucoma associated with PACG. Nevertheless, unilateral and even bilateral attacks have been reported after laser iridotomy.79,80,81 An unusual form of malignant glaucoma has accompanied keratomycotic infections.82,83,84
Treatment of malignant glaucoma is directed at providing access to the anterior chamber for aqueous trapped behind the lens within the vitreous. Such therapy includes cycloplegia, hyperosmolar agents, and vitreous face disruption. YAG laser capsulotomy or disruption of the vitreous face with the YAG laser may be attempted. Pars plana vitrectomy may be helpful if less invasive measures are unsuccessful.85,86,87
Neovascular Glaucoma (Rubeosis Iridis)
Neovascular glaucoma is characterized by the proliferation of a fibrovascular membrane on the anterior iris and onto the trabecular meshwork (Fig. 7). In the initial stages, neovascular glaucoma is a SOAG. As the sheet of tissue proliferates over the trabecular meshwork surface, myofibroblasts within this fibrovascular membrane contract, drawing the iris into contact with the trabeculum and closing the filtration angle through the creation of peripheral anterior synechiae.88
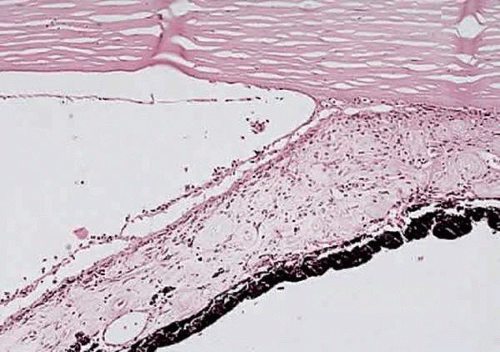 Figure 7. Neovascularization in the anterior chamber angle region, with formation of a secondary “pseudoangle” anterior to a peripheral anterior synechia. (H&E, 33×) |
In a review of 208 patients with neovascular glaucoma, Brown and associates89 found retinal venous obstructive disease in 36.1%, diabetic retinopathy in 32.2%, and carotid artery obstructive disease in 12.9%. They concluded that 97% of involved eyes that were studied demonstrated extensive retinal ischemia. In such cases, the ischemic retina is believed to produce a vasoproliferative substance that stimulates and supports vascular proliferation. Vascular endothelial growth factor (VEGF) has been shown to be upregulated in such ischemic eyes and has been found to be a key mediator of intraocular neovascularization.90,91,92,93 Additionally, increased levels of VEGF are found in the aqueous humor of patients with neovascular glaucoma.94
The fragile vessels produced by neovascularization are prone to bleed, creating a source of spontaneous hyphema and compounding the secondary glaucoma. Because of its association with iris neovascularization and secondary hyphema, retinoblastoma must be excluded in any child with “spontaneous” hyphema.95,96 Other diagnoses to be considered in a child with spontaneous hyphema include child abuse, medulloepithelioma, iris juvenile xanthogranuloma, pseudogliomas, and blood dyscrasia.97,98,99,100,101,102,103
Iridocorneal Endothelial Syndrome
ICE syndrome is a disorder of abnormal endothelial cell proliferation and encompasses and unifies the disorders previously categorized as essential iris atrophy, iris nevus (Cogan-Reese) syndrome, and Chandler syndrome.104,105,106,107,108 However, certain patients may exhibit one or more features of a specific entity, including iris holes, endothelial dystrophy, iris surface nodules, and corectopia. There is enough overlap between these three entities that they seem to represent different manifestations of the same or very similar underlying abnormalities.104,105,106,107,108 For clarification, each entity will be described in its classic form; however, a given patient may display elements of more than one of these.
Essential iris atrophy usually is unilateral and most often affects women in the third decade of life. The initial clinical finding is the formation of a peripheral anterior synechia that distorts the pupil in the direction of the synechia. There is progressive pupillary distortion, and ectropion uveae develops. Histologically, the iris stroma is atrophic. Characteristically, full-thickness iris holes involving the pigment epithelium develop in the quadrant opposite the distorted pupil. The etiology of the iris holes is not known. Endothelialization of the iris surface and filtration angle is a characteristic finding. The endothelium then deposits a new basement membrane beneath the original endothelium and Descemet’s membrane.109 Iris nodules may appear late in the disorder and are a clinical marker for iris endothelialization. They display a progressive change in color from initially yellow to dark brown. Peripheral anterior synechia formation progresses circumferentially, closing the filtration angle and resulting in intractable glaucoma.
Chandler syndrome is almost always unilateral. The glaucoma is usually mild; however, poor endothelial function results in corneal edema even with modest pressure elevation. Histologically, endothelialization of the anterior chamber angle and anterior iris may be present. Iris surface abnormalities and peripheral anterior synechiae are least prominent in this syndrome. Stromal thinning is limited, and holes are rare.
The iris nevus syndrome, like the other components of the ICE syndrome, most often is unilateral and is most often seen in women. Commonly described features of the iris nevus syndrome include peripheral anterior synechiae and associated iris stromal atrophy, a matted appearance to the iris stroma accompanied by a whorl-like iris surface displaying loss of crypts, and the presence of fine iris nodules.110,111 Other associated findings include ectropion uveae, heterochromia, and secondary glaucoma. Histologically, the iris surface contains a diffuse nevus and is covered by an endothelial proliferation and ectopic Descemet’s membrane that also covers the anterior chamber angle.
Table 5 compares Axenfeld-Rieger and ICE syndromes and posterior polymorphous dystrophy. Posterior polymorphous dystrophy may show characteristics similar to the ICE syndrome such as endothelial abnormalities on specular microscopy, corneal edema, iridocorneal adhesions, endothelialization of the anterior chamber angle, and glaucoma. The corneal endothelium in posterior polymorphous dystrophy, however, displays epithelial-like characteristics in contrast to the ICE syndrome.112 Nevertheless, some authors also have suggested epithelial characteristics for the cells in Chandler syndrome.113,114 Posterior polymorphous dystrophy also differs from the ICE syndrome in that the former usually is familial and bilateral and tends not to be progressive.112
Table 5. Distinctions among Axenfeld-Rieger and Iridocorneal Endothelial Syndromes and Posterior Polymorphous Dystrophy | ||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||
Table 5 also provides a possible differentiation of Axenfeld-Rieger and ICE syndromes and posterior polymorphous dystrophy on the basis of the hypothetical underlying abnormality in neural crest cell embryology. Viewed from this perspective, Axenfeld-Rieger syndrome would be related to abnormal neural crest cell migration, ICE syndrome to abnormal crest cell proliferation, and posterior polymorphous dystrophy to abnormal crest cell terminal induction or differentiation. Nevertheless, the specific causes for the abnormal behavior of corneal endothelium present in these syndromes have not been established with certainty. Alvarado and associates115,116,117,118 have suggested that herpes simplex virus infection plays a causative role in the pathogenesis of the ICE syndrome.
Epithelial Downgrowth
Epithelial downgrowth is an uncommon complication of anterior segment surgery. Extensive review of anterior segment cases at the Massachusetts Eye and Ear Infirmary estimated the incidence at 0.06% to 0.08%.119,120 The most common presenting complaints are decreased vision, red eye, and pain. Epithelial downgrowth is probably more common after keratoplasty (0.270%) than after cataract surgery (0.091% to 0.110%).121 It is a dreaded complication of anterior segment surgery with a poor visual prognosis.
Poor wound apposition, fistulas, postoperative hypotony, and nonspecific postoperative complications such as inflammation and hemorrhage are all thought to contribute to the establishment of an epithelial downgrowth.119,120,121,122,123,124,125,126,127,128,129 Sassani and others130,131,132,133 confirmed the importance of healthy endothelium in inhibiting epithelial migration, thereby acting as a defense against epithelial downgrowth.
Typically, epithelial downgrowth presents as a horizontally oriented area of endothelial haze that progressively migrates inferiorly on the posterior corneal surface. This finding may be accompanied by chronic inflammation and ocular hypotony. As the downgrowth progresses, intractable glaucoma may develop. Corneal striae and stromal vascularization may be seen overlying the area of corneal involvement. Epithelium may proliferate on the anterior iris before it is visible elsewhere,123 and eventually, iris surface architecture effacement is seen. Histologically, a multilayered epithelial sheet, which often has characteristics suggesting a conjunctival origin, is seen to proliferate on the posterior cornea, angle structures, and iris surface, and it may even involve the vitreous face and ciliary body.124,125,126,127,128
There can be several mechanisms for the glaucoma in epithelial downgrowth. Desquamating epithelial cells may plug the trabecular meshwork, resulting in SOAG. If the epithelial sheet causes posterior synechiae, pupillary block angle-closure glaucoma can be produced. Ultimately, secondary angle closure without pupillary block results from progressive synechial closure of the filtering angle by the proliferating epithelial sheet.120
Specular microscopy can be of assistance in the diagnosis of epithelial downgrowth,134,135 and laser photocoagulation of the iris surface can be helpful in delineating the extent of epithelial membrane proliferation. Cytologic examination of aqueous or vitreous fluids from aspirates or of scrapings from the corneal endothelial surface or from the iris surface is confirmatory. The clinical progression of epithelial downgrowth to intractable glaucoma may be gradual, although inexorable. The clinical course of the patient must be weighed against the radical therapy usually required to treat the disorder.
Stromal Ingrowth
Stromal ingrowth most frequently is seen after failed corneal transplants;136,137 however, it may follow other surgical procedures, such as cataract surgery, especially if they have been complicated by vitreous loss and incarceration.138,139 Although many of these membranes represent direct proliferation of keratocytes through a dehiscence in Descemet’s membrane, some retrocorneal fibrous membranes may represent fibrous metaplasia of corneal endothelium.140,141 Histologically, a fibrous membrane is seen to extend from a corneal wound to proliferate over the posterior cornea. Peripheral anterior synechiae result in SACG.
Endothelialization of the Anterior Chamber Angle
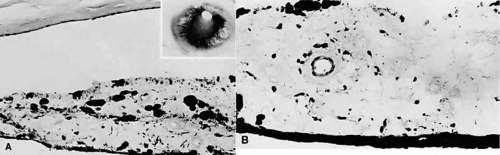
Endothelialization of the anterior chamber angle is seen on histologic examination in 20% of enucleated eyes.142 Endothelial proliferation extends over anterior segment structures, including the iris and the anterior chamber angle (or pseudoangle in the presence of peripheral anterior synechiae, which are noted frequently) (Fig. 8). Endothelialization may be found accompanying rubeosis iridis.143
Postoperative Surgical Complications
Postoperative “flat” anterior chamber is seen in various surgical procedures, particularly those performed for glaucoma, in which overfiltration and wound leaks are common causes. Such overfiltration or wound leaks are particularly likely to occur if adjunctive antimetabolites are used. The advent of viscoelastic agents and releasable sutures has decreased the frequency of these complications.144,145,146,147,148,149 Persistent hypotony secondary to aqueous loss also may lead to choroidal detachment and effusions, which can further contribute to anterior chamber shallowing.150 Persistent flat anterior chamber may result in peripheral anterior synechiae that may be very broad. Suprachoroidal hemorrhage is another feared complication of intraocular surgery. Choroidal hemorrhage also may cause anterior rotation of the ciliary body and forward movement of the iris–lens diaphragm, resulting in SACG. Ocular implants, such as seton devices and scleral buckles, may also cause forward movement of the iris diaphragm and anterior rotation of the ciliary processes, resulting in angle closure.
Iris and Ciliary Body Cysts
Cysts of the iris and anterior ciliary body, particularly if multiple, may displace the iris–lens diaphragm anteriorly, resulting in angle closure.151 Angle closure in the case of multiple cysts may be acute. The cysts may be idiopathic or acquired, such as those associated with trauma or late syphilitic interstitial keratitis.152,153,154 Unlike acquired cysts, primary cysts tend to be stationary. Ultrasound biomicroscopy has been demonstrated to be useful in the evaluation of cystic lesions of the iris.155
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree