51
Pathologic Myopia
Mario Stirpe  Guido Ripandelli
Guido Ripandelli
High myopia is generally defined as a myopia of −6 diopters or more (with the corresponding axial length usually exceeding 26 mm) (1).
Pathologic myopia on the other hand is defined by posterior chorioretinal changes caused by the excessive elongation of the eye; this condition generally occurs in eyes with an axial length over 28 mm.
It has been observed that after macular hole (MH) formation the retina does not detach in emmetropic eyes while it detaches in myopic eyes. It has been hypothesized that the vitreous cortex plays a role in MH formation in both emmetropic and myopic eyes, while a retinal detachment (RD) in myopic eyes can be related to pigment epithelial atrophy (2, 3). Surgical observations in myopic eyes with RD due to MH (RDMH eyes) showed a retinal reattachment after the removal of epiretinal tissue, suggesting another mechanism (4–6). In any case it seems probable that either vitreous tractions or choroidal atrophy may play the prominent role, according to the degree of the myopia (7).
Several factors are involved in the evolution of pathologic myopia and different surgical procedure can be used to repair a RD with MH. In choosing the procedure, vitreous changes, chorioretinal alterations, and the presence of a staphyloma have to be taken into account.
In an histological study on 369 eyes with high myopia, Green and Grossnicklaus found a posterior staphyloma in 33% of the eyes (8). The posterior staphyloma correlated with axial elongation of the eyes, which gives an egg-shaped configuration to the eye. The posterior elongation of eyes in pathologic myopia creates thinning of the posterior sclera, which may be found to be nearly absent during surgery. Posterior chorioretinal degeneration is the most common clinical finding in eyes with pathologic myopia; retinal pigment epithelium atrophy is accompanied by loss of choroid. Green and Grossnicklaus reported a curious form of retinal alteration that they called “stretch schisis.” This condition results from retinal vessels that do not lengthen as much as the underlying neurosensory retina, resulting in a schisis-like configuration. The authors did not find evidence that vitreoretinal traction plays a role in the pathogenesis of this condition.
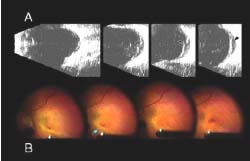
Vitreous changes that are involved in the development of pathological modifications of the posterior retina in myopic eyes include posterior vitreous detachment (PVD) and posterior vitreous schisis (PVS). True PVD is defined as a separation of the posterior vitreous cortex from the internal limiting lamina of the retina. MH that occurs in eyes with high but not excessive myopia during a PVD may be due to incomplete dissection of posterior vitreoretinal adhesions by liquefied vitreous that has penetrated into the retrovitreal space (9). In this situation, the subsequent RD is generally characterized by a wide extension to the periphery especially in the inferior quadrants (10). During biomicroscopical examination of RD with MH associated with PVD, sometimes firm localized vitreoretinal tractions can be observed (Fig. 51-1A), but in many cases there is no evidence of posterior vitreoretinal adhesions (Fig. 51-1B). It is possible that weak remaining posterior adhesions, not necessarily localized to the macular area, can cause anteroposterior traction that is sometimes difficult to see, despite a careful examination by biomicroscopy and ultrasonography. This may explain why selected RDs with MH can be reattached using an intravitreal gas injection that breaks the remaining vitreoretinal adhesions (11).
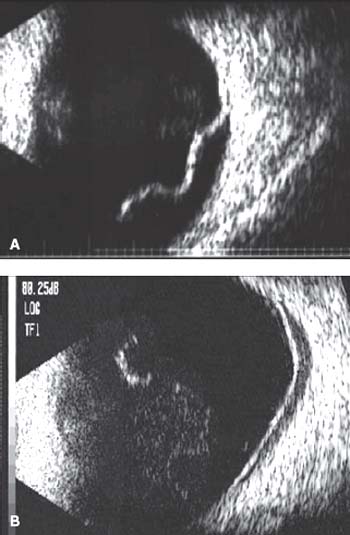
Figure 51-1. A: Retinal detachment with macular hole associated with posterior vitreous detachment. B-scan ultrasonography: persistent anteroposterior tractions on the posterior retina. B: Retinal detachment with macular hole associated with posterior vitreous detachment. B-scan ultrasonography: no evidence of posterior vitreoretinal tractions.
PVS is defined as an anomalous form of vitreoretinal separation characterized by a forward displacement of the anterior portion of the posterior vitreous cortex leaving part of the posterior portion of the vitreous cortex still attached to the retina. In eyes with excessive myopia and a pronounced posterior staphyloma, the space just above the posterior staphyloma is frequently the site of vitreous liquefaction, causing PVS.
Tolentino, Schepens, and Freeman clearly described a posterior vitreous lacuna containing liquefied vitreous in high myopic eyes and concluded: “The posterior limit of the lacuna may be absent if liquefaction has involved the entire thickness of the vitreous cortex. In this case, part of the inner surface of the retina then became the posterior wall of the lacuna” (12). After the introduction of optical coherence tomography (OCT) (13) we recognized that when there is a vitreous schisis, a posterior vitreous wall of the lacuna always exists; it is sometimes difficult to detect by biomicroscopic examination, due to its thinness and transparency. This layer of vitreous tissue is, in a number of cases, the cause of tangential tractions (Fig. 51-2) causing posterior RD with or without MH and posterior retinoschisis. RD resulting from this change is generally limited to the area of posterior staphyloma and the subretinal fluid is really liquefied vitreous. Sometimes the posterior layer of the vitreous lacuna partially detaches creating anteroposterior traction (Fig. 51-3); occasionally a complete separation can occur.

Figure 51-2. Optical coherence tomography scans show a shallow retinal detachment with disruption of the neuroretinal layers, consistent with retinoschisis. A hyperreflective band, strictly adherent to the inner retinal surface and exerting tangential tractions, is detected.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


