Otosclerosis
Brandon Isaacson
Joe Walter Kutz Jr.
Peter S. Roland
Otosclerosis (OS) is a fibrous osteodystrophy of the human otic capsule. Its clinical manifestations are primarily conductive hearing loss (CHL), although sensorineural hearing loss (SNHL) and mixed hearing loss (MHL) can also occur. The disease process causes abnormal resorption and deposition of bone. OS is noted clinically in 1% of the Caucasian population; it is transmitted in an autosomal dominant fashion but with incomplete penetrance. Females appear to be affected twice as often as males (1).
In 1873, Schwartze described a reddish hue medial to an intact tympanic membrane (TM), which was secondary to the increased vascularity of the cochlear promontory in active OS lesions (the phase known as otospongiosis). This finding is named after him and is known as Schwartze sign. It is seen in 10% of patients with OS. In 1881, von Troltsch noted abnormalities of the middle ear mucosa in this disease and was the first to use the term OS. In 1893, Politzer described OS as a primary disease of the otic capsule, rather than a condition related to previous episodes of inflammatory ear disease, as originally thought (2).
The clinical entity of OS was further described by Bezold in 1908, when he discussed its historical, physical, and audiometric findings. In 1912, Siebenmann discussed the possibility of OS causing SNHL. Since that time, numerous etiologies of OS have been suggested, including hereditary, endocrine, biochemical, metabolic, infectious (e.g., measles), traumatic, vascular, and even autoimmune factors (3). In fact, Lopez-Gonzalez and Delgado (4) suggested that oral vaccination with type II collagen may mitigate the autoimmune reaction in those susceptible to OS through hyposensitization. It is also possible that interplay of these different factors exist and vary from individual to individual, while causing the same pathologic and clinical findings. In other words, OS may be the common, final pathway of a clinically and genetically heterogeneous group of disorders (5).
EMBRYOLOGY
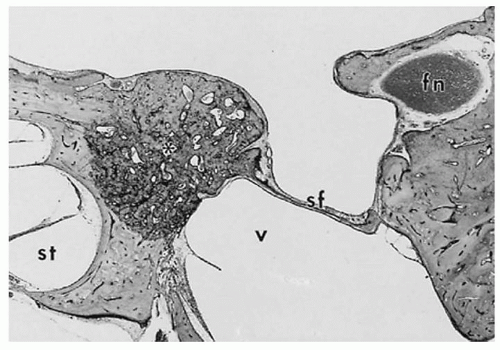
The maturation of the bony labyrinth plays a role in the pathogenesis of OS. The otic capsule arises from mesenchyme surrounding the otic vesicle at 4 weeks of embryologic development. At 8 weeks, the cartilaginous framework is initiated. At 16 weeks, endochondral osseous replacement of this framework begins in 14 identifiable centers. In some people, complete bony replacement does not occur and leaves cartilage in certain locations. One of these regions, the fissula ante fenestram, is anterior to the oval window (OW) and is usually the last area of endochondral bone formation in the labyrinth. According to temporal bone studies, this region is affected in 80% to 90% of patients with OS (6). In 1985, Schuknecht and Barber (7) reported other areas of predilection for otosclerotic lesions, such as the border of the round window (RW), the apical medial wall of the cochlea, the area posterior to the cochlear aqueduct, the region adjacent to the semicircular canals, and the stapes footplate itself (which is derived from otic capsule, as opposed to the superstructure, which is a branchial arch derivative).
HISTOLOGY
There are three forms of otosclerotic lesions: otospongiosis (early phase), transitional phase, and OS (late phase). The early, active phase lesions consist of histiocytes, osteoblasts, and the most active cell group, the osteocytes. The osteocytes resorb bone around preexisting blood vessels, which causes widening of the vascular channels and dilation of the microcirculation. Otoscopic or microscopic exam can reveal the reddish hue caused by these lesions (Schwartze sign if seen on clinical examination). As osteocytes become more involved, these areas grow rich in amorphous ground substance and deficient in mature collagen, resulting in
formation of new spongy bone. With hematoxylin-eosin (H&E) staining, this new spongy bone appears densely blue. This was described in 1914 by Manasse and is known as the blue mantles of Manasse. Interestingly, mantles are found in up to 20% of normal temporal bones. On electron microscopy, the foci of perivascular bony invasion coalesce as the lesions enlarge within the otic capsule (7).
formation of new spongy bone. With hematoxylin-eosin (H&E) staining, this new spongy bone appears densely blue. This was described in 1914 by Manasse and is known as the blue mantles of Manasse. Interestingly, mantles are found in up to 20% of normal temporal bones. On electron microscopy, the foci of perivascular bony invasion coalesce as the lesions enlarge within the otic capsule (7).
The predominant finding in the late phase of OS is the formation of sclerotic, dense bone in areas of previous osseous resorption. The vascular spaces that were once dilated are narrowed due to bony deposition. Within each temporal bone containing OS, lesions can be found in early, transitional, and late phases, although the overall histologic status of the developing lesions is fairly uniform. Although OS begins in endochondral bone, as the spongiosis and sclerosis continue, the endosteal and periosteal layers also become involved (8).
BASIC SCIENCE
A number of mechanisms including autoimmune, genetic, and infectious have all been described as potential causative factors for the development of OS. Definitive evidence for an autoimmune etiology for OS is currently lacking. Conflicting evidence exists for increased levels of type II and IX collagen antibodies in patients with OS. Animal models of type II collagen autoimmunity were found to have lesions similar to OS in contrast to another nearly identical study where autoimmune mice were found to have no lesions (5).
OS has a significant genetic component with seven distinct loci reported to date. Autosomal dominant transmission with incomplete penetrance is the predominant mode of inheritance. The OS loci identified include genes that regulate growth regulation, intercellular communication; cartilage, bone, and collagen homeostasis and metabolism. Additional work is needed to identify potential candidate genes involved in the pathogenesis of OS (9).
A number of findings point toward a viral etiology for OS. Measles antigens and RNA, as well as nucleocapsid structures identical to measles virus have all been identified in otosclerotic lesions. Increased levels of measles-specific IgG have also been detected in the perilymph of OS patients undergoing stapedectomy. It is not yet certain that the measles virus is involved in the development of OS, and the pathogenesis has yet to be elucidated (9).
A more in-depth understanding of the molecular biology of bone remodeling has shed additional light on the pathogenesis of OS. The otic capsule is unique compared to the rest of the skeleton in that after the age of one, no further osseous remodeling occurs. Bone remodeling is rigorously regulated via a balance between the cytokines and receptor: osteoprotegerin (OPG), receptor activator of nuclear factor kB (RANK), and RANK ligand (RANKL). RANKL is present on the surface of osteoblasts and binds to RANK receptors on the surface of osteoclast precursor cells, which results in osteoclast differentiation, activation, and subsequent bone remodeling. Soluble OPG competes with RANKL in binding to the RANK receptor on the surface of osteoclast precursor cells and results in decreased bone remodeling. A fine balance exists between RANKL and OPG, which regulates skeletal remodeling including the otic capsule. High levels of OPG (reduced predilection for bone turnover) have been detected in the inner ear and are secreted into perilymph by type I fibrocytes located within the spiral ligament. It has been postulated that genetic, infectious, and autoimmune mechanisms likely alter this pathway, which eventually results in OS (9).
PATHOPHYSIOLOGY
The areas of OS involvement dictate the clinical presentation. The most common type involves the stapes and accounts for those cases in which CHL is the presenting symptom. The CHL is due to fixation of the stapes footplate, usually beginning at the fissula ante fenestram (Fig. 154.1). Progressive involvement of the footplate can create a thick focus of OS that fills the OW niche (obliterative OS) (5).
If OS involves only the footplate and spares the annular ligament, minimal fixation may occur. Such a thickened footplate is called a biscuit footplate. Because of minimal fixation, biscuit footplates can become mobilized inadvertently during a stapes procedure, placing the patient at a higher risk of postoperative SNHL. The RW is involved in 30% of all clinical cases of OS; complete closure of this niche is uncommon (10).
SNHL as a result of OS is an ongoing controversial subject. Some patients with OS have a greater amount of SNHL than expected considering their age and history of noise exposure. The mechanism for the SNHL is possibly the liberation of toxic metabolites into the inner ear with resultant injury to neuroepithelium, vascular compromise, or direct extension of lesions into the cochlea, causing
disruption of electrolytes and changes in basilar membrane mechanics. SNHL is usually associated with significant stapedial OS, although some otologists contend that isolated pure SNHL can be seen without associated CHL. The latter presentation is also known as cochlear OS (11).
disruption of electrolytes and changes in basilar membrane mechanics. SNHL is usually associated with significant stapedial OS, although some otologists contend that isolated pure SNHL can be seen without associated CHL. The latter presentation is also known as cochlear OS (11).
Shambaugh (11) has suggested seven criteria to identify patients suffering from SNHL due to OS:
Schwartze sign in either ear
Family history of OS
Unilateral CHL consistent with OS and bilateral, symmetric SNHL
Audiogram with a flat or “cookie-bite” curve with excellent discrimination
Progressive pure cochlear loss beginning at the usual age of onset for OS
Computed tomography (CT) scan showing demineralization of the cochlea typical for OS
Stapedial reflex demonstrating the biphasic “on-off effect” seen before stapedial fixation
Vestibular symptoms occur in up to 40% of patients with OS. OS lesions have been described in the lateral semicircular canal during fenestration procedures (which have been replaced by the stapedectomy/stapedotomy). The vestibular symptoms are usually not severe, but objective evidence can be obtained with electronystagmography testing. Non-Ménière-type vertigo or disequilibrium associated with OS has been termed OS inner ear syndrome. It is important to differentiate this disorder from Ménière disease or superior semicircular canal dehiscence (SSCD). Ménière disease is an absolute contraindication for stapedectomy/stapedotomy. When the endolymphatic space is dilated (endolymphatic hydrops), the saccule may be enlarged to the point that it adheres to the undersurface of the stapes footplate. A stapes procedure can injure the saccule and result in profound SNHL. The distinction between OS inner ear syndrome and other causes of dizziness is based on differences in clinical presentation. Rarely does the inner ear syndrome of OS cause well-defined episodes of severe rotational vertigo, nausea, vomiting, and fluctuating SNHL. Dizziness in OS inner ear syndrome is milder but more persistent; low-frequency SNHL is generally not present (12).
In 2004, Mikulec et al. (13) reported on eight patients with presumed OS/unilateral CHL that did not improve after a stapes procedure. These patients were ultimately found to have SSCD. In contrast to typical SSCD patients, these patients had only CHL and no vestibular symptoms. One should keep this entity in mind, especially in a patient with CHL and pressure or sound-induced vertiginous symptoms. Intact acoustic reflexes in the setting of CHL should prompt further imaging to evaluate for an inner ear third window. SSCD, posterior and lateral semicircular canal dehiscence, enlarged vestibular aqueduct, and modiolar deficiencies (i.e., X-linked stapes gusher) can all present with a CHL or MHL with intact acoustic reflexes (13).
EPIDEMIOLOGY
OS is transmitted in an autosomal dominant fashion with incomplete penetrance (25% to 40%). The degree of penetrance is related to the distribution of lesions in the otic capsule. Some lesions are located where they cannot cause clinical symptoms. About 10% of Caucasians have histologic findings of OS. However, of those with histologic changes, only 12% have clinical symptoms; thus, overall, this represents about 1% of the Caucasian population. In the Japanese and South American populations, the incidence is 50% of that in Caucasians. The African American population has fewer cases of OS; only 1% demonstrate histologic findings of the disease. In all races, when one ear is affected, the contralateral ear shows histologic involvement 80% of the time. Generally, the lesions occur in similar anatomic locations and at similar histologic phases. The age at which symptoms become apparent is variable due to the insidious progression of hearing loss, but hearing loss often begins between the ages of 15 and 45 years. The average age at presentation is 33 years (14).
About 60% of patients with clinical OS report a family history of this condition. The remaining 40%, as suggested by Morrison and Bundey (14), make up a collection of cases that fall into one of the following categories:
Autosomal dominant inherited cases with failure of penetrance in other family members
Phenocopies (an individual expressing a trait that is environmentally as opposed to genetically induced)
New mutations
Those rare cases transmitted by alternate modes of inheritance (i.e., autosomal recessive)
OS has been reported to advance more rapidly in females than males, although no difference has been noted in age at onset. A recent study by Clayton et al. (15) examined the relationship in elderly women between osteoporosis and OS; both diseases show some similarities, including an association with the COL1A1 gene. The study showed that a much higher percentage of women with OS also had osteoporosis as compared with a similar aged group with only presbycusis (P < 0.007). Juvenile OS may progress more rapidly than the adult form. Hormonal factors may play a role; some females with OS appear to have their condition worsen during pregnancy. Estrogen receptors have been noted in the OS plaques. However, more recent data minimize the association between pregnancy and worsening of OS (9).
HISTORY AND PHYSICAL EXAMINATION
Patients with OS usually present with a slowly progressive hearing loss over a period of years. Patients may describe hearing speech more easily in noisy situations. The CHL improves the signal to noise ratio by subduing background noise (paracusis of Willis). Tinnitus is present in 75% of patients. A complete head and neck examination
is performed to rule out concurrent otolaryngologic abnormalities. Otomicroscopic examination with pneumatic insufflations is done of the external auditory canal (EAC) and TM to asses for the presence of a middle ear effusion or mass, cholesteatoma, or TM retraction. The physical appearance of the TM is normal in most patients with OS. A Schwartze sign (a red to pink appearance of the cochlear promontory occasionally seen in active OS through the TM) may be present.
is performed to rule out concurrent otolaryngologic abnormalities. Otomicroscopic examination with pneumatic insufflations is done of the external auditory canal (EAC) and TM to asses for the presence of a middle ear effusion or mass, cholesteatoma, or TM retraction. The physical appearance of the TM is normal in most patients with OS. A Schwartze sign (a red to pink appearance of the cochlear promontory occasionally seen in active OS through the TM) may be present.
The primary purpose of performing a tuning fork exam is to confirm the findings of the audiogram. The Rinne test should demonstrate bone conduction to be better than air conduction (Rinne negative) in patients contemplating a stapes procedure. In the initial phases of the disease, CHL may be limited to the 256-Hz tuning fork. As footplate fixation progresses, the 512- and 1,024-Hz tuning forks will “reverse” as well. The amount of air-bone gap required to reverse the tuning forks are about 10 to 15 dB for the 256-Hz tuning fork and 20 to 25 dB for the 512-Hz tuning fork. The Weber test should lateralize to the ear with the greater degree of CHL, although this test is also affected by concurrent SNHL. If the tuning fork exam does not correlate with the audiogram, repeat testing is recommended since inadequate masking may falsely lead the clinician to believe a conductive loss is present in the setting of anacusis (16).
AUDIOLOGIC TESTING
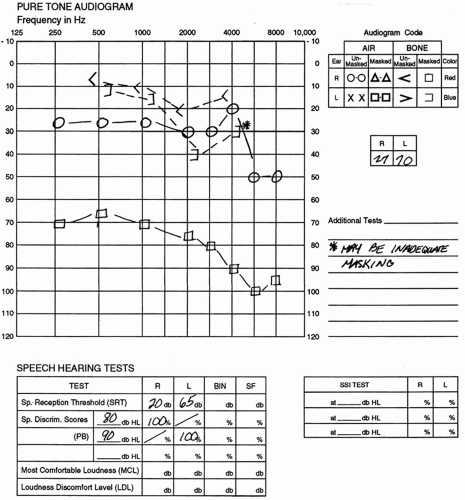
The main objective measurement in OS is the audiogram (Fig. 154.2). On the audiogram, OS is seen as a widening air-bone gap that usually begins in the low frequencies.
Variable degrees of SNHL may also be present. Bone conduction may show a 20-dB loss at 2,000 Hz and a 5-dB loss at 500 and 4,000 Hz. Such an apparent depression of bone conduction at 2,000 Hz is known as Carhart notch, which is most commonly seen in OS but can be seen in other types of CHL. This notch is an artifact of the audiogram and disappears after a stapedectomy. It is secondary to stapes fixation and a resultant change in the resonance of the otic capsule (17).
Word recognition scores are usually excellent in patients with OS even in the later stages of the disease process. Impedance can show reduced TM compliance (type A or As). Stapedial reflexes are characteristically absent in the setting of CHL. Intact stapedial reflexes can occasionally be observed in the earliest stages of OS depending on the degree of fixation. With early stapes fixation, a characteristic abnormal decrease in impedance may be noted at the onset and offset of the eliciting signal. This is the on-off effect of OS. The presence of stapedial reflexes with a significant CHL warrants evaluation for an inner ear third window (i.e., SSCD). Vestibular testing should be included when dizziness is present. Although there are not characteristic findings for OS inner ear syndrome, findings or a clinical history suggestive of SSCD or Ménière disease will alter treatment planning (17).
High-resolution CT scans can help identify or confirm patients with OS. Radiolucent areas in and around the cochlea are noted early in the course of the disease, creating the “halo sign.” Diffuse sclerosis is found in mature cases (Fig. 154.3). Negative results on the CT scan are not diagnostic because some patients have disease below the capabilities of scanning protocols. The CT can rule out middle ear masses, vascular anomalies, or facial nerve abnormalities but is not an essential part of the workup. These scans can also assess the ossicular chain in addition to the osseous labyrinth (cochlea, semicircular canals) (18).
DIFFERENTIAL DIAGNOSIS
The differential diagnosis should include other causes of CHL or MHL. A history of progressive CHL or MHL in the absence of history of trauma or infection but with the presence of a normal TM limits the possibilities. However, a definitive diagnosis can only be made during exploratory tympanotomy. The most common conditions that mimic OS are those that result in ossicular discontinuity or exert a mass effect on the TM or ossicles. A history of recurrent chronic otitis media suggests an ossicular discontinuity due to incus necrosis. The TM may be normal or thickened or atrophic in cases of chronic infection. The TM in these ears is sometimes abnormally compliant, which can be manifested as a type Ad tympanogram. Fibrous union of the incudostapedial (IS) joint can produce an air-bone gap wider in the high frequencies than in the lower frequencies (16).
Fractures or displacement of the ossicular chain is not uncommon in the setting of temporal bone trauma. Hemotympanum or otorrhea is frequently encountered in the immediate period following the injury. A follow-up examination with audiometry is typically recommended in patients with temporal bone fractures to allow for resolution of hemotympanum and spontaneous healing of TM perforation. In cases of traumatic ossicular chain displacement, a fibrous union often forms with resultant resolution of CHL. Distorted TM surface landmarks occasionally provide evidence of prior temporal bone trauma that has resulted in CHL or MHL. A fracture of the stapes superstructure or incus long process may have a similar audiometric configuration as OS.
Congenital stapedial footplate fixation presents at an earlier age than does juvenile OS. De la Cruz noted in his series that congenital footplate fixation was detectable at age 3, whereas juvenile OS was not detectable until about age 10 (19). In the setting of lateral ossicular chain fixation, the malleus and/or incus become fixed in the epitympanum (usually at the superior malleolar ligament), resulting in immobility of all the ossicles; this can occur congenitally or may be acquired through tympanosclerosis. The entire ossicular chain must be examined with
every exploratory tympanotomy to avoid overlooking this lesion. Tympanosclerosis can mimic OS, but a history of recurrent otitis media or tympanostomy tubes is usually present. In addition, the TM is often thickened with associated myringosclerosis. Persistent middle ear effusion, neoplasms of the middle ear and EAC (such as glomus tumors or facial nerve tumors), and chronic suppurative otitis media with and without cholesteatoma can also cause CHL. Audiometry and physical examination should help make the diagnosis apparent (16).
every exploratory tympanotomy to avoid overlooking this lesion. Tympanosclerosis can mimic OS, but a history of recurrent otitis media or tympanostomy tubes is usually present. In addition, the TM is often thickened with associated myringosclerosis. Persistent middle ear effusion, neoplasms of the middle ear and EAC (such as glomus tumors or facial nerve tumors), and chronic suppurative otitis media with and without cholesteatoma can also cause CHL. Audiometry and physical examination should help make the diagnosis apparent (16).
Paget disease (osteitis deformans) is a disease with diffuse bony involvement that is histologically similar to OS. In contrast to OS, Paget disease begins in the periosteal layer and involves the endochondral bone last. Temporal
bone involvement can produce SNHL, but stapes involvement or fixation rarely occurs (20).
bone involvement can produce SNHL, but stapes involvement or fixation rarely occurs (20).
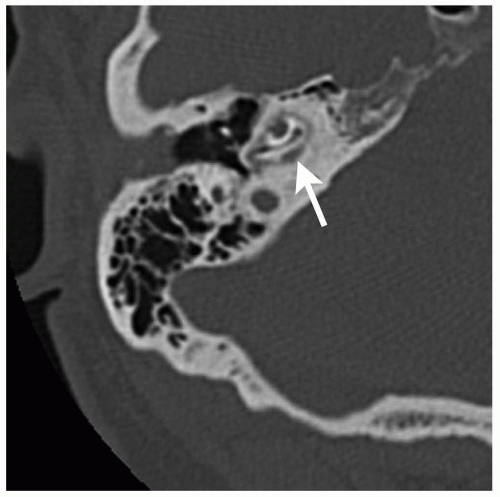 Figure 154.3 High-resolution axial temporal bone CT scan demonstrates extensive OS involving the right cochlea. A classic “halo” sign (arrow) surrounds the cochlea. |
| ||||||||||||||||||||||||||||||||||
Osteogenesis imperfect (van der Hoeve-de-Kleyn syndrome) is an autosomal dominant defect of osteoblast activity resulting in multiple fractures. Stapes fixation and unique blue sclera are also found in 40% to 50% of affected patients. Stapes surgery can be performed in these patients, usually with results similar to those in patients with OS (Table 154.1) (21).
MANAGEMENT
Ninety percent of patients with histologic evidence of OS are asymptomatic; active lesions usually mature without stapedial fixation or cochlear loss. In the symptomatic patient, slowly progressive CHL and SNHL usually begins between the ages of 30 and 50 years with a peak incidence in the 40s (22).The disease may advance more rapidly at times, possibly depending on environmental factors. Periods of progress may be followed by periods of quiescence. The CHL stabilizes at a maximum of 50 to 60 dB.
AMPLIFICATION
Patients with hearing loss secondary to OS should be offered the option of amplification with typical hearing aids as an alternative to observation or surgery. Unilateral or bilateral hearing aids may provide effective treatment. Some patients may not be suitable candidates for surgery, making amplification the only reasonable option. Another option is to use bone conduction hearing aid. A bone anchored hearing aid (BAHA) is another option for patients with CHL or MHL secondary to OS who cannot wear a hearing aid. Two BAHA systems are currently available in the United States (BAHA, Cochlear Corporation; PONTO, Oticon). A BAHA bypasses the ossicular chain and amplifies sound that stimulates the cochlea directly through bone conduction. McLarnon et al. (23) reported that satisfaction levels for three groups of patients receiving a BAHA was highest in patients with congenital aural atresia, followed by patients with OS, and was lowest in patients with single-sided deafness (e.g., acoustic neuroma patients).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree