Ossiculoplasty and Tympanoplasty in Chronic Otitis Media
Saumil N. Merchant
This work was supported in part by research grants from the National Institute on Deafness and Other Communication Disorders of the National Institutes of Health.
Chronic suppurative otitis media (COM) is a chronic inflammatory disease of the middle ear and mastoid that often results in partial or total loss of the tympanic membrane and ossicles, leading to conductive hearing losses that can range in severity up to 60 to 70 dB. Chronic otitis media is a common condition, affecting 0.5% to 30% of any community (1). Therefore a conservative estimate of the number of people in the world suffering from COM is more than 120 million. The mainstay of therapy for COM is surgical, with the main goals being eradication of disease, prevention of recurrence, and preservation or improvement of hearing. Mastoidectomy is designed to eradicate disease in the mastoid and middle ear, whereas tympanoplasty is an operation designed to reconstruct the middle ear hearing mechanism (2). In the United States, more than 70,000 tympanoplasty and mastoidectomy procedures are performed annually (3).
Selection of surgical approaches for COM is discussed in Chapters 9 and 11. Surgery for repair of tympanic membrane perforations is discussed in Chapter 14, and mastoidectomy procedures are described in Chapter 17. This chapter focuses on the rationale for and the surgical techniques used to restore hearing after eradicating disease in the tympanomastoid compartment.
CLASSIFICATION OF TYMPANOPLASTY
The modern era of tympanoplasty was ushered in by Wullstein (4) and Zöllner (5). Subsequently, many other otologic surgeons contributed to the development and refinement of tympanoplasty techniques. Wullstein classified the operations as types I through V, based on the concepts of sound transformation at the oval window and sound protection of the round window. A modified version of Wullstein’s classification is presented and used in this chapter.
Type I
Type I tympanoplasty refers to repair of the tympanic membrane without altering the ossicular system. The procedure includes exploration of the middle ear to inspect and ensure normality of the ossicles. Myringoplasty refers to repair of the tympanic membrane alone without inspection of the ossicular chain.
Type II
Type II tympanoplasty refers to repair of the tympanic membrane and ossicular system with restoration of the lever mechanism, which is a normal function of the malleus and incus. The most common condition leading to type II tympanoplasty is osteitic resorption of the lenticular process of the incus, which is repaired with a bone graft or synthetic prosthesis.
Type III
Type III tympanoplasty restores sound conduction to the oval window by one of the following three types of columella reconstruction: (i) A stapes columella consists of placing the tympanic membrane or graft onto an intact stapes. (ii) A minor columella consists of placing an ossicle graft from the stapes capitulum to the tympanic membrane or manubrium. A synthetic prosthesis of this type is termed a partial ossicular replacement prosthesis (PORP). (iii) A major columella, performed when the stapes crura are missing, consists of an ossicle graft placed from the footplate to the tympanic membrane or manubrium. Such a synthetic prosthesis is termed a total ossicular replacement prosthesis (TORP).
Type IV
In type IV tympanoplasty, the stapes footplate is allowed to remain directly exposed to incoming sound from the ear canal and a tissue graft is placed to acoustically shield the
round window membrane from sound. The air space enclosed between the acoustic shield and the round window is called the cavum minor. The cavum minor is aerated via the eustachian tube.
round window membrane from sound. The air space enclosed between the acoustic shield and the round window is called the cavum minor. The cavum minor is aerated via the eustachian tube.
Type V
The type V operation is used to bypass an ankylosed stapes footplate and is performed as a second-stage procedure after eradication of active disease. There are two subtypes: (i) Type Va tympanoplasty is the original Wullstein type V and consists of fenestration of the lateral semicircular canal to bypass the ankylosed stapes footplate. (ii) A type Vb is similar to a type IV, but the stapes footplate is removed and the oval window is sealed by a tissue graft (6). Type Va procedures are rarely performed, having been largely supplanted by type Vb operations.
PHYSIOLOGIC PRINCIPLES OF TYMPANOPLASTY
The goals of tympanoplasty are to restore sound pressure transformation at the oval window by coupling an intact tympanic membrane with a mobile stapes footplate via an intact or reconstructed ossicular chain and to provide sound protection for the round window membrane by means of a closed, air-containing, mucosa-lined middle ear (4).
In the normal ear, most of the middle ear gain is provided by the area ratio; that is, the tympanic membrane gathers force over its surface and then couples the gathered force to the smaller footplate of the stapes. It is pertinent to note that the mean gain provided by the normal human middle ear is only approximately 20 dB between 250 and 1,000 Hz, and the gain decreases by 6 to 8 dB per octave at frequencies above 1,000 Hz (7). Consequently, a mechanically mobile but suboptimal tympanoplasty combined with adequate middle ear aeration and round window protection can result in no middle ear gain but still produce a relatively good hearing result. For example, a tympanoplasty that gives a middle ear gain of 5 dB but leaves the middle ear aerated and allows round window motion will result in an air-bone gap of only 15 dB.
Because the cochlea responds to a difference in sound pressure between the oval and round windows, it is important to understand how this difference depends on the relative magnitude and phase of the two sound pressures. In the normal ear and after successful tympanoplasty, the magnitude of sound pressure at the oval window is significantly greater than that at the round window, and under these circumstances, differences in phase have little effect on determining the window pressure difference (7). Therefore the goal of tympanoplasty should be to increase the magnitude of sound pressure at the oval window relative to the round window, without regard to phase.
PATHOLOGIC CONSIDERATIONS
A number of pathologic changes can occur in the middle ear and mastoid as a result of COM (8). These tissue responses can compromise sound transmission, leading to conductive hearing loss, and they can also play an important role in determining the success or failure of tympanoplasty. In addition, the host response to ossicular implants and grafts is an important determinant of the long-term efficacy of ossicular reconstruction (9,10). Insight into these pathologic factors can help a surgeon to make more rational decisions regarding selection of cases and surgical techniques to optimize both control of disease and restoration of hearing.
Pathology of Chronic Otitis Media
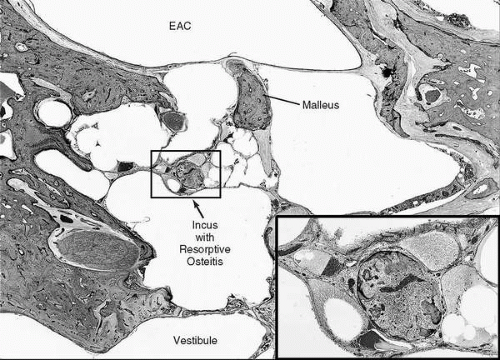
Active COM, both with and without cholesteatoma, may lead to resorptive osteitis of the ossicular chain (Fig. 23.1). The lenticular process of the incus is the most commonly affected part of the chain, leading to discontinuity at the incudostapedial joint or its replacement with a fibrous band. Resorption can also involve the stapes crura, body of incus, and manubrium, in that order of frequency.
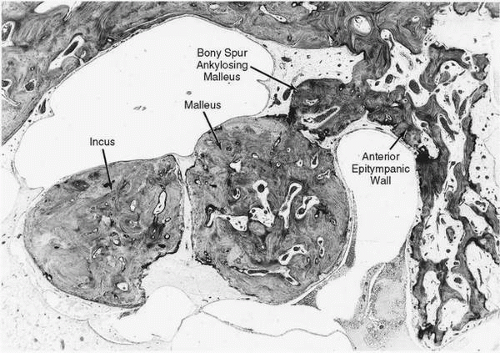
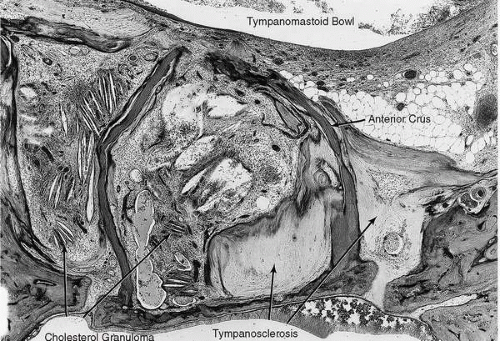
Chronic otitis media may lead to ankylosis or fixation of an ossicle as a result of proliferation of fibrous tissue, deposition of tympanosclerosis, or neoosteogenesis. Tympanosclerotic fixation may involve one, two, or all three ossicles. Common sites of fixation are the malleus head in the epitympanum (Fig. 23.2) and the stapes footplate at the oval window (Fig. 23.3). Ossicular fixation may occur in association with tympanic membrane perforation and ossicular resorption, and failure to recognize fixation may lead to an unsatisfactory surgical result.
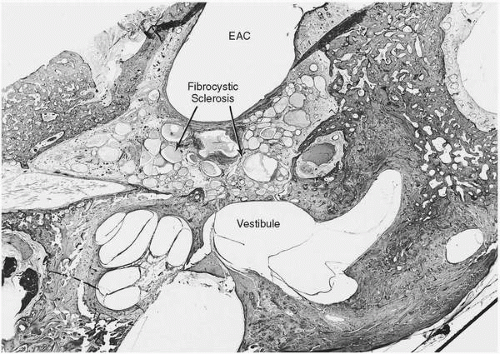
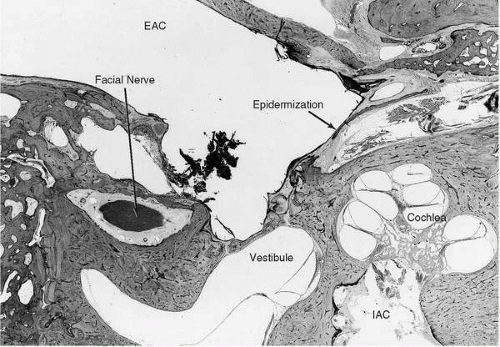
Some cases of healed, inactive COM result in end-stage pathology, characterized by fibrosis and cyst formation (fibrocystic sclerosis), that obliterates large portions of the tympanomastoid compartment (Fig. 23.4). The cystic spaces are lined by mucosal epithelium that has been overrun by proliferation of fibrous tissue. Often there is deposition of new bone in the mastoid antrum and central mastoid cell tract (fibroosseous sclerosis). Another example of inactive COM is epidermization, which refers to keratinizing squamous epithelium lining areas of the middle ear but without retention of keratin (Fig. 23.5). Fibrocystic or fibroosseous sclerosis and epidermization represent nonprogressive, end-stage pathology that is a contraindication to tympanoplasty surgery, because it is very difficult to restore middle ear aeration in such cases.
Pathology of Middle Ear Grafts and Implants
Tympanic membrane perforations can be successfully repaired using a variety of graft materials. Autologous tissue such as temporalis fascia, tragal cartilage perichondrium, and earlobe adipose tissue are all adequate grafting materials with ease of availability near the surgical site and uniformly high take rates in excess of 90%.
Ossicular grafts and prostheses are different in many ways when compared with implants placed elsewhere in the body. Ossicular implants must couple well at their ends to bone or soft tissue but must remain suspended in air elsewhere to avoid unwanted ankylosis (e.g., to the promontory or facial nerve canal). They must maintain not only their shape and size but also their acoustic transmission properties over long periods. For example, changes in mechanical properties of an implant, such as stiffness, can lead to changes in middle ear sound transmission. Furthermore, the recipient middle ear milieu in COM is potentially hostile as a result of active or arrested inflammatory disease or because of inadequate eustachian tube function. Persistent or recurrent infection can predispose to breakdown and resorption of an implant, and tubal insufficiency can accelerate implant extrusion. Also, homograft and synthetic ossicular implants are potentially subject to immune-mediated rejection.
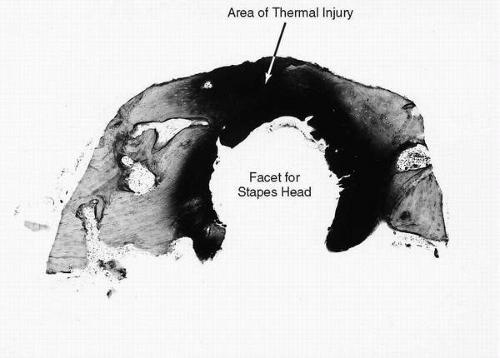
A variety of autograft, homograft, and synthetic materials have been used for reconstructing the ossicular chain. Autologous ossicle grafts (incus or head of malleus), when available, constitute the material of choice (Fig. 23.6). They maintain their morphologic contour, size, shape, and physical integrity for long periods, more than 20 years. They do not incite formation of new bone nor do they undergo resorption (in the absence of infection). They undergo slow replacement of nonviable bone by new bone formation through a process of “creeping substitution.” It is critical to avoid thermal injury when sculpturing such grafts (Fig. 23.7), and the generous use of irrigation is recommended. The general availability, low cost, ease of handling, and time-tested functional results make autologous ossicles a good first choice for ossiculoplasty.
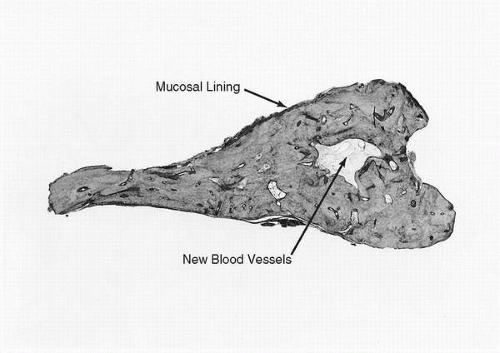
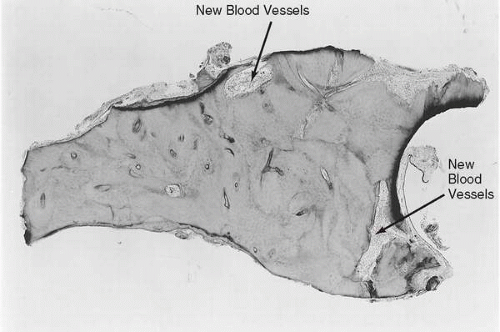
Cortical bone grafts are readily obtained from the mastoid cortex through a postauricular or endaural incision. A 2-mm bur is used to create troughs around a segment of bone that will roughly meet the requirements for length, thickness, and contour. The strut is then separated from the mastoid cortex with an osteotome and then further sculpted with drills, using liberal irrigation to prevent thermal injury. The behavior of autologous cortical bone struts is histologically similar to that of ossicular bone grafts (Fig. 23.8), and cortical bone is a useful and viable alternative for ossiculoplasty.
Homologous human ossicles are also well tolerated histologically. Creeping substitution occurs less rapidly than with autologous ossicles. There are no overt features of immune-mediated rejection. Ossicle grafts made of cartilage often develop chondromalacia with loss of stiffness and a tendency to become resorbed over time. Hence, cartilage grafts are not optimal for ossicular reconstruction, although they are probably adequate as a buffer between prosthesis and the tympanic membrane.
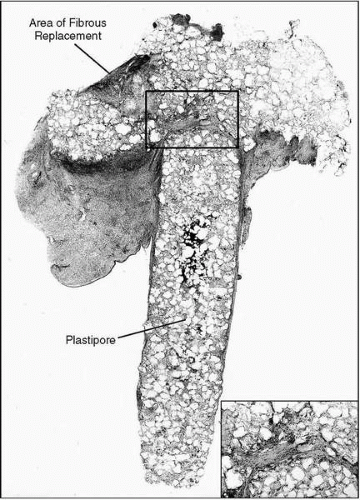
A variety of synthetic ossicular implants are currently available. Those made of porous high-density polyethylene (Plastipore) have been shown to elicit an intense foreign-body giant cell reaction that becomes well established within a few weeks and probably continues for the duration of the implant. Microdegradation of the plastic material occurs and appears to increase with time, eventually leading to implant failure in many cases (Fig. 23.9). More recently, many other synthetic materials have been used for ossiculoplasty, including bioactive glasses (Bioglass, Ceravital), aluminum oxide ceramic, carbon, hydroxylapatite, gold, titanium, hydroxylapatite-polyethylene (Hapex), and others. The histological fate of these other synthetic materials in the human middle ear needs further study. Although these materials may work well in an animal model, results in an animal model cannot always be extrapolated to humans because of species differences and many unique human factors such as chronic inflammation and eustachian tube dysfunction. The extrusion rate of synthetic implants is significantly higher than for autologous tissues. Placement of a cartilage buffer between a synthetic prosthesis and the tympanic membrane has decreased the rate of extrusion, although it has not eliminated the problem. Long-term studies examining biocompatibility, extrusion potential, and functional results are needed before one can determine the place of synthetic implants in otologic surgery.
SELECTION OF CASES
Tympanoplasty should be considered when there is a conductive hearing loss of 30 dB or greater in an ear with COM that has good cochlear function. Tympanoplasty is contraindicated in a dead ear or in an ear with poor cochlear function. Tympanoplasty is not advisable in an ear with fibrocystic sclerosis because of high propensity for postoperative nonaeration of the middle ear and recurrent fibrosis. Similarly, epidermization is a contraindication because of the risks of nonaeration, prosthesis extrusion, and iatrogenic cholesteatoma.
Tympanoplasty carries a small risk of inducing a sensorineural hearing loss. Therefore it is important that cochlear function in the contralateral ear be at an adequate level, and an only hearing ear or much better hearing ear is a contraindication for tympanoplasty.
Children younger than 5 years are poor candidates for tympanoplasty because of risk of subsequent failure from otitis media and poor eustachian tube function. For the elderly, and for adults with serious medical problems, one has to determine whether the benefits of surgery outweigh the risks of anesthesia.
It is important to determine whether the COM in the ear under consideration is active or inactive (Chapter 17). Active COM with cholesteatoma necessitates surgical treatment to remove cholesteatoma (mastoidectomy or atticotomy) in conjunction with tympanoplasty. Active COM without cholesteatoma should be treated medically to control infection and eliminate otorrhea, thus converting the process to inactive COM. Expectant observation for 6 months is recommended, and if the ear remains dry, then elective tympanoplasty may be performed. Failure of medical management in active COM without cholesteatoma generally indicates the need for combining mastoidectomy with tympanoplasty. Ears that drain intermittently and do not have cholesteatoma (inactive COM with frequent reactivation) need attention to obvious inciting events such as water exposure to control otorrhea. If there are no obvious predisposing events, then mastoidectomy is recommended in conjunction with tympanoplasty to eliminate infection and granulation in the mastoid tracts, antrum, and epitympanum.
In patients with bilateral COM, determining which ear to operate on first depends on the type of COM and the severity of conductive hearing loss. In general, the ear with more active disease should be chosen first. With bilateral inactive disease, the poorer hearing ear should be operated on first, similar to the selection process for patients with otosclerosis. An exception to this rule may involve patients with bilateral air-bone gaps with a small difference in the hearing level between the two ears and a better chance for hearing gain in the better hearing ear.
Patients with a history of multiple failed tympanoplasties are likely to have insurmountable hurdles, including nonfunctioning eustachian tubes, middle ear fibrosis, tendency for failures of tympanic membrane grafts, and extrusion of prostheses. In such patients, the goal of chronic ear surgery should be to make the ear safe and dry, and hearing improvement should be achieved by amplification rather than by additional tympanoplasty surgery.
It is sometimes difficult to assess whether tympanoplasty surgery will result in a hearing gain that will be subjectively perceived by the patient to be an improvement in hearing ability. Overall, hearing includes the ability to detect speech in both quiet and in noise, as well as the ability to localize sound. The hearing benefit perceived by a given patient after tympanoplasty depends not only on the magnitude of improvement in air-bone gap but also on the level of cochlear function in the operated ear, the hearing level in the contralateral ear, the symmetry of hearing levels between the two ears, the level of central auditory processing, and the patient’s lifestyle (11). For example, a patient with a bilateral, 50-dB conductive hearing loss who undergoes a successful tympanoplasty in one ear is likely to report more benefit than a patient with a unilateral 50-dB conductive loss who also undergoes a successful tympanoplasty, although in technical terms both operations were equally successful. Patients may express disappointment that their hearing has not improved as much as they had expected. The following initial conditions seem most likely to result in patients being dissatisfied with their hearing improvement: (i) excellent hearing in one ear and a moderate-to-severe mixed type hearing loss in the surgical ear, (ii) longstanding unilateral loss, (iii) a postoperative hearing level that still requires a hearing aid in spite of successful surgery, and (iv) a conductive hearing loss as shown by audiometry but with a positive Rinne test at 256 Hz and 512 Hz (12). Patients with these conditions should not necessarily be excluded from surgical treatment, but the degree of expected improvement must be fully discussed with them to ensure that they have a realistic expectation of what can be achieved.
It must be emphasized that the surgical decision making for tympanoplasty in a patient with COM must be individualized. As discussed earlier, several factors should be considered, including hearing levels in the diseased and contralateral ear, pathology and activity of COM, age, and the general health and medical condition of the patient. These factors must be modified by the experience and talent of the otologic surgeon.
PREOPERATIVE EVALUATION
An otologic history, examination, and audiometric evaluation are done to determine if tympanoplasty surgery is indicated. The clinician must proceed in a logical manner and must quantify the conductive hearing loss, assess cochlear
reserve, gain some insight into the probable ossicular pathology, assess the activity of COM, assess eustachian tube function, assess the contralateral ear, and eliminate potential contraindications. Having decided to proceed with surgery, the surgeon should formulate a preoperative plan, including the type of anesthesia, surgical approach, and type of tympanoplasty. The plan should be flexible to allow for intraoperative revision and modification as necessary.
reserve, gain some insight into the probable ossicular pathology, assess the activity of COM, assess eustachian tube function, assess the contralateral ear, and eliminate potential contraindications. Having decided to proceed with surgery, the surgeon should formulate a preoperative plan, including the type of anesthesia, surgical approach, and type of tympanoplasty. The plan should be flexible to allow for intraoperative revision and modification as necessary.
A history of otorrhea in a patient without cholesteatoma warrants further attention to determine its etiology. As discussed in Chapter 17, medical management may convert the process to inactive COM, and if the ear remains dry for several months, elective tympanoplasty can be considered. Recurrent otorrhea can sometimes be secondary to lack of water precautions or secondary to hearing aid usage, which produces a moist environment. Persistent or recurrent otorrhea despite attention to these factors usually signifies the need for mastoid exploration in addition to tympanoplasty.
Careful otoscopic evaluation using the monocular 6X otoscope or binocular otomicroscope can provide a wealth of useful information to the trained eye. The size and shape of a perforation should be noted, which in conjunction with the extent of anterior canal wall convexity will help to determine the surgical approach. Areas of the tympanic membrane that are dimeric or atrophic may necrose after elevation of a tympanomeatal flap and should be reinforced by grafting. The presence of chronic middle ear effusion, fibrocystic sclerosis of the middle ear, and epidermization are all indicative of eustachian tube dysfunction and constitute contraindications to tympanoplasty. A retraction pocket of the pars flaccida or tensa with retention of keratin debris signifies a cholesteatoma. Signs of infection may be obvious, such as pooling of pus in the middle ear, or subtle, such as minute granulations at the margins of a perforation or an inflamed and edematous middle ear mucosa.
One should assess the integrity of the ossicular chain. Mobility of the malleus can be evaluated by pressure otoscopy if the tympanic membrane is intact or by gentle instrumental manipulation if the drum is perforated. A perforation may allow for inspection of the incus and stapes. Common areas of resorptive osteitis are the long process of the incus and the stapes crura. Chalky white tympanosclerotic plaques around the oval window may signify fixation of the footplate, in which case a second stage stapedectomy may be necessary. If the stapes is visible through a perforation, its mobility may be assessed by observing the superstructure and stapes tendon using otomicroscopy while eliciting the crossed stapedial reflex using a Barany noise box to stimulate the contralateral ear.
A functioning eustachian tube is critical to the success of tympanoplasty surgery; however, tests of eustachian tube function that can be used preoperatively as a reliable predictor of surgical success do not exist (13,14). Autoinflation of the ear by the Valsalva maneuver can be of diagnostic value in some patients. It may help to determine the extent of retraction and mobility of the tympanic membrane or a retraction pocket. In the presence of a perforation, simultaneous autoinflation and auscultation can demonstrate the anatomic patency of the tube. However, forced inflation is unphysiologic and is therefore not a valid test of eustachian tube function. Indirect indicators for poor eustachian tube function include bilateral chronic otitis media, chronic serous otitis media in the contralateral ear, uncontrolled rhinosinusitis, cleft palate, and other skull base anomalies.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree