Oropharyngeal dysphagia (OPD) is a challenging and relatively common condition in children. Both developmentally normal and delayed children may be affected. The etiology of OPD is frequently multifactorial with neurologic, inflammatory, and anatomic conditions contributing to discoordination of the pharyngeal phase of swallowing. Depending on the severity and source, OPD may persist for several years with significant burden to a patient’s health and family. This article details current understanding of the mechanism and potential sources of OPD in children while providing an algorithm for managing it in the acute and chronic setting.
Key points
- •
Oropharyngeal dysphagia (OPD) is the presence of laryngeal penetration or aspiration of food contents, predominately liquid, during oral ingestion.
- •
The incidence of OPD in children is on the rise due to increasing life expectancy of premature infants and children with complex medical conditions.
- •
Identification and resolution of OPD in children is best determined by the presence or absence of symptoms, including wet respirations and coughing and choking during drinking.
- •
An initial clinical evaluation of feeding and swallowing is instrumental in assessment of OPD in children whereas video fluoroscopic swallow studies (VFSSs) and fibreoptic endoscopic evaluations of swallowing (FEES) remain the best tools for confirming aspiration in infants and children.
- •
Persistent OPD in neurologically normal children demands careful evaluation for potential etiologies and is best managed by a dedicated multidisciplinary team.
Introduction
Swallowing disorders can be identified at all ages. Coughing, choking, and wet respirations with feeding are all evidence of feeding problems in newborns and children. When left undiscovered or untreated, recurrent cough, bronchiectasis, reactive airway disease, and pneumonias may ensue. The cycle of symptoms and sickness is frequently stressful to patients and their caretakers who simply want their child to eat normally. The duration of dysphagia and difficulty in identifying the source compounds this anxiety. Unfortunately, epidemiologic data and sound diagnostic and treatment protocols for dysphagia are not well established.
Swallowing disorders in infants and children are common, with 25% of the pediatric population reported to experience some type of nonspecific feeding difficulty. OPD is the most commonly encountered feeding disorder and refers to the dysfunction of the oral and pharyngeal phase of swallowing that results in laryngeal penetration and aspiration of solid or liquid food. As expected, higher rates of OPD are discovered in children with prematurity, upper aerodigestive tract anomalies, central nervous system (CNS) malformations, neurodevelopmental delays, and craniofacial syndromes. OPD is rarely an isolated event, however, and occurs in both developmentally delayed and normal children.
Recent advances in neonatal medicine have improved the survival of premature infants (<37 weeks’ gestation) and those with complex medical conditions, thereby increasing the number of children in the community with residual difficulties with feeding and OPD. The correlation between prematurity, complex medical conditions and feeding disorders in children is well established. Pediatricians and otolaryngologists now see a greater number of children with persistent OPD. This includes developmentally normal and neurologically intact children who, as demonstrated by Sheikh and colleagues, can present with chronic aspiration. The impact of OPD on the health of developmentally normal children emphasizes the importance of an extensive work-up and effective algorithm for treatment. Subtle inflammatory and anatomic problems are frequently present in otherwise healthy children with OPD.
Delayed reflexes, hypotonia, and generalized discoordination complicate the control of normal swallowing function in neurologically or developmentally affected children. Alternative feeding options or modified diets help maintain nutrition in this population pending improvement in function and strength. Gastrostomy tubes are frequently necessary to achieve fluid and nutritional goals. Depending on the underlying neurologic condition, dysphagia may take many years to improve and may never reach a normal state. Nonetheless, inflammatory and anatomic conditions, such as reflux, generalized respiratory illness, and upper aerodigestive anatomic anomalies, need to be assessed for in neurologically affected children because they may exacerbate their OPD.
The psychological impact of OPD on the family complicates early intervention because significant dysfunctional interactions between mothers and their infants with feeding disorders have been found. The chronic nature of OPD with associated complications and the strain on the child and the family requires a dedicated team that caters to the medical, social, and dietary needs of these patients. Such a multidisciplinary team should consist of, with varying degrees of involvement, a pediatric otolaryngologist, pulmonologist, gastroenterologist, pediatric surgeon, speech and language pathologist (SLP), radiologist, nutritionist, occupational therapist, psychologist, and social worker. The objective of this clinical review is to provide pediatricians and otolaryngologists a global understanding of the potential causes of dysphagia and to provide an algorithm for diagnosing and treating infants and children with complicated or persistent OPD.
Introduction
Swallowing disorders can be identified at all ages. Coughing, choking, and wet respirations with feeding are all evidence of feeding problems in newborns and children. When left undiscovered or untreated, recurrent cough, bronchiectasis, reactive airway disease, and pneumonias may ensue. The cycle of symptoms and sickness is frequently stressful to patients and their caretakers who simply want their child to eat normally. The duration of dysphagia and difficulty in identifying the source compounds this anxiety. Unfortunately, epidemiologic data and sound diagnostic and treatment protocols for dysphagia are not well established.
Swallowing disorders in infants and children are common, with 25% of the pediatric population reported to experience some type of nonspecific feeding difficulty. OPD is the most commonly encountered feeding disorder and refers to the dysfunction of the oral and pharyngeal phase of swallowing that results in laryngeal penetration and aspiration of solid or liquid food. As expected, higher rates of OPD are discovered in children with prematurity, upper aerodigestive tract anomalies, central nervous system (CNS) malformations, neurodevelopmental delays, and craniofacial syndromes. OPD is rarely an isolated event, however, and occurs in both developmentally delayed and normal children.
Recent advances in neonatal medicine have improved the survival of premature infants (<37 weeks’ gestation) and those with complex medical conditions, thereby increasing the number of children in the community with residual difficulties with feeding and OPD. The correlation between prematurity, complex medical conditions and feeding disorders in children is well established. Pediatricians and otolaryngologists now see a greater number of children with persistent OPD. This includes developmentally normal and neurologically intact children who, as demonstrated by Sheikh and colleagues, can present with chronic aspiration. The impact of OPD on the health of developmentally normal children emphasizes the importance of an extensive work-up and effective algorithm for treatment. Subtle inflammatory and anatomic problems are frequently present in otherwise healthy children with OPD.
Delayed reflexes, hypotonia, and generalized discoordination complicate the control of normal swallowing function in neurologically or developmentally affected children. Alternative feeding options or modified diets help maintain nutrition in this population pending improvement in function and strength. Gastrostomy tubes are frequently necessary to achieve fluid and nutritional goals. Depending on the underlying neurologic condition, dysphagia may take many years to improve and may never reach a normal state. Nonetheless, inflammatory and anatomic conditions, such as reflux, generalized respiratory illness, and upper aerodigestive anatomic anomalies, need to be assessed for in neurologically affected children because they may exacerbate their OPD.
The psychological impact of OPD on the family complicates early intervention because significant dysfunctional interactions between mothers and their infants with feeding disorders have been found. The chronic nature of OPD with associated complications and the strain on the child and the family requires a dedicated team that caters to the medical, social, and dietary needs of these patients. Such a multidisciplinary team should consist of, with varying degrees of involvement, a pediatric otolaryngologist, pulmonologist, gastroenterologist, pediatric surgeon, speech and language pathologist (SLP), radiologist, nutritionist, occupational therapist, psychologist, and social worker. The objective of this clinical review is to provide pediatricians and otolaryngologists a global understanding of the potential causes of dysphagia and to provide an algorithm for diagnosing and treating infants and children with complicated or persistent OPD.
Mechanism of normal and dysfunctional swallowing
Normal swallowing is a complex process that involves both voluntary and involuntary mechanisms. It includes 4 phases: oral preparatory, oral transit, pharyngeal, and esophageal. The oral preparatory phase involves grinding or chewing the food and mixing with saliva, creating a food bolus of appropriate size and consistency. The food bolus is voluntarily pushed backwards into the oropharynx. The backward movement to the oropharynx triggers the reflex pharyngeal phase.
The pharyngeal phase of swallowing is reflex mediated by the stimulation of the afferent receptors along the anterior tonsillar pillars, base of tongue, and epiglottis. The resultant efferent motor muscular activity is mediated by the glossopharyngeal (cranial nerve [CN] IX) and vagus (CN X) nerves. This muscular activity is a complex and coordinated contraction involving a series of muscle groups to ensure quick bolus passage across the relaxed cricopharyngeal or upper esophageal sphincter (UES) while simultaneously protecting the airway. The bolus is directed posteriorly by the voluntary propulsion of the tongue and then by the sequential reflex contractions of pharyngeal constrictors. The soft palate moves against the posterior pharyngeal wall to close the nasopharyngeal port. At the same time, the hyoid is advanced anteriorly by contraction of the strap muscles while pulling the larynx anteriorly and superiorly. In the process, the epiglottis is retroflexed to cover the laryngeal introitus.
During the pharyngeal phase, various measures protect the airway to prevent aspiration. The pharyngoglottal closure reflex is initiated by the sensory and chemoreceptors in the pharynx and larynx and is mediated by the CN IX and CN X nerves. When stimulated, adduction of true vocal cords and approximation of arytenoid cartilages occurs by contraction of the thyroarytenoid and interarytenoid muscles, thereby closing the laryngeal inlet.
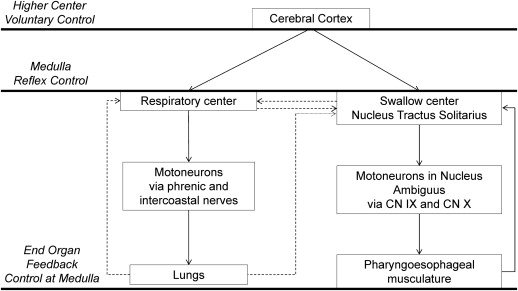
The swallow center of the CNS is located in the medulla along the nucleus tractus solitarius and the nuclei of the reticular system of the fourth ventricle. The supranuclear connections are relayed from the swallow center via the hypothalamus to the cerebral cortex. The swallow center is the area for coordination of the afferent and efferent activity in swallowing and transmits inhibitory impulses to the adjacent respiratory center, located in the medulla, thus inhibiting respiration during swallowing. The afferent oropharyngeal, pharyngeal, and laryngeal receptors relay information via afferent nerves in CN IX and CN X and the efferent arm is relayed via the same nerves from nuclei located in the nucleus ambiguus ( Fig. 1 ).
The laryngeal adductor reflex (LAR) is the second protective reflex that is more specific to the supraglottic portion of larynx. It is mediated by the internal sensory division of the superior laryngeal nerve (CN X) supplying the mucosal surface of the epiglottis, aryepiglottic folds, and posterior larynx above the vocal cords. The LAR coordinates the sensory input from these areas and relays them to the medulla. The efferent return through the recurrent laryngeal nerve (CN X) causes contraction of the thyroarytenoid and interarytenoid muscles, which results in reflex closure and protection of the airway.
The significance of normal laryngopharyngeal sensation is demonstrated by recent studies using FEES with sensory testing. Evidence suggests that laryngopharyngeal sensation is reduced or inhibiting in pediatric and adult patients with OPD.
The stimulation of the swallow center in the medulla inhibits the adjacent respiratory center that results in a temporary cessation of respiration, which accompanies the laryngeal upward movement, the closure of epiglottis, and the reflex closure of the larynx during the process of deglutition. The temporal coordination of breathing and pharyngeal phase of swallow is critical. Unfortunately this process can be severely disrupted in children with neurologic conditions and chronic lung disease associated with prematurity, thus increasing the risk of aspiration in these groups.
The movement of the food bolus below the pharynx occurs with opening of the UES, primarily by reflex relaxation of the cricopharyngeus muscle, and aided by the upward and anterior movement of larynx. This is followed by the esophageal phase of swallowing, which is reflex mediated under the influence of the autonomic nervous system of cervical and thoracic ganglia.
Age-Related Differences—Maturation of Swallow with Age
All the phases of swallowing are demonstrable in children, adolescents, and adults. There are some inherent differences, however, in swallowing between neonates, infants and adolescents. The oral phase in neonates and infants is a primitive sucking reflex. The buccal pads are prominent to aid sucking; the tongue protrudes whereas the perioral muscles, including the lips, cheeks, tongue, and palate act rhythmically and synergistically like a single organ to compress the nipple and express its contents. In the first 3 months, infants fail to differentiate consistency between solids and liquids and use the same suck reflex for both. Furthermore, the pharyngeal phase in infants lasts longer than in adults. In spite of the longer duration of the pharyngeal phase in infants, no aspiration is noticed in a majority, possibly due to a more efficient laryngeal closure owing to the softer cartilaginous framework.
The coordination between breathing and swallowing, as described previously in adults, translates into a coordinated suck-swallow-breathe sequence in infants, so that they can suck efficiently and swallow rapidly with minimal interruption in airflow. Poor coordination of this sequence is associated with prematurity and patients with cerebral palsy (CP). Upper airway obstruction in neonates and infants may interrupt this sequence mainly by breathlessness and prolonged sucking when infants are unable to generate a sufficient suction pressure in the presence of obstruction. This subtle discoordination between eating and breathing contributes to OPD in infants with upper airway obstruction.
As an infant matures, the jaw grows and the buccal pads are absorbed to increase the intraoral space. The protrusion of tongue, which is an important component of suckling, is gradually lost by 6 months and replaced by raising and lowering of the tongue. This is coupled with increasing use of tongue intrinsic musculature, which is responsible for the development of propulsive action. At this stage, the infants may be fed with solids as their voluntary swallow function starts to mature beyond the primitive suckling. The rhythmic biting in response to stimulation of the alveolar ridge gradually develops into mastication with the development of deciduous teeth. This stage represents a maturation of swallowing that may continue to 24 months of age. These changes represent a continuum of development in response to stimulation in the form of changing oral feeding habits. Lack of development is often noticed in infants on gastrostomy feeds who develop oral aversion and OPD if oral stimulation is not attempted.
Etiology of oropharyngeal dysphagia
Efficient and effective swallowing relies on 2 important steps. The voluntary oral skills that involve preparation of the food bolus and the reflex patterned motor actions of swallowing. This combination results in the coordinated action and inhibition of the muscle groups located around the oropharynx and esophagus responsible for the passage of food into the stomach. As discussed previously, voluntary oral skills are not present until 6 months of age and may be a primary source of dysfunction in this age group. This is especially true if neonatal hospitalization and chronic illness prevents normal oral intake and stimulation at this key developmental age.
Frequently, OPD is multifactorial ( Box 1 ). Developmental and neurologic delays can result in discoordination of swallow and contribute to OPD. Inflammatory, obstructive, and anatomic conditions may also be involved and are more frequently seen in developmentally normal individuals. Contributing factors may be grossly apparent at presentation or only through meticulous investigation. For example, prematurity and laryngomalacia can both independently contribute to OPD but premature patients have more prolonged symptoms than seen in those with laryngomalacia alone. Contributing factors in children with OPD are outlined.
|
|
|
|
|
|
|
|
|
|
|
|
a CHARGE stands for coloboma of the eye, heart defects, atresia of the nasal choanae, retardation of growth and/or development, genital abnormalities, and ear abnormalities.
Prematurity
A functionally appropriate feeding pattern in neonates and young infants involves a coordinated suck-swallow-breathing rhythm so that an infant can suck efficiently and swallow rapidly with minimal airflow interruption. Due to neurologic immaturity, prematurity less than 34 weeks may be associated with poor coordination of this rhythm. Prematurity contributes to a delay in the pharyngeal phase of swallowing as demonstrated on high-resolution manometry studies of neurologically normal preterm infants at 31 to 32 weeks. Poor pharyngeal pressures coupled with poor coordination of pharyngeal propulsion and UES relaxation were found compared with term infants. Weaker pharyngeal pressures were presumably related to neurologic immaturity in the premature infants.
Premature infants also have a weak suck reflex. A sucking pattern consists of suckling bursts. An immature pattern may include a short burst of 4 to 6 sucks at 1 to 1.5 sucks/s and a mature pattern may consist of approximately 30 sucks at 2 sucks/s. The number of sucking bursts gradually increases by term gestation. These suckling bursts should be coordinated with breathing and swallowing. A poorly coordinated suck-swallow-breathe sequence is found in infants born before 34 weeks of gestation due to lack of myelination in the medulla. A mature sucking pattern is characterized by prolonged suckling bursts of more than 10 sucks with suck-swallow-breathe in equal proportions with a ratio of 1:1:1. A delay in maturation of the swallow and sucking reflex is reported in patients born very early when sucking patterns were analyzed at a corrected age of 40 weeks. Extremely preterm infants born at 24 to 29 weeks’ gestation generate significantly fewer bursts and sucks per burst than more mature preterm infants (30–32 weeks) and those born at term. This causes preterm infants to have a tendency to aspirate easily and fatigue quickly. This can make breastfeeding difficult and accounts for more desaturations in preterm infants when feeding.
Preterm infants are also more likely to suffer anoxia or hypoxia at birth. This can result in permanent, but sometimes subtle, neurologic damage, including dysfunctional feeding patterns. A higher incidence of CP is found in preterm infants with lower gestational age (24–26 weeks) compared with those born later. These patients primarily suffer with poor and noncoordinated oral skills required for sucking. They also exhibit poor head control, uncoordinated tongue movements, impaired palatal function, poor gag reflex, and laryngopharyngeal hyposensitivity; all of which increase the risk of OPD and aspiration. Subtle and radiographically undetectable hypoxic injury to the swallowing and respiratory centers in premature infants may help explain the increased incidence of OPD in these children.
Intubation as a newborn can also contribute to OPD in this population. The presence of an endotracheal tube and the resultant remodeling of the soft palate can lead to palatopharyngeal incompetence, nasal reflux, or a defective integration of the suck-swallow mechanism. On the other hand, the presence of a tracheostomy tube in a newborn can prevent the normal rise of subglottic pressure and laryngeal elevation necessary for an effective pharyngeal phase of swallowing.
Neurologic Disorders
The manifestation, course, and possible resolution of OPD in neurologically affected children are determined by the nature, site, and evolution of the CNS defect. The prognosis for recovery also is influenced strongly by whether the underlying neurologic condition is static or progressive. Static neurologic conditions include CP, cerebrovascular accident, Arnold-Chiari malformation, syringomyelia, congenital viral infections with varicella, cytomegalovirus, tumors, and injuries to the brainstem. Progressive neurologic disorders are not limited to but include myopathies, neuropathies, and metabolic disorders like mucopolysaccharidosis. Children with static neurologic diagnoses generally improve in their OPD with developmental progress. Children with progressive neurologic conditions demonstrate early improvement but eventually lose these skills.
The most common neurologic condition encountered in children with OPD is CP. CP affects volitional oral movements and the involuntary reflexes (LARs) and compromises the neurologically dependent reflexive pharyngeal swallow. The situation is worsened by poor coordination of the suck-swallow-breathe sequence as infants. CP patients frequently have a weak gag reflex and are prone to silent aspiration. Volitional movements are affected when there is cortical injury or periventricular leukomalacia whereas reflex inhibition suggests subcortical injury involving brainstem and basal ganglia. Although it is hard to predict the incidence of OPD in CP patients, 85% to 90% of patients with CP are affected by dysphagia. Chronic aspiration may be further complicated by the presence of gastroesophageal reflux disease (GERD) and drooling, which are present in more than 50% of cases. Drooling is secondary to impaired volitional movements whereas posterior salivation causes recurrent aspiration and subsequent pulmonary infections.
Other common static conditions include Arnold-Chiari and central arteriovenous malformations, which may be present with only subtle clinical evidence of OPD. A high index of suspicion for OPD is necessary in these patients. Greenlee and colleagues reported that children with a Chiari malformation type 1 (CM-I) were most likely to present with OPD under 3 years of age. After evaluating the signs and symptoms of CM-I in children younger than 6 years of age, Albert and colleagues also determined that 77.8% presented with OPD between 0 and 2 years of age. Indirect neurologic signs, such as a hoarse cry, delayed milestones, unsteady gait, and worsening OPD on VFSS, also may be present and should prompt an early brain MR imaging or neurology consult. This approach has been recommended in neurologically intact children with worsening or persistent OPD after 2 years of age. In a child with new onset of OPD, CNS neoplasms should also be ruled out using MR imaging.
O’Neill and colleagues demonstrated that more than 50% of children with Down syndrome had evidence of persistent OPD. The mean age at diagnosis of OPD was 1.6 years. Resolution rates of OPD were also poor (15%) in this population, especially in patients with significant neurologic delay and prior tracheostomies. They suspected that inherent hypotonia and poor pharyngeal reflexes in the Down syndrome children contributed to the swallowing results found in their study. Moreover, procedures aimed at reducing upper airway obstruction had no effect on the resolution rates of OPD in their study.
Anatomic Contributors to OPD
Poor coordination of the suck-swallow-breath sequence may be observed in infants with upper airway obstruction. Similarly, in older infants and children, upper airway obstruction complicates swallowing by limiting normal respiration; this is particularly true in patients when OPD is multifactorial. Conditions associated with airway obstruction may contribute to OPD and include both congenital and acquired entities ( Box 2 ).
|
|
Nasal or nasopharyngeal obstruction in an infant can complicate coordination of the suck-swallow-breathing rhythm. This is because neonates up to 3 months of age are obligate nasal breathers. Bilateral choanal atresia often causes respiration difficulty and swallowing dysfunction. Choanal stenosis patients typically fatigue and take short breaks during feeding, making coordination difficult. In older infants and children, nasal obstruction may be a result of allergic rhinitis, turbinate hypertrophy, adenoid hypertrophy, sinusitis, pyriform aperture stenosis, or nasopharyngeal or nasal congenital masses, such as glioma, meningocele, and nasal dermoid. It is important to document an appropriate patency of the nasopharyngeal airway in the evaluation of OPD. This is particularly relevant in late infancy and the early second year of life when adenoid hypertrophy is a primary source of obstruction. Anecdotal evidence suggests that chronic rhinitis and nasal obstruction affect VFSS results and complicate weaning off a modified diet in young children with OPD.
Development of normal oral and oropharyngeal anatomy is important for natural suckling in neonates and the preparatory phases of swallowing in children. Craniofacial dysmorphisms and cleft lip or cleft palate have an impact on normal oral intake. Some children, as seen in Beckwith-Wiedemann syndrome, have a disproportionately large tongue that interferes with early oral preparation and oropharyngeal function.
Laryngeal elevation propels the food bolus whereas protective reflexes in the hypopharynx and larynx aid in the coordination of breathing and swallowing and at the same time offer laryngeal protection. Anatomic abnormalities of the hyphopharynx and larynx can result in OPD. These include vocal fold paralysis, vallecular cysts, laryngotracheal clefts, glottic webs, laryngomalacia, and subglottic stenosis. Laryngotracheal reconstruction, with alteration of normal laryngeal anatomy, can contribute to temporary or long-term OPD. Vocal fold paralysis with the loss of recurrent laryngeal nerve function increases the chance of aspiration owing to reduced vocal fold adduction, an open posterior glottis, and potentially the loss of sensation associated with superior laryngeal nerve weakness. Airway obstruction due to webs or subglottic stenosis with difficulties in ventilation cause early fatigue of respiration and swallowing, leading to OPD. Deep laryngeal clefts (Benjamin-Inglis types 2–4) allow for passage of food contents directly into the larynx below the level of the vocal folds. The diagnosis and management of the less obvious type 1 laryngeal clefts can be challenging with late diagnosis and persistent OPD. These laryngoesophageal defects may often be associated with esophageal dysmotility and complicated by GERD.
Laryngomalacia is the most common cause of stridor in newborns and infants due to redundancy and/or weakness of the supraglottic larynx. Airway symptoms are secondary to dynamic inspiratory collapse of the supraglottic structures and redundant mucosa. Laryngomalacia is associated with OPD in more than 50% of patients. Airway obstruction may interfere with the suck-swallow-breathing rhythm pattern and increases dysphagia and GERD, which in turn can reduce laryngeal sensation and exacerbate laryngeal edema. Management of GERD can improve the respiratory pattern and dysphagia and result in improved weight gain in these patients. Laryngomalacia is associated with reduced laryngeal sensitivity, which enhances the risk of silent aspiration. Increased diameter and surface area of the nerve endings have been reported in supra-arytenoid specimens harvested from laryngomalacia patients that may represent an autocrine enhancement of dysfunctional nervous system due to laryngomalacia.
Cervical and distal esophageal anatomic anomalies may also contribute to persistent OPD, including esophageal atresia, tracheoesophageal fistula (TEF), and cricopharyngeal achalasia.
Dysphagia can be a persistent issue after repair of both esophageal atresia and TEF owing to disrupted upper esophageal neuromuscular control and chronic GERD. Patients may be on a modified diet (liquid thickeners) for many years after the repair. It is important to rule out an associated laryngeal cleft because this may also be present in a significant number of patients with distal esophageal anatomic anomalies.
The cricopharyngeus muscle is a striated muscle that is contracted at rest, thus keeping the esophagus closed during respiration. Cricopharyngeal achalasia is thought to involve spasm or incomplete relaxation of the cricopharyngeus muscle. This is uncommon in children but can be diagnosed by identification of a prominent bar on VFSS, with OPD found in approximately 50% of cases. Increased pressures proximal to the muscle can also be demonstrated on manometry and confirmed by electromyography. Management with cricopharyngeus myotomy or dilatation has been reported useful in relieving symptoms of affected patients.
Inflammatory Conditions
Gastroesophageal reflux (GER) is a normal physiologic phenomenon known to occur in all healthy infants. Actual repeated expulsion of gastroesophageal contents from the oral cavity in GER is reported to occur in approximately 40% of infants. On the other hand, the prevalence of symptomatic or pathologic GER or GERD is estimated to occur in 10% to 20% of infants in North America. Some children are at higher risk of GERD, including those with neurologic impairment, obesity, esophageal achalasia, hiatal hernia, prematurity, bronchopulmonary dyplasia, and esophageal atresia. GERD can contribute to persistent OPD by reducing mucosal sensation and laryngeal reactivity (LAR) during the pharyngeal phase of swallowing owing to mucosal injury by caustic reflex contents. Reduced laryngeal sensation has been demonstrated in the setting of chronic reflux in both animals and infants. In view of the prevalence of GERD, treatment has become an important part of OPD management in children.
Eosinophilic esophagitis (EoE) is a chronic immune-mediated condition characterized by clinical symptoms secondary to esophageal dysfunction and histologically by eosinophilic infiltration of the esophagus. Feeding difficulties are the most common symptoms in infants and toddlers, with vomiting and retrosternal pain in children and adolescents. The main histologic feature of EoE is striking eosinophilia of esophageal mucosa with microabcesses and basal zone hyperplasia. The relationship to EoE to OPD is unclear. EoE is associated, however, with GERD and food allergies, both of which are thought to contribute to chronic inflammation and reduced sensitivity of the larynx. Such a reaction to cow milk protein has been described and careful history with radioallergosorbent (RAST) testing may be useful to help identify the cause quickly.
Esophageal biopsies and histology usually confirms the diagnosis of EoE and the management consists of dietary modification and reflux therapy. Three diet forms are commonly prescribed: an elemental diet that is a liquid formula based on amino acids and free of all allergens, a 6-food elimination diet that removes commonly identified allergens, or a targeted elimination diet that eliminates food identified as allergic to patient after testing. Swallowed corticosteroids are also effective in treating acute exacerbations of EoE but the disease often relapses after discontinuation.
Evaluation of pediatric oropharyngeal dysphagia
History and Physical Examination
Slow feeding, blue spells, frequent respiratory pauses, or wheeze and/or cough during the feed suggests OPD in an infant. Wet respirations (biphasic washing machine sound) with a wet cry or voice suggest silent aspiration and OPD in both infants and children. The importance of detecting a postprandial wet voice by itself is not considered diagnostic but is likely useful in identifying those with dysphagia related to laryngeal dysfunction. Airway symptoms, such as breathlessness, stridor, and wheeze, may mask silent aspiration and a high index of suspicion for OPD in these patients is well served. Weight gain is an important predictor of health and nutrition in children with OPD and should be followed closely. Discussion of perinatal events and gestational age help tease out the cause of OPD in otherwise normal children. Parents should also be asked about potential neurologic, inflammatory, and anatomic sources of OPD (discussed previously). A history of recurrent and chronic lower respiratory tract infections, reactive airway disease, and pneumonia, especially if severe enough to warrant hospitalization, is an important symptom of pediatric OPD. In less severe cases, infants may sound congested due to chronic respiratory secretions and bronchitis from chronic microaspiration. Delays in speech and gait may also indicate subtle central pathology in older children.
A complete and thorough otolaryngology examination is essential in the diagnosis of OPD and exploration of potential etiology. Syndromic facial characteristics should be searched for. Auscultation for wheezing, course breath sounds, and wet voice/cry or respiration before and after eating is essential. This is best performed by an SLP who can observe subtle symptoms of OPD during oral intake and postprandially. Nasal patency and identification of upper aerodigestive tract obstruction are essential components of the examination.
Flexible fiberoptic nasolaryngoscopy should be performed as routine part of the examination in patients with OPD. This provides anatomic detail of the nasal cavity, nasopharynx, oropharynx, hypopharynx, and larynx while identifying evidence of chronic mucosal inflammation of these sites, which may be secondary to rhinitis, postnasal drip, and GERD. Low lying tonsils, laryngomalacia, laryngeal clefts, and evidence of hypopharyngeal residue can be seen with this examination.
In all cases of suspected OPD it is important to involve SLP early in the process of evaluation. Clinical bedside evaluation or clinical feeding evaluation can be easily performed ( Box 3 ). Evaluation using 3-oz water challenge has been described. With this brief study, a child is observed during and after oral consumption of up to 3 oz of water. OPD can manifest with coughing, choking, or tearing occurring during or shortly after the test. Suiter and colleagues reported their results in children between 2 and 18 years of age. Compared with FEES, the investigators concluded that the 3-oz challenge had high sensitivity but a low specificity, indicating a high false-positive rate, suggesting that normal children who cleared this test may be safely given thin liquids. It is not a good screening tool for children at high risk of aspiration, however, and is not a good indicator of silent aspiration.



