Orbit
7.1 Orbital Disease
This section provides a framework to evaluate a variety of orbital disorders.
Symptoms
Eyelid swelling, bulging eye(s), and double vision are common. Pain, decreased visual acuity, and decreased color vision can occur.
Signs
Critical. Globe dystopia (e.g., proptosis/exophthalmos, hypoglobus, hyperglobus) and restriction of ocular motility, which can be confirmed by forced duction testing (SEE APPENDIX 6, FORCED DUCTION TEST AND ACTIVE FORCE GENERATION TEST). Resistance to retropulsion of the globe is common.
Differential Diagnosis of Proptosis
Mass effect (e.g., infiltration or displacement of soft tissues by inflammatory, neoplastic, or infectious etiologies).
Enlarged globe (e.g., myopia). Large, myopic eyes frequently have tilted discs and peripapillary crescents, and ultrasonography (US) reveals a long axial length. Asymmetric myopia may present as unilateral proptosis.
Enophthalmos of the fellow eye (e.g., after an orbital floor fracture).
Asymmetric eyelid position: Unilateral upper and/or lower eyelid retraction, or contralateral upper eyelid ptosis.
Etiology
Rarely, specific signs of orbital disease are diagnostic. Otherwise, orbital disease can be grouped into six broad categories to help tailor the necessary work-up:
Inflammatory: Thyroid eye disease (TED), idiopathic orbital inflammatory syndrome (IOIS), sarcoidosis, granulomatosis with polyangiitis (GPA) (Wegener granulomatosis), reactive inflammation from sinusitis, IgG4-related systemic disease, etc.
Infectious: Orbital cellulitis, subperiosteal abscess (SPA), mucormycosis, etc.
Neoplastic (discrete, infiltrative, or hematologic): Typically categorized as primary (e.g., cavernous hemangioma), or secondary (e.g., extension of sinus mucocele or intracranial meningioma, etc). May be benign, malignant, or metastatic.
 NOTE: As a general rule, any patient with a history of cancer and a new orbital process should be assumed to have metastatic disease unless proven otherwise.
NOTE: As a general rule, any patient with a history of cancer and a new orbital process should be assumed to have metastatic disease unless proven otherwise.
Trauma: Orbital fracture, retrobulbar hemorrhage, orbital foreign body, carotid–cavernous fistula, etc.
Malformation: Skeletal abnormalities, congenital/genetic syndromes, etc.
Vascular: Usually either congenital or acquired and categorized as primary arterial (e.g., carotid–cavernous fistula) or venous (e.g., varix). Lymphangioma may also cause proptosis from intralesional hemorrhage.
Work-Up
History: Rapid or slow onset? Pain? Ocular bruit and/or pulsation? Fever, chills, systemic symptoms, skin rash, weight change? History of malignancy, diabetes, pulmonary disease, or renal disease? Trauma? History of sinonasal congestion, epistaxis? Smoking? Up to date with health maintenance and age appropriate screenings (e.g., mammography, prostate examination/screening)?
Examination:
Review vital signs, particularly temperature.
Check visual acuity, size and reactivity of pupils, visual fields, color vision, intraocular pressure. Check for pulsatility of semicircles on Goldmann tonometry.
Check extraocular movements. Measure any ocular misalignment ([prisms or Maddox rod], SEE APPENDIX 3, COVER/UNCOVER AND ALTERNATE COVER TESTS AND 10.7, ISOLATED FOURTH NERVE PALSY). Consider a forced duction test in select cases (SEE APPENDIX 6, FORCED DUCTION TEST AND ACTIVE FORCE GENERATION TEST).
Check for proptosis. Tilt the patient’s head back and look from below (“ant’s-eye view”). Measure with a Hertel exophthalmometer. Position the exophthalmometer against the lateral orbital rims, not the lateral canthi. Average value is 17 mm with the upper limit of normal about 22 to 24 mm. A difference between the two eyes of more than 2 mm is considered abnormal. Can be used in conjunction with a Valsalva maneuver if a venous malformation is suspected. In addition to classic axial exophthalmos, also look for nonaxial displacement of the globe (e.g., hypoglobus, hyperglobus).
Test resistance to retropulsion by gently pushing each globe into the orbit with your thumbs. Feel along the orbital rim for a mass. Check the conjunctival cul-de-sacs carefully and evert the upper eyelid.
Check trigeminal and facial nerve function. Check for preauricular and cervical adenopathy.
Perform a dilated examination to evaluate optic nerves (pallor, swelling), posterior pole (especially for chorioretinal folds), and peripheral retina.
Consider automated perimetry if compressive optic neuropathy is suspected.
Imaging studies: Orbital computed tomography (CT) (axial, coronal, and parasagittal views) or magnetic resonance imaging (MRI) with gadolinium and fat suppression, depending on suspected etiology. Orbital B-scan (US) with or without color Doppler imaging is useful if the diagnosis is uncertain or when a cystic or vascular lesion is suspected. Consider optical coherence tomography (OCT) to assess optic nerve contour. SEE CHAPTER 14, IMAGING MODALITIES IN OPHTHALMOLOGY.
Laboratory tests when appropriate: Triiodothyronine (T3), thyroxine (T4), thyroid-stimulating hormone (TSH), thyroid-stimulating immunoglobulin (TSI), angiotensin-converting enzyme (ACE), cytoplasmic staining and perinuclear staining antineutrophil cytoplasmic antibody (cANCA and pANCA), lactate dehydrogenase (LDH), IgG/IgG4 levels, antinuclear antibody (ANA), complete blood count (CBC) with differential, blood urea nitrogen (BUN)/creatinine (especially if CT contrast or gadolinium is indicated), fasting blood sugar/hemoglobin A1c, blood cultures, etc.
Consider further systemic work-up and additional imaging, depending on clinical suspicion and radiologic findings (metastasis, lymphoma, etc.).
Consider an excisional or incisional biopsy, as dictated by the working diagnosis. Fine-needle aspiration biopsy has a limited role in orbital diagnosis.
Additional work-up, treatment, and follow-up vary according to the suspected diagnosis. See individual sections.
7.2 Inflammatory Orbital Disease
7.2.1 THYROID EYE DISEASE
Synonyms: Thyroid-Related Orbitopathy, Graves Disease
Ocular Symptoms
Early: Nonspecific complaints including foreign-body sensation, redness, tearing, photophobia, and morning puffiness of the eyelids. Early symptoms are often nonspecific and may mimic allergy, blepharoconjunctivitis, chronic conjunctivitis, etc. Upper eyelid retraction tends to develop early.
Late: Additional eyelid and orbital symptoms including lateral flare, prominent eyes, persistent eyelid swelling, chemosis, double vision, “pressure” behind the eyes, and decreased vision.
Signs
(See Figure 7.2.1.1.)
Critical. Retraction of the upper eyelids with lateral flare (highly specific) and eyelid lag on downward gaze (von Graefe sign), lagophthalmos. Lower lid retraction is a very nonspecific sign and often present as a normal finding. Unilateral or bilateral axial proptosis with variable resistance to retropulsion. When extraocular muscles are involved, elevation and abduction are commonly restricted and there is resistance on forced duction testing. Although often bilateral, unilateral or asymmetric TED is also frequently seen. Thickening of the extraocular muscles (inferior, medial, superior, and lateral, in order of frequency) without involvement of the associated tendons may be noted on orbital imaging. Isolated enlargement of lateral rectus muscles is highly atypical of TED and requires further work-up and possibly biopsy. Isolated enlargement of the superior rectus can occur in TED, but should be followed carefully for alternative causes.
Other. Reduced blink rate, significantly elevated IOP (especially in upgaze), injection of the blood vessels over the insertion sites of horizontal rectus muscles, superior limbic keratoconjunctivitis, superficial punctate keratopathy, or infiltrate or ulceration from exposure keratopathy, afferent pupillary defect, dyschromatopsia, optic nerve swelling/pallor.
Systemic Signs
Hyperthyroidism is common (at least 80% of patients with TED). Symptoms include a rapid pulse, hot and dry skin, diffusely enlarged thyroid gland (goiter), weight loss, muscle wasting with proximal muscle weakness, hand tremor, pretibial dermopathy or myxedema, cardiac arrhythmias, change in bowel habits. Some patients are hypothyroid (5% to 10%) or euthyroid (5% to 10%). Euthyroid patients should undergo thyroid function testing every 6 to 12 months; a significant proportion will develop thyroid abnormalities within 2 years. TED does not necessarily follow the associated thyroid dysfunction and may occur months to years before or after the thyroid dysfunction. The clinical progression of TED also has only minor correlation with control of the thyroid dysfunction.
Concomitant myasthenia gravis with fluctuating double vision and ptosis may occur in a minority of patients. Always ask about bulbar symptoms (e.g., dysphagia, dysphonia, difficulty with breathing, weakness in proximal muscles, etc.) and fatigue in patients with suspected myasthenia gravis.
Differential Diagnosis of Upper Eyelid Retraction
Previous eyelid surgery or trauma may produce eyelid retraction or eyelid lag.
Severe contralateral ptosis may produce eyelid retraction because of Hering’s Law, especially if the nonptotic eye is amblyopic.
Third cranial nerve palsy with aberrant regeneration: The upper eyelid may elevate with downward gaze, simulating eyelid lag (pseudo-von Graefe sign). Ocular motility may be limited, but results of forced duction testing and orbital imaging are normal. Eyelid retraction is typically accentuated in adduction or in downgaze. SEE 10.6, ABERRANT REGENERATION OF THE THIRD NERVE.
Parinaud syndrome: Eyelid retraction and limitation of upward gaze may accompany convergence-retraction nystagmus and mildly dilated pupils that react poorly to light with an intact near response (light-near dissociation).
Work-Up
History: Duration of symptoms? Pain? Change in vision? Known history of cancer or thyroid dysfunction? Smoker? Last mammogram, chest x-ray (especially in smokers), prostate examination?
Complete ocular examination to evaluate for exposure keratopathy (slit lamp examination with fluorescein staining) and optic nerve compression (afferent pupillary defect, dyschromatopsia, optic nerve edema, automated perimetry). Extraocular motility (versions and ductions). Diplopia is measured with prisms or Maddox rod (SEE APPENDIX 3, COVER/UNCOVER AND ALTERNATE COVER TESTS AND 10.7, ISOLATED FOURTH NERVE PALSY). Proptosis is measured with a Hertel exophthalmometer. Check IOP in both primary and upgaze (increase in upgaze correlates with severity of inferior rectus muscle enlargement in TED). Dilated fundus examination with optic nerve assessment. Automated perimetry in cases of suspected optic neuropathy.
Imaging: CT of the orbit (axial and coronal views without contrast) is performed when presentation is atypical (e.g., all cases of unilateral proptosis or any bilateral proptosis without upper eyelid retraction), or in the presence of severe congestive orbitopathy or optic neuropathy. CT in TED varies from patient to patient. In patients with restrictive strabismus and minimal proptosis (“myogenic variant”) imaging will show thickened extraocular muscles without the involvement of the associated tendons. In patients with full or nearly full extraocular motility, severe proptosis, and exposure keratopathy (“lipogenic variant”), increased fat volume with minimal muscle involvement is typical. OCT may be helpful in cases of suspected optic neuropathy.
Thyroid function tests (TFTs) (T3, T4, TSH). These may be normal. TSI is sometimes ordered and can be followed over time, but the clinical significance of this test remains unclear.
Work-up for suspected myasthenia gravis is necessary in selected cases. SEE 10.11, MYASTHENIA GRAVIS.
Treatment
Smoking cessation: All patients with TED who smoke must be explicitly told that continued tobacco use increases the risk of progression and the severity of the orbitopathy. This conversation should be clearly documented in the medical record.
Refer the patient to a medical internist or endocrinologist for management of systemic thyroid disease, if present. If TFTs are normal, the patient’s TFTs should be checked every 6 to 12 months. Not infrequently, a euthyroid patient with TED will have an elevated TSI.
Treat exposure keratopathy with artificial tears and lubrication or by taping eyelids closed at night (SEE 4.5, EXPOSURE KERATOPATHY). Goggles at night may be helpful. The use of topical cyclosporine drops for the treatment of ocular surface inflammation in TED is still under investigation, but is a reasonable long-term treatment option if dry eye syndrome is present.
Treat eyelid edema with cold compresses in the morning and head elevation at night. This management may not be very effective. Avoid diuretics.
Indications for orbital decompression surgery include: Optic neuropathy, worsening or severe exposure keratopathy despite adequate treatment, globe luxation, uncontrollably high IOP, morbid proptosis.
A stepwise approach is used for surgical treatment, starting with orbital decompression (if needed), followed by strabismus surgery (for significant strabismus, if present), followed by eyelid surgery. Alteration of this sequence may lead to unpredictable results. Note that only a minority of patients with TED will need to undergo the entire surgical algorithm.
The following recommendations are somewhat controversial:
Corticosteroids: During the acute inflammatory phase, prednisone 1 mg/kg p.o. daily, tapered over 4 to 6 weeks, is a reasonable temporizing measure to improve proptosis and diplopia in preparation for orbital decompression surgery. There is evidence that the use of pulsed intravenous corticosteroids followed by a course of oral corticosteroids may result in better long-term control of TED with fewer systemic side effects than oral corticosteroids and is a reasonable option to offer patients in the acute phase of TED; other experts questions the long-term efficacy of this regimen. Periorbital corticosteroid injections are also used by some experts, but may be suboptimal to oral corticosteroids. Chronic systemic corticosteroids for long-term
management should be avoided because of the systemic side effects.
Orbital radiation: The use and efficacy of orbital radiation in the management of TED remains controversial. It may be used as a modality in the acute inflammatory phase of TED or as a means to limit progression and provide long-term control. Radiation therapy appears to decrease the severity and progression of restrictive strabismus in patients with active TED; efficacy in managing other aspects of TED (including optic neuropathy) has not been proved definitively, but is advocated by some experts. Radiation therapy should be used with caution in patients with diabetes, as it may worsen diabetic retinopathy, and in vasculopaths, as it may increase the risk of radiation retinopathy or optic neuropathy. All patients offered radiation therapy should be informed of the potential risks.
If used, radiation is best performed according to strict protocols with carefully controlled dosage and shielding under the supervision of a radiation oncologist familiar with the technique. Typically, a total dose of 2,000 cGy is administered in 10 to 14 fractions over 2 weeks. Treatment may transiently exacerbate inflammatory changes and an oral prednisone taper may mitigate these symptoms. Improvement is often seen within a few weeks of treatment, but may take several months to attain maximal effect.
Selenium supplementation: Data from Europe has concluded that the use of selenium supplementation (an antioxidant) reduces the severity and progression of mild-to-moderate TED. It remains unclear whether this finding is applicable in the United States, where no dietary selenium deficiency (as is present in certain European countries) exists. It is reasonable to offer this therapy to women with mild-to-moderate, active TED at a dose of 100 μg p.o. b.i.d. Caution should be used in the use of selenium supplementation in men, especially with a family history of prostate cancer; some studies have suggested an increased risk of prostate cancer in males with high selenium levels, although this issue does not appear to have been settled conclusively.
Biologics: Limited data are available on the use of biologic agents (rituximab, infliximab, adalimumab, etc), with some studies showing efficacy and others finding none. Their use as primary therapy in lieu of more conventional modalities is, at present, off-label and controversial. Furthermore, there appears to be little consensus as to the most effective, specific biologic target in TED.
Visual loss from optic neuropathy: Treat immediately with prednisone 1 mg/kg/day with close monitoring. In cases of severe visual loss, admission for pulsed intravenous therapy may be indicated. Radiation therapy may be offered for mild-to-moderate optic neuropathy, with the understanding that there is typically a lag in the treatment effect. Posterior orbital decompression surgery (for mild-to-severe optic neuropathy), either medial or lateral, is essential and usually effective in rapidly reversing or stabilizing the optic neuropathy. Anterior orbital decompression is usually ineffective in treating TED optic neuropathy.
Follow-Up
Optic nerve compression requires immediate attention and close follow-up.
Patients with advanced exposure keratopathy and severe proptosis also require prompt attention and close follow-up.
Patients with minimal-to-no exposure problems and mild-to-moderate proptosis are reevaluated every 3 to 6 months. Because of the potential risk of optic neuropathy, patients with restrictive strabismus may be followed more frequently.
Patients with fluctuating diplopia or ptosis should be evaluated for myasthenia gravis (SEE 10.11, MYASTHENIA GRAVIS).
All patients with TED are instructed to return immediately with any new visual problems, worsening diplopia, or significant ocular irritation. All smokers with TED must be reminded to discontinue smoking at every office visit, and appropriate referral to their primary physician for a smoking cessation program is indicated.
7.2.2 Idiopathic Orbital Inflammatory Syndrome
SYNONYMS: INFLAMMATORY ORBITAL PSEUDOTUMOR
Symptoms
May be acute, recurrent, or chronic. An explosive, painful onset is the hallmark of IOIS, but is present
in only 65% of patients. Pain, prominent red eye, “boggy” pink eyelid edema, double vision, or decreased vision. Children may have concomitant constitutional symptoms (fever, headache, vomiting, abdominal pain, lethargy) and bilateral presentation, neither of which is typical in adults.
in only 65% of patients. Pain, prominent red eye, “boggy” pink eyelid edema, double vision, or decreased vision. Children may have concomitant constitutional symptoms (fever, headache, vomiting, abdominal pain, lethargy) and bilateral presentation, neither of which is typical in adults.
Signs
Critical. Proptosis and/or restriction of ocular motility, usually unilateral, typically of explosive onset. On imaging studies, soft tissue anatomy is involved in varying degrees. The extraocular muscles are thickened in cases of myositis; involvement of the tendon may occur, but is by no means essential or pathognomonic. The sclera (in posterior scleritis), Tenon capsule (in tenonitis), orbital fat, or lacrimal gland (in dacryoadenitis) may be involved. The paranasal sinuses are usually clear.
Other. Boggy, pink eyelid erythema and edema, conjunctival injection and chemosis, lacrimal gland enlargement or a palpable orbital mass, decreased vision, uveitis, increased IOP, hyperopic shift (typically in posterior scleritis), optic nerve swelling or atrophy (uncommon).
Differential Diagnosis
Orbital cellulitis and/or abscess.
TED.
Other noninfectious orbital inflammatory conditions: sarcoidosis, GPA, IgG4-related orbitopathy, amyloidosis, Churg–Strauss syndrome, polyarteritis nodosa, Sjögren syndrome, rheumatoid arthritis, systemic lupus erythematosus, histiocytosis, etc.
Lymphoproliferative disease (including lymphoma).
Primary orbital malignancy (e.g., rhabdomyosarcoma).
Metastasis.
Leaking dermoid cyst.
Lymphangioma with acute hemorrhage.
Spontaneous orbital hemorrhage.
Necrotic choroidal melanoma.
Work-Up
SEE 7.1, ORBITAL DISEASE, for general orbital work-up.
History: Previous episodes? Any other systemic symptoms or diseases? History of cancer? Smoking? Last mammogram, chest x-ray, colonoscopy, prostate examination? History of breathing problems? A careful review of systems is warranted. Fever, night sweats, weight loss?
Complete ocular examination, including color vision, extraocular motility, exophthalmometry, IOP, and dilated funduscopic evaluation.
Vital signs, particularly temperature.
Imaging: Orbital CT (axial, coronal and parasagittal views) with contrast: may show a thickened posterior sclera (the “ring sign” of 360 degrees of scleral thickening), orbital fat or lacrimal gland involvement, or thickening of the extraocular muscles (± their tendons). Bony erosion is very rare in IOIS and warrants further work-up.
Blood tests as needed (e.g., bilateral or atypical cases): Westergren ESR, CBC with differential, ANA, ACE, cANCA, pANCA, LDH, IgG4/IgG levels, BUN/creatinine, and fasting blood sugar/hemoglobin A1c (before instituting systemic corticosteroids). If sarcoidosis is suspected, consider chest CT which is significantly more sensitive than chest x-ray (CXR). Mammography and prostate evaluation are warranted in specific or atypical cases.
If possible, perform incisional biopsy of involved orbital tissue if easily accessible with minimal morbidity before instituting corticosteroid therapy (corticosteroid therapy may mask the true diagnosis). The lacrimal gland is often involved in IOIS and is relatively easy to access surgically; strong consideration should be given to biopsy all cases of suspected inflammatory dacryoadenitis. However, biopsy of other orbital structures (extraocular muscle, orbital apex) is typically avoided in cases of classic IOIS because of the potential surgical risks; biopsy of these structures is reserved for atypical or recurrent cases. Always be suspicious for metastatic disease in any patient with a history of cancer.
Treatment
Prednisone 1 to 1.2 mg/kg/day as an initial dose in adults and children, along with gastric
prophylaxis (e.g., ranitidine 150 mg p.o. b.i.d., omeprazole 40 mg p.o. daily). All patients are warned about potential systemic side effects and are instructed to follow up with their primary physicians to monitor blood sugar and electrolytes.
Low-dose radiation therapy may be used when the patient does not respond to systemic corticosteroids, when disease recurs as corticosteroids are tapered, or when corticosteroids pose a significant risk to the patient. Radiation therapy should only be used once orbital biopsy, if anatomically and medically feasible, has excluded other etiologies.
Steroid-sparing agents (e.g., methotrexate, cyclophosphamide, etc.) in cases that do not respond to or recur with corticosteroid therapy. Biopsy of affected tissue, when feasible, is indicated to rule out malignancy.
Biologic therapy may be considered in cases that fail other modalities. The efficacy of specific biologic agents (e.g., CD20 antibody, TNF antibody, etc.) in IOIS is not known.
Follow-Up
Reevaluate in 1 to 2 days. Patients who respond dramatically to corticosteroids are maintained at the initial dose for 3 to 5 days, followed by a slow taper to 40 mg/day over 2 weeks, and an even slower taper below 20 mg/day, usually over several weeks. If the patient does not respond dramatically to appropriate corticosteroid doses, biopsy should be strongly considered. Recurrences of IOIS are not uncommon, especially at lower corticosteroid doses.
References
Bradley EA, Gower EW, Bradley DJ, et al. Orbital radiation for graves ophthalmopathy: A report by the American Academy of Ophthalmology. Ophthalmology. 2008;115(2):398–409.
Marcocci C, Kahaly GJ, Krassas GE, et al. Selenium and the course of mild Graves’ orbitopathy. N Engl J Med. 2011;364(20):1920–1931.
7.3 Infectious Orbital Disease
7.3.1 Orbital Cellulitis
Symptoms
Red eye, pain, blurred vision, double vision, eyelid and/or periorbital swelling, nasal congestion/discharge, sinus headache/pressure/congestion, tooth pain, infra- and/or supraorbital pain, or hypesthesia.
Signs
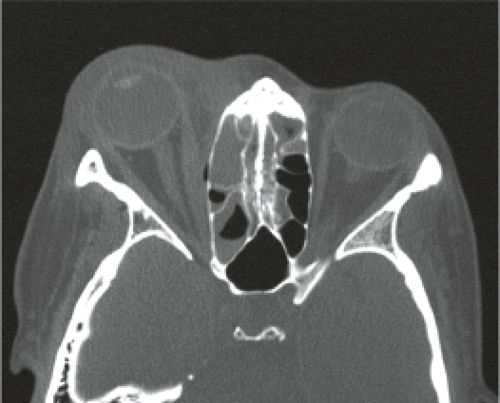
(See Figures 7.3.1.1 and 7.3.1.2.)
Critical. Eyelid edema, erythema, warmth, and tenderness. Conjunctival chemosis and injection, proptosis, and restricted extraocular motility with pain on attempted eye movement are usually present. Signs of optic neuropathy (e.g., afferent pupillary defect, dyschromatopsia) may be present in severe cases.
Other. Decreased vision, retinal venous congestion, optic disc edema, purulent discharge,
decreased periorbital sensation, fever. CT scan usually shows an adjacent sinusitis (typically at least an ethmoid sinusitis), possibly a subperiosteal orbital collection.
decreased periorbital sensation, fever. CT scan usually shows an adjacent sinusitis (typically at least an ethmoid sinusitis), possibly a subperiosteal orbital collection.
Etiology
Direct extension from a paranasal sinus infection (especially ethmoiditis), focal periorbital infection (e.g., infected hordeolum, dacryoadenitis, dacryocystitis, panophthalmitis), or dental infection.
Sequela of orbital trauma (e.g., orbital fracture, penetrating trauma, retained intraorbital foreign body).
Sequela of eyelid, orbital, or paranasal sinus surgery.
Sequela of other ocular surgery (less common).
Vascular extension (e.g., seeding from a systemic bacteremia or locally from facial cellulitis via venous anastomoses).
Extension from a septic cavernous sinus thrombosis.
 NOTE: In cases of unsuspected retained foreign body, cellulitis may develop months after injury (SEE 3.12, INTRAORBITAL FOREIGN BODY).
NOTE: In cases of unsuspected retained foreign body, cellulitis may develop months after injury (SEE 3.12, INTRAORBITAL FOREIGN BODY).
Organisms
Adult: Staphylococcus species, Streptococcus species, Bacteroides species.
Children: Haemophilus influenzae (rare in vaccinated children).
Following trauma: Gram-negative rods.
Dental abscess: Mixed, aggressive aerobes and anaerobes.
Immunocompromised patients (diabetes, chemotherapy, HIV infection): Fungi including those that produce zygomycosis infections (e.g., Mucor) and Aspergillus.
Work-Up
SEE 7.1, ORBITAL DISEASE, for a nonspecific orbital work-up.
History: Trauma or surgery? Ear, nose, throat, or systemic infection? Tooth pain or recent dental abscess? Stiff neck or mental status changes? Diabetes or an immunosuppressive illness?
Complete ophthalmic examination to evaluate for orbital signs including afferent pupillary defect, restriction or pain with ocular motility, proptosis, increased resistance to retropulsion, elevated IOP, decreased color vision, decreased skin sensation, or an optic nerve or fundus abnormality.
Check vital signs, mental status, and neck flexibility. Check for preauricular or cervical lymphadenopathy. Evaluate nasal passages for signs of eschar/fungal involvement in diabetic, acidotic, or immunocompromised patients.
Imaging: CT scan of the orbits and paranasal sinuses (axial, coronal, and parasagittal views, with contrast if possible) to confirm the diagnosis and to rule out a retained foreign body, orbital or SPA, paranasal sinus disease, cavernous sinus thrombosis, or intracranial extension.
Laboratory studies: CBC with differential and blood cultures.
Explore and debride any penetrating wound, if present, and obtain a Gram stain and culture of any drainage (e.g., blood and chocolate agars, Sabouraud dextrose agar, thioglycolate broth). Obtain CT before wound exploration to rule out skull base foreign body.
Consult neurosurgery for suspected meningitis for management and possible lumbar puncture. If paranasal sinusitis is present, consider consultation with otorhinolaryngology for possible surgical drainage. Consider an infectious disease consultation in atypical, severe, or unresponsive cases. If a dental source is suspected, oral maxillofacial surgery should be consulted
urgently for assessment, since infections from this area tend to be aggressive, potentially vision threatening, and may spread into the cavernous sinus.
 NOTE: Zygomycosis is an orbital, nasal, and sinus disease occurring in diabetic or otherwise immunocompromised patients. Typically associated with severe pain and external ophthalmoplegia. Profound visual loss may rapidly occur. Metabolic acidosis may be present. Sino-orbital zygomycosis is rapidly progressive and life-threatening. SEE 10.10, CAVERNOUS SINUS AND ASSOCIATED SYNDROMES (MULTIPLE OCULAR MOTOR NERVE PALSIES).
NOTE: Zygomycosis is an orbital, nasal, and sinus disease occurring in diabetic or otherwise immunocompromised patients. Typically associated with severe pain and external ophthalmoplegia. Profound visual loss may rapidly occur. Metabolic acidosis may be present. Sino-orbital zygomycosis is rapidly progressive and life-threatening. SEE 10.10, CAVERNOUS SINUS AND ASSOCIATED SYNDROMES (MULTIPLE OCULAR MOTOR NERVE PALSIES).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree