FIGURE 10.1 Placement of the Needle in Greater Palatine Foramen for a Greater Palatine Nerve Lock.
GP, Greater palatine. (The Anatomical Basis of Dentistry; 2011. Applied Anatomy, fig. 11.7, pii: B978-0-323-06807-9.00011-9.)
• Empiric treatment should include anaerobic coverage
• Pathogenesis: occurs either from uncontrolled dental caries → pulpal necrosis → periapical infection that spreads into the alveolar bone or a deep periodontal pocket → periodontal infection
• Periapical infections are the most common sources
• Clinical manifestation of infection is dependent upon muscle attachments (eg, buccinator and mylohyoid)
• Maxillary alveolar infections that erode the bone below the buccinator attachment will present with intraoral mucosal swelling (maxillary vestibular infection). Those that erode above the buccinator attachment will present as infraorbital swelling
• Mandibular alveolar infections involving the molars will often present with submandibular swelling because the roots of the molars are below the insertion of the mylohyoid. Alveolar infections of the premolars and anteriors may present with sublingual swelling because the roots are above the mylohyoid
Treatment of Odontogenic Infections
1. ABCs first (always), be prepared to secure emergency surgical airway as often as needed
2. Determine severity of infection
• Fever, tachycardia, tachypnea, and hypotension
• Trismus, dysphonia, dysphagia, inability to control secretions, and respiratory distress
• Identify potential high-risk space involvement
3. Assess host defenses
• Immunocompromised (steroids/chemotherapy, human immunodeficiency virus infection, diabetes, substance abuse, and malnutrition)
4. Provide surgical drainage and source control
• Incision and drainage of all affected spaces
• The source of the infection must be treated (ie, tooth extraction)
5. Antibiotic treatment
• Drainage and source control are the primary treatment
• All infections should be cultured
• Antibiotic treatment begins empirically with penicillin or clindamycin (if penicillin allergic)
• Severe infections may necessitate additional antibiotics (eg, piperacillin/tazobactam and metronidazole) for broader gram-negative or anaerobic coverage
• Antibiotic therapy tailored to culture results
Temporomandibular Joint Disorders
1. Myofascial pain
2. Internal derangement of temporomandibular joint (TMJ)
3. Osteoarthritis
4. Rheumatoid arthritis
5. Infectious arthritis
6. Traumatic arthritis
7. TMJ ankylosis
8. Condylar hyperplasia
9. Condylar hypoplasia
10. Mandibular dislocation
11. Idiopathic condylar resorption
Myofascial Pain
• Diagnosis: clinical exam, panoramic radiograph to rule out condylar/mandibular pathology
• Treatment:
• Phase 1, soft diet, intermittent moist heat, nonsteroidal antiinflammatory drugs (NSAIDs), and muscle relaxation; symptoms should improve within 1 month of treatment
• Phase 2, if not better after 1 month of phase 1, bite appliance and occlusal equilibration; should improve within 1 month of treatment
• Phase 3, physical and relaxation therapy
• Phase 4, stress reduction and psychotherapy ± pain management (about 10% of patients will not respond to escalation of therapy through phase III)
Internal Derangement of the Temporomandibular Joint
• History/exam: traumatic injury, parafunctional habits (tooth grinding and clenching), joint pain, joint clicking/popping/locking, and limited mouth opening
• Diagnosis: clinical exam, panoramic radiograph or maxillofacial computed tomography (CT) to rule out condylar/mandibular pathology, magnetic resonance imaging (MRI) of the TMJ to assess articular disc positioning (static and dynamic), and arthroscopy
• Wilkes classification3:
I Painless clicking, slightly forward disc that reduces on opening, and the joint contour appears normal on radiograph
II Occasional painful clicking/headache, early disc deformity, and forward position
III Frequent pain, joint tenderness, headache, locking, restricted motion, anterior disc, early reducing disc progresses to nonreducing, disc thickened, fibrillations, and no bone changes
IV Chronic pain, headache, restricted motion, nonreducing disc, and bony changes including degeneration, osteophyte, and adhesions, but no disc perforation
V Variable pain, joint crepitus, painful function, anterior disc displacement, perforated disc, adhesions, and multiple degenerative changes
• Treatment
• Clicking or popping: NSAIDs, soft diet, jaw rest, and bite appliance; consider surgical intervention (arthrocentesis, discplasty, or discectomy) if conservative measures fail
• Locking: anterior disc displacement without reduction (arthrocentesis, arthroscopic surgery, or discplasty); disc adhesion to articular eminence → arthrocentesis
Osteoarthritis of the Temporomandibular Joint
• History/exam: jaw trauma, constant aching pain that increases with function, parafunctional habits, decreased mouth opening, TMJ tenderness, and joint crepitus
• Diagnosis: clinical exam, panoramic radiograph or maxillofacial CT to assess for condylar changes (subcondylar sclerosis, condylar flattening, condylar erosion, and osteophyte formation); consider bone scan to assess for active disease process within condyles; rule out rheumatoid arthritis
• Treatment:
• Primary: NSAIDs, soft diet, limit jaw function, bite appliance, and establish a stable occlusion
• If not improvement after 6 months of primary treatment → TMJ arthroplasty
Rheumatoid Arthritis of the Temporomandibular Joint
• History/exam: bilateral TMJ swelling/tenderness, dull/aching pain, TMJ stiffness—worse in the morning, limited mouth opening, history of rheumatoid disease, and anterior open bite/condylar, or retrognathia in severe cases
• Diagnosis: panoramic radiograph, CT scan, MRI, rheumatoid factor, antinuclear antibody, and erythrocyte sedimentation rate (ESR)
• Treatment:
• Active disease: medical management (NSAIDs, soft diet, moist heat, range of motion exercises, and short-term steroids). If no improvement → disease-modifying therapy, coordinated with rheumatologist; if no improvement with disease-modifying therapy → surgical intervention (arthrocentesis and synovectomy)
• Inactive disease: surgical correction of ankylosis, open bite, or retrognathia as needed
Infectious Arthritis of the Temporomandibular Joint
• History/exam: history of tuberculosis/syphilis/gonorrhea, associated infection in the ear/mandible/parotid gland/pharynx, fever or malaise, TMJ pain, swelling, redness, and tenderness
• Diagnosis: clinical exam, panoramic radiograph, MRI, joint aspiration for culture and Gram stain, complete blood count (CBC) with differential, and ESR
• Treatment:
• Empiric antibiotics (penicillin for simple infections and third-generation cephalosporin for GNRs)
• Joint aspiration or incision and drainage
• If improvement → 2 weeks of antibiotics and TMJ physical therapy once active issues are resolved
• If no improvement → change antibiotics based on cultures, consider intravenous (IV) antibiotic therapy and surgical debridement
Traumatic Arthritis of the Temporomandibular Joint
• History/exam: trauma to mandible/TMJ, TMJ pain and tenderness, and limited motion
• Diagnosis: panoramic radiograph ± CT scan
• Treatment: NSAIDs, intermittent moist heat, soft diet, steroid injection, and jaw rest
• If improvement → jaw physical therapy to prevent ankylosis
• If no improvement → arthrocentesis
Temporomandibular Joint Ankylosis
• History/exam: history of trauma or infection to the TMJ, facial asymmetry, and trismus
• Diagnosis: panoramic radiograph, maxillofacial CT with three-dimensional reconstructions—consider angiography if a large ankylotic mass is present with possible intimate association with internal maxillary artery or pterygoid plexus
• Treatment:
• Pseudoankylosis (postsurgical scar, radiation fibrosis, coronoid hyperplasia, osteochondroma, untreated zygomatic arch fracture, paramandibular neoplasia, myositis ossificans, and psychogenic) → site-specific treatment
• Ankylosis: mechanical dilation of jaws with physical therapy or appliance (eg, Therabite) if onset is recent. If unsuccessful or for long-standing ankylosis → surgical correction with resection of the ankylotic mass and reconstruction of the ramus-condyle unit (bone graft, distraction osteogenesis, and alloplastic reconstruction), followed by orthognathic surgery or facial aesthetic surgery to achieve facial balance
Condylar Hyperplasia
• History/exam: facial asymmetry (usually starting in puberty), deviation of chin point away from the affected side, crossbite or open bite malocclusion, prognathic appearance, and asymmetric mandibular projection
• Diagnosis: panoramic radiograph, anterior-posterior and lateral cephalograms, review of historical photographs to document time course and evolution of deformity, CT scan, and technetium-99 (Tc99) bone scan to assess activity and growth
• Treatment: based on Tc99 bone scan
• Positive bone scan: partial condylectomy on the affected side with compensatory contralateral mandibular osteotomy, inferior-border contour correction, and possible genioplasty
• Negative bone scan: orthodontic treatment to address the dental component of malocclusion with subsequent orthognathic surgery and contour correction
Condylar Hypoplasia
• History/exam: history of mandibular trauma, inflammation, or radiation. Facial deformity with chin point deviation toward the affected side, micrognathia, mandibular contour asymmetry, and exaggerated antigonial notching
• Diagnosis: clinical exam, panoramic radiograph, anterior-posterior and lateral cephalograms, and CT scan
• Treatment: based on growth
• Still growing: costochondral graft or distraction osteogenesis
• Done growing: orthodontics → orthognathic surgery or genioplasty/contour correction
Mandibular Dislocation
• History/exam: external trauma, wide mouth opening (sudden or prolonged), joint subluxation, muscular disease, and open lock
• Diagnosis: clinical exam and panoramic radiograph or CT scan
• Treatment: based on time course
• Acute: manual reduction and immobilization (Intermaxillary Fixation or head wrap for 5-7 days)
• Chronic: manual reduction under general anesthesia; if unsuccessful → manual reduction with angle traction wires; if unsuccessful → temporalis myotomy, if unsuccessful → subcondylar osteotomy or condylectomy
Idiopathic Condylar Resorption
• History/exam: history of orthodontic treatment or orthognathic surgery, female predilection (age 15-35 years, “Cheerleader” syndrome), class II skeletal profile, class II malocclusion, high mandibular plane angle, and anterior open bite
• Diagnosis: clinical exam, panoramic radiograph, CT scan, and rule out rheumatoid arthritis, scleroderma, and other autoimmune processes
• Treatment: based on Tc-99 bone scan (Fig. 10.2)
• Positive scan: delay treatment until scan is negative
• Negative scan: orthognathic surgery ± condylectomy with TMJ reconstruction
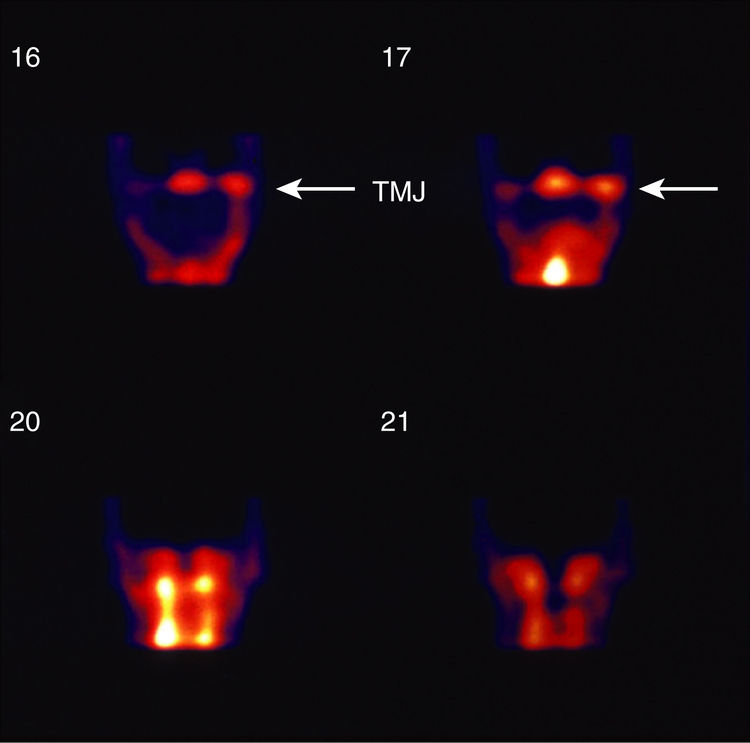
FIGURE 10.2 Technetium-99m Bone Scan.
A nuclear medicine bone scan evaluates metabolic activity in the condyles. The bone scan is sensitive to increased activity, and it serves as a guide for determining the stability of the asymmetry. (Farrell BB, Tucker MR. Mandibular asymmetry: diagnosis and treatment considerations. In: Bagheri SC, Bell RB, Khan HA, eds. Current Therapy in Oral and Maxillofacial Surgery. Philadelphia, PA: Saunders; 2012:671-684, fig. 80.8.)
Common Odontogenic Cysts and Tumors4,5
1. Radicular (periapical) cyst
2. Dentigerous cyst
3. Residual cyst
4. Lateral periodontal cyst
5. Eruption cyst
6. Traumatic bone cyst
7. Odontogenic keratocyst (OKC)
8. Calcifying epithelial odontogenic tumor (CEOT, Pindborg tumor)
9. Clear cell odontogenic carcinoma (clear cell odontogenic tumor)
10. Adenomatoid odontogenic tumor
11. Odontogenic myxoma
12. Calcifying odontogenic cyst (Gorlin cyst)
13. Ameloblastoma
14. Ameloblastic carcinoma
15. Ameloblastic fibroma
16. Ameloblastic fibro-odontoma
17. Odontoma
Radicular (Periapical) Cyst
• Round or oval lesion that arises from residual odontogenic epithelium and nonvital pulp
• Treatment: enucleation of cyst, endodontic treatment, or extraction of tooth
Dentigerous Cyst (Fig. 10.3)
• Develops in relationship to the crown of the erupting tooth
• Uni- or multilocular
• Most common in the third molar and maxillary canine regions
• Treatment: removal of the impacted tooth and enucleation or decompression of the cyst
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


