19 Oral Cavity Disorders in Geriatric Patients
 Introduction
Introduction
In 1900, there were 3.1 million people aged 65 and over in the United States. As the population 65 years and over steadily increased throughout the 20th century, the older population reached 40.3 million in 2010. Although there was an increase in overall population of ~ 10% between 2000 and 2010, those 65 years and over increased by 15%.1
As people live longer, there will be an increase in chronic conditions and illnesses that will affect both systemic and oral health.2,3 Arthritis, hypertension, heart disease, sinus diseases, and diabetes are some of the most common chronic diseases in the elderly. All of these conditions, and in many instances their treatments, can have oral consequences.
The effects of oral diseases are not necessarily limited to the oral cavity. Oral pathogens can cause immediate systemic complications (e.g., aspiration pneumonia, bacteremia) or, by complex immunologic pathways, may be associated with long-term problems (e.g., coronary heart disease and cerebrovascular disorders).4–7
This chapter reviews age-related changes in oral tissues and common oral conditions in the geriatric population, as well as the influence of systemic diseases and their treatments.
 Oral Mucosa
Oral Mucosa
Age-Related Changes
The clinical appearance of the oral mucosa is most commonly the result of recurrent mild trauma from cheek biting, chronic mucosal disease such as lichen planus, tobacco use, and increased friction as a result of salivary hypofunction. Histological changes may include epithelial thinning, loss of submucosal elastin and fat, and increased fibrotic connective tissues with degenerative alteration in collagen.8 The resulting clinical appearance may be one of dry, thin, smooth tissue, which is prone to further trauma and infection, particularly with denture use in the face of salivary hypofunction. Although oral mucosal immunity is believed to undergo some age-related changes, wound healing and regeneration of the oral mucosa are generally not affected (Fig. 19.1).9,10
Conditions
Many lesions are attributable to poorly fitting dentures. The persistent low-grade irritation caused by the prostheses moving and rubbing against tissue, or by patients wearing dentures 24/7 without cleaning or removing them regularly, can induce chronic inflammation, causing denture stomatitis, papillary hyperplasia, and even atrophy of the bone of the alveolar ridges. Hyperplastic reactions can also occur leading to the formation of redundant soft tissue (epulis fissuratum) or alteration of the mucosa such as frictional hyperkeratosis. Other conditions may be grouped as follows.
Benign Pigmented Mucosal Lesions
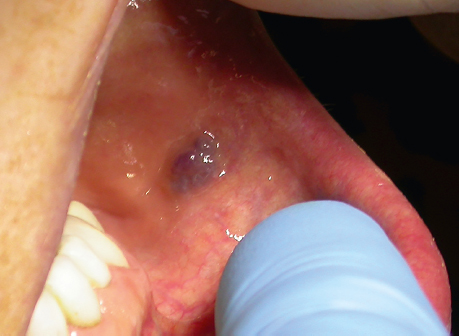
Conditions demonstrating change in mucosal color can include mucosal varices (venous lake) (Figs. 19.2 and 19.3), lingual varicosities, amalgam tattoos, melanosis from medications (e.g., Plaquenil), and melanotic macules.
Benign Soft Tissue Growths
Various benign soft tissue lesion may present in the oral cavity. Some common lesions that present as submucosal swellings include reactive lesions like pyogenic granuloma, epulis fissuratum, and fibromas. Other benign growths include lipoma, neuroma, papilloma, and granular cell tumor. Benign bone growths include tori and exostoses. Ectopic sebaceous glands are seen as submucosal creamy or white dots on the lips, buccal, and labial mucosa.
Vesiculobullous Diseases
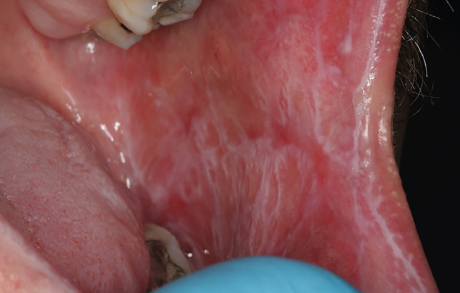
Lichen planus, pemphigus vulgaris, and cicatricial pemphigoid are some of the oral vesiculobullous diseases that can be found more frequently in the geriatric population. The most common of these is lichen planus, which is a recurrent, chronic, inflammatory, and immune-regulated mucocutaneous disorder that affects ~ 1% of the population, of which ~ 35% are aged 50 years or older (Fig. 19.4).11 In the oral cavity, there are two major forms of lichen planus, reticular and erosive. Only the erosive type needs to be treated, but all patients with oral lichen planus should be monitored at regular intervals due to a slightly increased risk of developing squamous cell carcinoma.
Lichenoid mucositis can be caused by a variety of medications commonly prescribed in older patients (e.g., acyclovir, gold salts, methyldopa, and thiazide diuretics) as well as over-the-counter products such as mouth rinses or chewing gum (Fig. 19.5).
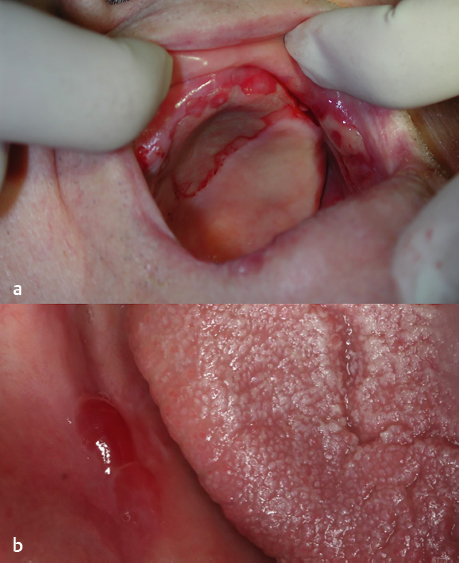
Pemphigus vulgaris is a potentially serious autoimmune disorder that usually affects individuals in their fifth and sixth decades (Fig. 19.6). Cicatricial pemphigoid is another immunologically mediated disorder; it affects primarily older women (Fig. 19.7).
The use of tissue-supported complete or partial dentures in any of these conditions can cause exacerbation of disease leading to vesicle formation, then rupture and formation of ulcers.
Recurrent Aphthous Stomatitis
This condition is less common in elderly people than in younger people; however, nutritional and hematologic deficiencies that are common in older adults can predispose to recurrent ulcers,12 as can gastrointestinal (GI) diseases such as Crohn disease, celiac disease, and Helicobacter pylori infection, which have been associated with aphthous stomatitis.
Fig. 19.5 Lichenoid mucositis. Erythema and erosion of the ventral lateral tongue in a patient with hepatitis C.
Fig. 19.7 An 83-year-old man with mucous membrane pemphigoid. (a) Ulceration of the anterior hard palate associated with the use of a full upper denture. (b) Vesicle formation on the lateral aspect of the mandibular alveolar ridge in the same patient
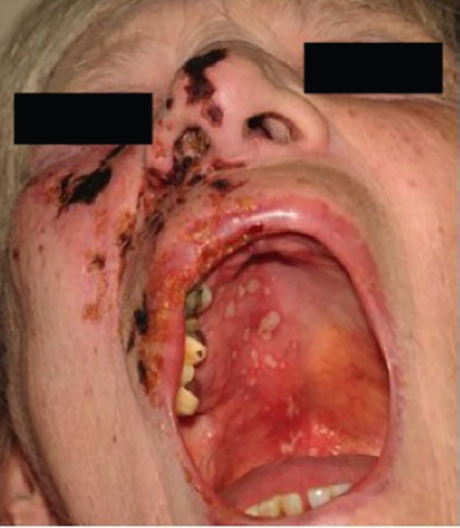
Oral Cancer
The incidence increases with age, with over 90% of all cases occurring in individuals 45 and older.13 Although there is a trend in recent years toward younger individuals, the American Cancer Society’s 2013 estimate for the average age of most people diagnosed with these cancers is 62. The most common risk factors are increased age and the use of tobacco and alcohol. In general, ~ 80% of oral cavity and pharynx cancers are squamous cell carcinoma.14 These lesions can appear as exophytic, poorly demarcated, and ulcerated, erythroplakic, and/or leukoplakic (Fig. 19.8). The most common premalignant oral lesion is leukoplakia, and the incidence of leukoplakic lesions undergoing malignant transformation rises sharply with age. Mortality rates for oral cancer also increase with age.15
Infections
The oral cavity of older adults is more likely to be susceptible to opportunistic infections due to age and disease-related changes in the oral and systemic immune system. The older patient is more likely to suffer systemic infection from viral, fungal, and bacterial organisms that invade, infect, and become latent in the hard and soft tissues of the oropharyngeal region.16
Herpes
Of the viral infections, the most common come from the herpes family. Herpes zoster (HZ) is a neurocutaneous disease that is caused by the reactivation of varicella-zoster virus (VZV) from a latent infection of dorsal sensory or cranial nerve ganglia. Although the initial infection typically occurs in childhood, reactivation of the latent virus may be secondary to immunosuppression, trauma, stress, or concurrent infections. Shingles, the result, is an acute condition with very painful and frequently incapacitating oral-facial vesicular lesions on the skin and mucous membranes in the areas that follow the unilateral distribution of ophthalmic, maxillary, or mandibular divisions of trigeminal sensory nerves (Fig. 19.9). The clinical presentation in an older adult will be similar to that in a younger person, but lesions may persist longer. The incidence of HZ increases sharply among patients aged ~ 50 to 60 years and continues an upward course in the decades > 60 years. In the Duke Established Populations for Epidemiological Studies of the Elderly,17 the lifetime risk of having HZ increased significantly with age even among elderly patients (odds ratio, 1.20 for every 5 year interval in patients > 65 years old; 95% confidence interval, 1.10–1.31). Extrapolating from HZ epidemiological studies, experts calculate the lifetime incidence rate of HZ to be 10 to 20% in the general population and as high as 50% of a cohort surviving to age 85 years. Not only is HZ considerably more common among elderly people, but so too is chronic HZ pain. This increased incidence of HZ and postherpetic neuralgia with age correlates with the simultaneous age-related decrease in VZV-specific cell- mediated immunity.18
In addition, recurrent infections from herpes simplex virus (HSV) may continue into old age. Although most commonly occurring on the lip, recurrent lesions may be seen on the skin of the face, the nose, and the ear. Intraoral recurrent lesions are restricted to the keratinized mucosa of the gingiva and hard palate and tend to present in crops of vesicles, which rupture into ulcerations and often will coalesce into one large ulcer. HSV 1 has historically been seen in the oral cavity, but increasingly HSV 2 infections are seen as well.
Candida Infections
Oral candidiasis, a common opportunistic infection of the oral cavity caused by an overgrowth of Candida, can result in difficulty eating as well as systemic infections. The most frequently identified risk factors for the development of oral candidiasis are the wearing of dentures, the degree of Candida colonization, a lack of oral hygiene, tobacco use, xerostomia, a deterioration in the general state of health, steroid use, and antibiotic therapy (Fig. 19.10).19
The bacteria that cause the most common oral mucosal infections are those associated with new and recurrent dental caries (Streptococcus mutans, Lactobacillus), periodontal diseases (Porphyromonas gingivalis, Treponema denticola), and acute and chronic salivary infections (Staphylococcus aureus, Streptococcus viridans).20
Treatments
Risk factors and treatment are summarized in Table 19.1. The treatment of traumatic oral lesions begins with the elimination of underlying factors such as the repair of a poorly fitting denture. Topical analgesics can be helpful along with antibiotics for secondary infections. Treatment of vesiculobullous disease and erosive lesions depends on the severity of the condition. Topical oral steroids may be mixed with oral adhesives like Orabase (Colgate-Palmolive Co., New York, NY). Systemic steroids and immunosuppressant agents may need to be considered. In the geriatric population, particular care must be exercised with such medications in the face of common concurrent medical issues such as heart disease, diabetes, osteoporosis, and depression.
Prevention of oral cancer begins with the elimination of established risk factors (e.g., the use of tobacco and alcohol). Early detection is a key component of successful treatment. Older edentulous individuals are four times less likely to see a dentist than are dentate individuals and should therefore be targeted for regular annual examinations for head and neck cancer.21,22 Dental management before, during, and after treatment of oral cancer is essential to prevent complications. Oral cancer is treated by surgery, chemotherapy, and radiotherapy. Common sequelae include stomatitis, dysphagia, pain, paresthesias, oral motor dysfunction, salivary hypofunction, and an increased risk of developing osteoradionecrosis.
Table 19.1 Risk factors and treatment of oral mucosa disease
Disease | Risk factors | Treatment |
Oral cancer | Tobacco, alcohol, human papilloma virus, human immunodeficiency virus, radiation, immunosuppression, leukoplakia, erythroplakia, family history, asbestos, printers (polycyclic aromatic hydrocarbons), betel quid | Surgery Radiation therapy Chemotherapy |
Traumatic lesions | Poorly fitting denture, chronic lip chewing, traumatic ulcers, secondary infection | Oral rinses Viscous lidocaine Diphenhydramine elixir Dyclonine Sucralfate Systemic medications Penicillin Amoxicillin Erythromycin |
Vesiculobullous and erosive disease | Drug reaction, trauma, allergy | Topical medications Fluocinonide gel Triamcinolone acetonide gel Clobetasol propionate gel Oral rinses Dexamethasone elixir Diphenhydramine elixir Dyclonine Sucralfate Systemic medications Prednisone Immunosuppressant Nutritional supplements Fluid intake |
Prevention of the spread of viral lesions in elderly patients can be accomplished by avoidance of individuals who have active infections. Although the lesions are usually self-limited, supportive measures are necessary to maintain adequate nutritional and fluid intake and to diminish pain. However, early diagnosis can diminish morbidity in older patients. In particular, immunocompromised adults are susceptible to recurrent herpes infections and require immediate and aggressive antiviral treatment. Acyclovir, valacyclovir, and famciclovir are common antiviral medications that can, in general, be used safely in older patients and are well tolerated. The drugs are excreted by the kidneys and should be dosed appropriately for patients with renal insufficiency. Randomized, controlled trials indicate that orally administered acyclovir (800 mg 5 times a day for 7 days), famciclovir (500 mg every 8 h for 7 days), and valacyclovir (1 g three times a day for 7 days) reduce acute pain and the duration of chronic pain in elderly patients with HZ who are treated within 72 hours of the onset of rash.23 Unfortunately, 20 to 30% of treated patients in antiviral trials had pain 6 months from HZ onset, indicating that patients who have been treated can develop postherpetic neuralgia. In the most recent trial of acyclovir and prednisone, time to uninterrupted sleep, return to daily activity, and cessation of analgesic therapy was significantly accelerated in patients who received corticosteroids.24 The patients in the trial had an average age of 60 years and no relative contraindications to corticosteroids such as hypertension, diabetes mellitus, or osteoporosis. Therefore, some experts advocate orally administered corticosteroids for otherwise healthy older adults with moderate to severe pain and no contraindications to corticosteroids.
Prevention of bacterial infections and candidiasis involves good oral and denture hygiene, the judicious use of antibiotics and immunosuppressants, and the elimination of underlying local and systemic etiologic factors such as salivary hypofunction, diabetes, or immunodeficiency. The use of antifungal creams, rinses, and lozenges is usually successful, but persistent infections require systemic antifungal agents. If a patient has a denture or other prosthesis, both the oral cavity (rinse, troches, etc.) and the prosthesis (antifungal denture bath) should be treated to limit fungal burden. Concurrent use of an antifungal (often needed only once or twice per day) is prudent when potent topical corticosteroids are used in patients with diabetes or severe salivary hypofunction or in immunocompromised patients to decrease the chance of developing thrush. Systemic antifungal agents will have limited effectiveness in patients with decreased or no salivary flow.
 Periodontium
Periodontium
Age-Related Changes
With the increasing retention of the natural dentition, the number of teeth in older adults at risk of developing periodontal disease is growing.25 Gingival recession and loss of periodontal attachment and alveolar bone are nearly universal age-related changes. Several systemic conditions and medications that are more prevalent among older adults have been linked with periodontal disorders.
Conditions and Treatments
Gingivitis is much more likely to develop in older patients because of oral and systemic factors. Dental plaque, gingival bleeding, and calculus accumulations develop as a result of softer diets, reduced oral motor activity, and salivary gland hypofunction. Advanced periodontal diseases have been associated with nonoral diseases such as pneumonia, bacteremia, infective endocarditis, coronary heart disease, and brain abscesses, and they may interfere with the treatment of systemic diseases.
There is some evidence that severe osteoporosis significantly reduces the bone mineral content of the jaws and that it may be associated with greater periodontal attachment loss and tooth loss.26 Studies have been conducted to evaluate the effect of hormone replacement therapy in modifying the periodontal conditions in postmenopausal women. The clinical significance of hormone replacement therapy in periodontal health is not well established.27
Medications and medical problems that are common among older adults have an adverse effect on periodontal health. Calcium channel blockers, phenytoin, and cyclosporine, which are prescribed frequently for older persons, have been associated with gingival overgrowth or hyperplasia.28 Diabetes, even when well controlled, is associated with increased risk of periodontal disease.29 The prevalence of diabetes among adults age 65 and older increased by more than 50% between 1997 and 2006.30 Oral mucocutaneous diseases such as erosive lichen planus and cicatricial pemphigoid can demonstrate the clinical appearance of desquamative gingivitis (Fig. 19.11).
If the periodontal disease is believed to arise from the patient’s medical conditions and their treatment, then a systemic approach to oral health management is required. Drug-induced gingival hyperplasia frequently requires surgical reduction along with plaque control and the consideration of alternative medication. Other dental issues commonly found in older patients, such as restoration problems, poorly fitting dentures, and caries need to be addressed as well.
Finally, there are oral and sociobehavioral factors that influence the progression of periodontal disease in elderly people. Irregular dental visits, smoking, psychosocial stress, and poor socioeconomic status all are predictors of periodontal attachment loss in older patients.31,32 Periodontal maintenance and prevention regimens are similar for all age groups but may require additional time, equipment, and recall visits to dental professionals depending on the functional and mental capacity of the individual. Periodontal health can be maintained with tooth brushing and flossing after each meal and with regularly scheduled professional dental examinations and cleanings. In older adults who are homebound, institutionalized, or physically and/or behaviorally compromised, all additional caregivers need to be made part of this routine. Dental professionals must be actively involved and must instruct caregivers on the proper use of oral and denture hygiene techniques for their patients.
 Dentition
Dentition
Age-Related Changes
With improvement in oral care, prevention, tooth preservation, and restoration major epidemiological changes have occurred over the past several decades in regard to retention of dentition. Only ~ 30% of adults aged ≥ 65 years are completely edentulous.33 Age-related changes are attributable to normal physiological processes and to pathological changes in response to functional and environmental stresses. Discoloration, loss of enamel, abrasion, and erosion are seen commonly.
Conditions and Treatments
Increases in caries in the elderly are influenced by two trends: a greater retention of teeth among elderly persons, and a decline in caries among younger people.34 Dental plaque is the primary source of microorganisms, which contribute to caries in the elderly. With diminished salivary gland function, disturbances in oral motor function, and difficulty in performing oral hygiene older patients are more susceptible to new and recurrent tooth decay. When detected early, caries can be restored with a variety of dental materials. In addition to pain and tooth loss, untreated caries can progress to cellulitis, abscess, and bacteremia.
Rigorous oral hygiene, including brushing and flossing after each meal, is the most important part of preventive care. The use of fluoride-containing rinses, gels, and varnishes can help in the remineralization of existing decay and the prevention of new caries.35 Regular dental visits for prophylaxis, examination, and early treatment of dental caries are also required. The treatment of coronal and root surface dental caries has been facilitated by the improvement in restorative materials. Cosmetic and implant dentistry has also made considerable advances that have implications for older adults.
Patients affected with medical conditions that are known to cause salivary hypofunction (e.g., Sjögren syndrome, diabetes, head and neck irradiation, Alzheimer disease) must be monitored more closely. Similarly, patients who are taking medications associated with salivary hypofunction (e.g., antidepressants, antihypertensives, antipsychotics) should be recalled more frequently than other patients to dental professionals. The older patient with salivary hypofunction requires rigorous oral hygiene practices with the addition of supplemental fluoride gels and rinses.
 Salivary Glands
Salivary Glands
Age-Related Changes
It was previously thought that changes in qualitative and quantitative salivary production were associated with normal aging. This may have been partly due to the common complaint of xerostomia (mouth dryness) in older people. Published work presents a conflicting picture of the effects of age on salivary flow. The different results are likely to be due primarily to the varying methodologies, including the age of the individuals, the number of individuals, the exclusion and inclusion criteria, cross-sectional rather than longitudinal design, method of stimulation (mechanical or chemical), and duration of collection period, all of which make comparisons between the studies difficult; but the age-old mantra of decreased salivation with increased age is not supported by the literature. Changes in anatomy and physiology, including sensation, with age can account for changes in salivary flow.36 In addition, no age-related decreases in the secretion of certain salivary constituents (e.g., total proteins, proline-rich proteins, lactoferrin, sodium, and potassium) are seen in a healthy elderly population. The loss of fluid-producing acinar cells increases the susceptibility of an older individual to salivary perturbations such as those caused by medications with anticholinergic side effects.37
Conditions and Treatments
The most common pathogens associated with acute salivary gland infections are Staphylococcus aureus and anaerobic bacteria. The predominant anaerobes include gram-negative bacilli (i.e., Prevotella spp, Porphyromonas spp, Fusobacterium spp) and Peptostreptococcus spp. Additionally, Streptococcus spp (including S. pneumoniae and S. pyogenes) and aerobic and facultative gram-negative bacilli (including Escherichia coli) have been reported. Aerobic and facultative gram-negative organisms are often seen in hospitalized patients. Organisms less frequently found are Haemophilus influenzae, Klebsiella pneumoniae, Salmonella spp, Pseudomonas aeruginosa, Treponema pallidum, Bartonella henselae, and Eikenella corrodens. Mycobacterium tuberculosis and atypical mycobacteria are rare causes of parotitis.38
Appropriate antibiotic therapy for salivary gland infections should be based on diagnostic culture and sensitivity testing, when possible. Hydration, the use of a sialogogue, massage of the infected gland, and the use of an amoxicillin and clavulanic acid (clindamycin if the patient is allergic to penicillin) can be started immediately. Diagnosis and treatment of salivary gland obstructions may require imaging tests (radiography, ultrasonography, sialography) and subsequent removal of the obstruction.
 Tongue
Tongue
Age-Related Changes
The tongue is a frequent site of oral soft tissue changes. Changes may range from varying forms of glossitis to mass formation. This section discusses various lingual changes that may be recognized in the elderly patient and, where appropriate, their associated treatments.
Conditions and Treatments
Median Rhomboid Glossitis
Median rhomboid glossitis is characterized by a rhomboid-shaped smooth atrophic erythematous mucosa with missing filiform papillae, located at the dorsal midline or paramedian of the tongue, just anterior to the circumvallate papillae on the dorsal midline of the tongue (Fig. 19.12). The area usually produces little symptoms other than occasional burning or itching. Men are affected three times more often than women. This lesion has traditionally been thought to be the result of a lack of fusion of the two lateral processes (lingual tubercles) resulting in a lack of coverage of the central structure formed from the first and second branchial arches, the tuberculum impar.39,40 However, there is also an association with candidal infections and a response to antifungals (e.g., nystatin, fluconazole, clotrimazole) given as a suspension or oral troche. Candida can be confirmed with a scraping or culture. More frequent Candida infections may be the cause of the higher incidence of median rhomboid glossitis in those with diabetes. Other surfaces of the mouth are characteristically spared. A possible premalignant or malignant phenomenon should be ruled out when the clinical aspects contradict those expected.
Atrophic Glossitis
The smooth, glossy appearance associated with atrophic glossitis is due to atrophy of the filiform papillae. In most cases atrophic glossitis is a manifestation of an underlying condition, many of which are summarized in the Table 19.2. Treatment can include nutrient replacement or treatment of the underlying condition.