Purpose
To report the visual and anatomic outcomes of a novel technique for the management of anterior corneal scarring using optical coherence tomography (OCT)–guided transepithelial phototherapeutic keratectomy (transepithelial PTK).
Design
Retrospective, consecutive case series.
Methods
The charts of 22 patients with anterior corneal scarring associated with irregularities in the Bowman layer who had undergone transepithelial PTK according to a novel protocol were reviewed. The protocol consisted of a preoperative OCT-measured depth-of-treatment calculation, followed by a dual excimer laser treatment profile set to achieve the desired refractive outcome while eliminating or reducing corneal scarring. The primary outcomes were change in best spectacle-corrected visual acuity (BSCVA) and change in corneal topography indices at 4 months after ablation.
Results
BSCVA (in logMAR) improved from a mean of 0.82 (0.61–1.02; 95% confidence interval) preoperatively to a mean of 0.40 postoperatively (0.19–0.61) ( P = 0.0070). All patients gained a minimum of 1 line of BSCVA postoperatively. Preoperative and postoperative corneal topographic indices showed significant improvement in corneal cylinder ( P = 0.0173) and projected visual acuity ( P = 0.0261) but not in the surface asymmetry index ( P = 0.0849) or the surface regularity index ( P = 0.0543). Postoperative spherical equivalent averaged 0.78 diopters (0.49–1.07) of error from the intended target refractive outcome. No complications were associated with the treatment, and no patients required or desired subsequent treatment with either repeat PTK or with more invasive surgery such as lamellar or penetrating keratoplasty.
Conclusions
OCT-guided transepithelial PTK using a dual ablation excimer laser profile can provide favorable results as well as predictable refractive outcomes in the treatment of corneal scarring associated with Bowman layer irregularities. Future investigations are warranted to further validate the technique reported in this study.
Phototherapeutic keratectomy (PTK) is a safe and efficacious modality for the treatment of opacities localized to more than one third of the superficial corneal stroma. In cases with irregular corneal surfaces, PTK may also enhance the cornea’s optical qualities and improve vision by smoothing the irregular corneal surface as well as avoiding the need for more invasive surgery such as lamellar or penetrating keratoplasty. Recently, new technologies, such as the Pentacam device (Oculus, Lynnwood, Washington, USA) and anterior segment optical coherence tomography (OCT) (Carl Zeiss Meditec, Dublin, California, USA), have improved preoperative prediction of the depth of corneal pathology and have determined more accurately the amount of corneal tissue to be removed during PTK.
Transepithelial PTK is a technique in which PTK is performed without the manual removal of the epithelium by superficial keratectomy but instead uses the excimer laser to photoablate the epithelial layer, which serves as a natural masking agent. Transepithelial PTK has been used to treat recurrent erosions, laser in-situ keratomileusis (LASIK) flap macrostriae, keratoconus (in combination with corneal collagen crosslinking), corneal stromal dystrophies and, more recently, corneal scarring. In cases with anterior corneal scarring or irregularities in the Bowman layer, OCT may provide useful clinical information that helps to determine the appropriate depth of ablation during transepithelial PTK.
While conventional epithelium-off PTK for anterior corneal scarring is being performed, intraoperative findings may reveal a visible “crater” or “divot” in the Bowman layer. Once the epithelium has been removed and a Bowman irregularity has been revealed, the laser ablation profile will transmit these subtle and focal irregularities down to a deeper level in the stroma, and they will persist to some degree once the cornea re-epithelializes. To mitigate against this problem, investigators have tried using various masking agents (eg, artificial tears or surgical sponges) to fill in or cover the irregular defect in order to provide for a more uniformly distributed ablation profile.
With the advent of OCT technology, clinicians now have the ability to determine preoperatively which patients are likely to develop intraoperative craters in the Bowman layer if traditional epithelium-off PTK is performed. In these cases, the authors hypothesize that the epithelium itself may act as an effective masking agent and allow for a more even distribution of the ablation pattern if preserved. This could result in lower amounts of postoperative irregular astigmatism by avoiding the propagation of the Bowman layer irregularities to a deeper level in the corneal stroma. In this study, the authors describe a novel technique that uses OCT imaging of the central cornea to guide a transepithelial excimer laser ablation algorithm in order to treat anterior corneal scars associated with an irregular Bowman layer, all while maintaining and controlling for refractive outcomes.
Methods
The Southwest Retina Specialists institutional review board (IORG0007600/IRB00009122) approved this retrospective chart review of consecutive cases in patients who underwent OCT-guided transepithelial PTK for anterior corneal scarring between January 2011 and February 2013. All research components adhered to the tenets of the Declaration of Helsinki and were conducted in accordance with human-subject research regulations and standards.
Inclusion Criteria
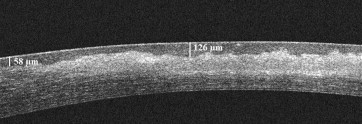
Subjects included in the study had undergone complete ophthalmologic examinations and had undergone OCT-guided transepithelial PTK for central corneal scarring that was associated with a significantly irregular Bowman layer. A significantly irregular Bowman layer was defined as follows: spectral domain OCT (Cirrus HD-OCT; Carl Zeiss Meditec, Dublin, California, USA) of the central 3 mm of cornea (1) exhibited a hyperintense signal that corresponded with scarring on clinical examination and (2) was associated with a variation in epithelial thickness by a minimum of a 33% increase from the baseline epithelial thickness, thus giving it the appearance of a crater or a divot scar ( Figure 1 ).
Optical Coherence Tomography Imaging and Measurements
Preoperative Cirrus HD-OCT of the central 3 mm of the cornea was performed in all subjects as follows. Multiple vertical and horizontal raster line scans (axial resolution 5 μm) were centered over the apex of the cornea and the following measurements were obtained: (1) maximum depth of the opacity; (2) maximum depth of the crater (ie, the depth to the Bowman layer, where the epithelium is at its thickest point); (3) baseline epithelial thickness (as ascertained from an area of the cornea where scarring is absent); and (4) the total central corneal thickness. Scans with signal strength less than 8 or scans that were noted to be significantly offset from the central cornea (as determined by inspection of the centration of the raster lines seen on the scout view) were rejected for use in the measurements and the analysis.
Dual Excimer Laser Photoablation Treatment Algorithm
All photoablations were performed by a single surgeon (S.W.R.). Off-label use of the Allegretto Wavelight Eye-Q 400 Hz (Alcon, Fort Worth, Texas, USA) platform was used to perform 2 wave-front–optimized ablation treatment profiles. First, the maximum depth of the patient’s scar (as measured on OCT) was used as the primary target ablation depth. A large optic zone (usually 7 mm) spherical myopic ablation was then calculated to ablate to the desired depth (including the epithelial thickness). Immediately following this, a secondary ablation was performed to control the refractive outcome by using a hyperopic ablation profile. This was calculated in the following way. The ablation depth for the baseline epithelial thickness (which is refractively neutral) was subtracted from the total of the myopic ablation depth. The patient’s preoperative spherical equivalent (SE) was then subtracted from the remaining myopic ablation treatment. Accounting for the surgeon-specific myopic ablation nomograms, the secondary spherical hyperopic ablation profile was used to bring the patient back to an SE near plano or any other desired refractive result.
The preoperative SE was ascertained by several methods: (1) previous prescriptions for glasses or contact lenses prior to the corneal scarring events; (2) manifest refraction results in those with good enough preoperative vision; and (3) the refractive status of the fellow eye. Pseudophakic patients were assumed to be plano unless known to be otherwise. All relevant historical data and clinical tests were used in combination to establish the final SE. (Astigmatic correction was not used in the laser ablation profiles because the majority of astigmatisms in these cases were irregular and were assumed to be related to the corneal scarring).
Patients were not given ablation treatment profiles that were calculated to leave the cornea with residual stromal beds of less than 275 μm. If the preoperative calculations anticipated violation of this restriction, the myopic portion of the ablation was decreased to accommodate for the 275 μm residual stromal-bed parameter, and the hyperopic portion of the ablation profile was also adjusted accordingly.
If the patient had corneal scarring that was too deep to eliminate entirely despite application of the largest myopic ablation profile allowed by the Allegretto Wavelight laser platform (−10 sphere at an optic zone of 7 mm, which ablates 163 μm of tissue), the ablation profile was done as deeply as possible and at least deeply enough to get to the maximal depth of the crater. If the patient had a moderate to high preoperative myopic SE, the patient may not have required the second ablation with the hyperopic treatment profile to achieve the desired refractive outcome.
Preoperative Routine
All patients with known or suspected herpes simplex virus keratitis were pretreated with oral acyclovir 400 mg by mouth twice daily 1 week prior to transepithelial PTK and continuing for a total of 3 months postoperatively. No cases of herpes zoster were included in the study.
Transepithelial PTK Surgical Technique
The excimer laser was programmed to deliver two separate ablation profiles, as described above. The patient was given topical anesthetic and prepared using Betadine 5% to the ocular fornices. The myopia profile was delivered first and was immediately followed by the hyperopic ablation (a delay of about 20 seconds between the two ablations). Following both ablations, mitomycin C 0.02% was applied to the stromal bed on an 8 mm diameter circular sponge for a total of 15 seconds, which was followed by vigorous ocular surface irrigation. A bandage contact lens was placed over the cornea at the end of the procedure.
Postoperative Routine
Patients were given ofloxacin 0.3% 1 drop 4 times a day for 1 week and prednisolone acetate 1% 4 times daily for 1 week, then twice daily for 1 week. The bandage contact lens was removed 3 to 5 days postprocedure. Additional follow-up included both 2-week and 4-month postoperative examinations.
Data Collection
The best spectacle-corrected visual acuity (BSCVA), the indices on the Tomey TMS-4 Corneal Topographer (Phoenix, Arizona, USA), and the maximal crater depth on OCT were collected at baseline and at the 4-month postoperative follow-up. The absolute value of the SE on postoperative refraction subtracted from the predicted SE refractive outcome was also recorded. The corneal topography indices measured included cylinder, projected visual acuity, surface asymmetry index, and surface regularity index.
Statistical Analysis
One-way analysis of variance was performed to compare the preoperative to the postoperative measurements of the BSCVA (logMAR), corneal topography indices and OCT crater depths. Mathematical software from the SAS Institute (Cary, North Carolina, USA) was used to perform statistical analysis. Results were considered statistically significant at the alpha <0.05 level.
Results
A total of 22 eyes of 20 patients met criteria for inclusion in the study. The various underlying pathologies responsible for the corneal scarring are detailed in Table 1 . The mean age of the subjects was 58.6 years (50.4–66.8; 95% CI); 59% were male and 41% female. Table 2 details the pertinent findings of the study. BSCVA (in logMAR) improved from 0.82 (0.61–1.02) to 0.40 (0.19–0.61) ( P = 0.0070). The mean baseline epithelial thickness was 51.6 μm, and the mean baseline maximum crater depth was 114.8 μm. This represented an overall average of a 55% variation in the baseline central corneal epithelial thicknesses. There was an 80% improvement in maximum crater depth postoperatively, with a mean of 12.5 μm residual crater depth, and 36% (8/22) of patients had resolution of the crater scar in its entirety. The mean postoperative SE was 0.78 (0.49–1.07) diopters (D) in error from the intended postoperative refractive target.
| Preoperative Diagnosis | Number of Patients (n = 22) |
|---|---|
| Herpes simplex virus keratitis | 9 |
| Bacterial keratitis | 9 |
| Trauma (including foreign body) | 2 |
| Other chronic ocular surface disease | 2 |
| Outcome Measurement | Preoperative Means (with 95% CI) | Postoperative Means (with 95% CI) | P value |
|---|---|---|---|
| Best spectacle-corrected visual acuity in LogMAR | 0.82 (0.61–1.02) | 0.40 (0.19–0.61) | 0.0070 |
| Topographic cylinder in diopters | 4.42 (3.54–5.30) | 2.90 (2.02–3.78) | 0.0173 |
| Topographic surface asymmetry index | 3.29 (2.58–4.01) | 2.41 (1.69–3.12) | 0.0849 |
| Topographic surface regularity index | 1.63 (1.37–1.90) | 1.27 (1.00–1.53) | 0.0543 |
| Topographic projected visual acuity in LogMAR | 0.36 (0.30–0.43) | 0.26 (0.19–0.32) | 0.0261 |
| Crater depth by optical coherence tomography in μm | 61.4 (49.5–73.5) | 12.5 (0.8–24.2) | <0.0001 |
All patients experienced a gain of at least 1 logMAR line of BSCVA during the study interval, and none of the patients experienced visually significant anisometropia or the effects of aniseikonia postoperatively. The corneal topography–measured cylinder and the projected visual acuity significantly improved, but the other corneal topographic indices were not statistically significant (although they trended toward improvement). None of the study subjects required (or requested) an additional treatment with repeat PTK or lamellar/penetrating keratoplasty. In addition, there were no cases of herpes simplex reactivation in any of the subjects during the study interval. In a subset analysis that excluded the 6 patients with poor visual potential unrelated to the cornea (three with advanced macular degeneration, two with dense cataracts, and one with a prior macula-off retinal detachment), the mean postoperative BSCVA improved from 0.54 to 0.20 ( P < 0.0001).
Case Example #1: Traumatic Corneal Foreign Body
A 53-year-old male with a history of a metallic corneal foreign body injury presented with monocular diplopia and 20/30 Snellen BSCVA in the affected eye. The patient’s preoperative OCT demonstrated a large corneal scar with crater formation ( Figure 2 ). To get as deeply as possible to the bottom of the crater, the initial myopic ablation profile was set at the maximum depth ablation profile for the excimer platform of −10.00 sphere with an optic zone of 7 mm, which removes a predicted total of 163 μm of tissue. Accounting for the baseline epithelial thickness, the first 3.25 D of this myopic ablation removed only epithelium (projected to be 58 μm) and did not contribute to the overall postoperative refractive outcome. Using our surgeon-specific nomogram, the remaining 6.75-sphere myopic ablation profile with an optic zone of 7 mm was calculated to result in an effective correction of 7.25 D of myopic treatment, which thereby induced 7.25 D of hyperopia in the patient. The operative eye was determined to have a preoperative SE of +1.00 D according to both the preoperative refraction and the historical refraction prior to injury. Therefore, the second ablation profile was set at maximum hyperopic correction for the excimer platform at +6.0 D at an optic zone of 6.5 mm, which provided exactly 6 D of correction according to our surgeon-specific nomogram. The mathematics anticipated that the resulting dual treatment excimer laser ablation profile would result in a total postoperative SE of 7.25 D of hyperopia induced, added to the 1.00 D of preoperative existing hyperopia and then subtracted from the 6 D of induced myopia in the second treatment, thereby equaling 2.25 D of postoperative hyperopia. The second (hyperopic) ablation was not expected to contribute much to the total ablation depth because the treatment was predominantly peripheral to the central 3 mm of the cornea ( Figure 3 and Figure 4 ).




