5 Operative Evaluation of the Geriatric Patient
 Introduction
Introduction
The American population is aging. In the next 25 years, the population of Americans age 65 years or older will double to ~ 72 million.1 Older Americans are more likely to need surgery than their younger counterparts. About half of adults age 65 and older will undergo a major surgical procedure.2 In the past 30 years, though, surgeries in the 65 and older cohort have increased by more than demographic trends alone might predict; in addition to emergent surgeries, patients in the 65 and older age group are becoming increasingly comfortable with elective surgeries to improve quality of life or treat disease burden.
In the field of otolaryngology, 14.3% of the patient population was age 65 or older in 2004, compared with 17.9% in 2010.3 The common pathologies in geriatric patients differ from those in younger age groups: 73% of geriatric diagnoses are otologic in nature, compared with just 32% of diagnoses in patients age 18 to 45 years.3 As the baby boomer generation ages, the percentage of the American population over 65 grows. These geriatric patients are more likely to undergo surgical procedures than previous generations, and these surgeries are increasingly more likely to be in the field of otolaryngology. In response to these changing dynamics, the American Society of Geriatric Otolaryngology was founded in 2007.
 Surgery in the Elderly
Surgery in the Elderly
The decision to operate in the geriatric population should be made with careful consideration and evaluation of potential risks and benefits. Despite the low-risk profile of numerous surgeries, the elderly are more likely to experience complications than their younger counterparts.4 Surgery is performed more frequently in the geriatric population, at a rate of 190 procedures per 100,000 for patients 65 and over, compared with 136 per 100,000 for those ages 40 to 64.2 Geriatric patients are more likely to require emergent surgery than younger patients,5 and nonelective procedures have higher rates of morbidity and mortality than elective operations. Elective surgery requires careful planning to minimize peri-operative morbidity and mortality: preoperative evaluation, perioperative monitoring, and postoperative management.
Head and neck surgery requires the same careful evaluation as other operative procedures. However, several unique considerations apply. For example, head and neck cancer may drastically affect both functionality and quality of life, and many head and neck cancer patients may be candidates for relatively aggressive cancer therapy.6 Both surgical and nonsurgical treatments may be worth exploring in the face of a large cancer burden, even if the patient has a relatively poor prognosis, because these procedures may lead to improvement in quality of life or symptom control.7 Geriatric patients with few comorbidities and generally good fitness have long-term outcomes similar to younger counterparts after aggressive head and neck cancer therapy. Age should not define their cancer treatment nor preclude geriatric patients from standard management.7
 General Considerations
General Considerations
The goals of treatment vary between patients. When deciding on an elective operation, it is important to elicit patient preferences and properly evaluate understanding of the procedure. This process should include a discussion of quality of life with and without surgical intervention as well as nonoperative treatment options. If surgical intervention is chosen, further counseling centers around the likelihood of achieving the desired surgical result, the estimated degree of symptom improvement, the risk of negative outcomes, and the expected postoperative course.8
Understanding the patient’s support system is critical in evaluation for elective surgery. Some geriatric patients have an extensive support network, whereas others live alone and have little help available. Depending on the postoperative needs of a particular patient, care may be required from family, friends, or home health workers. Geriatric patients undergoing head and neck reconstruction are more likely to be discharged to a nursing or other care facility when compared with younger patients. In a study of 450 patients undergoing head and neck reconstruction, 14.1% were unable to return home after surgery. Patients age 71 or older were 5 times less likely to return home than their younger counterparts; those 81 or older were 13 times less likely.9 An early analysis of psychosocial support can help with determining the long-term success of surgery and recovery. This is an especially valuable conversation for geriatric patients and those with significant comorbidities.9
Every adult is assumed to be responsible for his or her own medical decision making, and most geriatric patients maintain the capacity to consent to a procedure. In obtaining consent from a geriatric patient for surgery, a physician must ensure that (1) the patient is capable of giving consent and (2) there are no barriers to consent that cannot be easily overcome or reversed. Physicians must aim to preserve a patient’s autonomy while also being mindful that geriatric patients are more likely to have impaired cognition or physical ailments such as hearing or vision loss that can affect communication. Geriatric patients may also be physically, financially, or socially dependent on the people around them, complicating the consent process.10 If it is not clear that a patient has the level of understanding necessary to consent, a simple test such as a Mini-Mental State Examination (MMSE) can be performed to assess cognition, but a poor performance does not necessarily mean that a patient lacks capacity to consent to a surgical procedure.11 Whenever possible, patients should participate in their informed consent process.
If a patient has a designated health care proxy, the informed consent process changes. Surrogate decision makers may act in the best interest of the patient if the patient is unable to consent. Caution should be used in these situations to ensure that the surrogate decision maker is acting in accordance with both the patient’s wishes and his or her best interest. If a patient obviously lacks capacity and is in need of emergent surgery, medical care may be provided in the absence of consent if it is in the patient’s best interest and the patient’s wishes are not known. However, emergent situations do not override existing health care directives.
Shuman and colleagues promote an honest discussion of realistic surgical outcomes before head and neck cancer treatment or surgery. Given that medical or surgical stresses may lead to a change in functional status and a loss of decision-making capacity, they suggest that patients help identify surrogate decision makers in this preoperative period. Additionally, patients should outline their preferences in regard to life-sustaining interventions such as mechanical ventilation and airway management, code status, and artificial hydration and nutrition.7 It is best if these decisions are documented in the form of a living will, durable power of attorney, or formal establishment of a health care surrogate.
By understanding the patient’s treatment goals and psychosocial support, the physician can provide the best patient-centric care. Once these myriad considerations are adequately addressed in the geriatric patient, it is appropriate to proceed into the preoperative assessment, a more quantitatively driven process for evaluating a patient’s appropriateness for undergoing surgery.
 Normal Physiological Changes and Complicating Medical Comorbidities
Normal Physiological Changes and Complicating Medical Comorbidities
Certain metabolic changes predictably impact the physiological reserve of the older adult, leading to normal alterations in every organ system.12 This should not be confused with medical comorbidities that are frequently seen in older adults. These comorbidities can be just as, if not more, important in preoperative assessment than chronological age. Both normal physiological changes as well as comorbid conditions will be factors in preoperative assessment.
According to Centers for Disease Control and Prevention (CDC) data, two out of every three older Americans suffer from multiple chronic conditions.1 Every patient who is considering elective surgery must be assessed for overall health. These concurrent chronic conditions include arthritis, asthma, chronic respiratory disease, heart disease, and high blood pressure. It is now uncommon to have just one chronic condition; for example, only 9.3% of adults with diabetes have no other chronic health conditions.1 Those with ongoing medical problems are also more likely to suffer from mental illness and cognitive impairments.
Medication Assessment and Polypharmacy
In preparation for surgery the medications that a patient takes need to be elucidated and perhaps adapted. Prescription polypharmacy (using five or more prescription medications concurrently) has increased to 12% in the past few years. Geriatric patients are especially affected: of those 65 and older, 90% use at least 1 drug per week, 40% use 5 or more medications, and nearly 20% use 10 or more medications per week.12–14 The most common medications are those used for treatment of cardiovascular disease (60%), arthritis (51%), diabetes (20%), chronic obstructive pulmonary disease (COPD) (11%), and asthma (10%). Some of these medications, including aspirin, diuretics, statins, β-blockers, angiotensin-converting enzyme (ACE) inhibitors, and warfarin, are of particular concern due to effects on heart rate, blood pressure, and clot formation.14
Functional Status
In the normal aging process, metabolic function is well preserved under basal conditions.15 Functional reserve is a measurement of tolerance of an increased physiological burden and gradually decreases with age, though it varies based on genetics, lifestyle choices, and the presence of comorbidities.15 Undergoing a surgical procedure can stress and potentially exceed existing homeostasis, leading to a functional decline. Functional status is often measured by activities of daily living (ADLs) and instrumental activities of daily living (IADLs). ADLs represent the tasks necessary for self-care, whereas IADLs are the activities fundamental to living independently.16
Nutrition and Frailty
Nutritional status may worsen with age. Though this is not a normal part of aging, it is relatively common. Several factors in the geriatric population may contribute to poor nutritional status. These include inadequate dietary intake due to dementia, dysphagia, and even decreased access to or desire for food. Some medications may also affect appetite.8 Frailty has been described by Fried et al as a clinical syndrome in which three or more of the following criteria are present: unintentional weight loss (10 lb in the past year), weakness, slow walking speed, low physical activity, and self-reported exhaustion,. Frailty is increasingly prevalent with age, with 6.9% of adults aged 65 and older meeting frailty criteria. It is distinct from comorbidity and disability but is independently predictive of fall risk, hospitalization, and mortality.17
Cognitive Changes
As we age, normal cognitive changes include minor memory loss but can be complicated by dementia or delirium. There is some debate over whether surgical procedures can unmask or precipitate dementia, though its presence at baseline is known to predict poor outcomes.18 Robinson et al examined the impact of impaired cognition (evaluated via Mini-Cog testing) on postoperative outcomes in geriatric patients undergoing major elective surgeries and found complications to be more prevalent in those with a history of impaired cognition.18 Delirium is distinct from dementia, defined as a waxing and waning level of consciousness often accompanied by confusion, agitation, and disorganized thought processes. It may occur in patients with or without dementia.
Pulmonary Changes
As we age, pulmonary reserve decreases. This is characterized by a decrease in pulmonary perfusion and elastic recoil, as well as parameters such as forced expiratory volume and forced vital capacity.19 Asthma and COPD are two relatively common medical conditions that further impact lung function.
Cardiovascular Changes
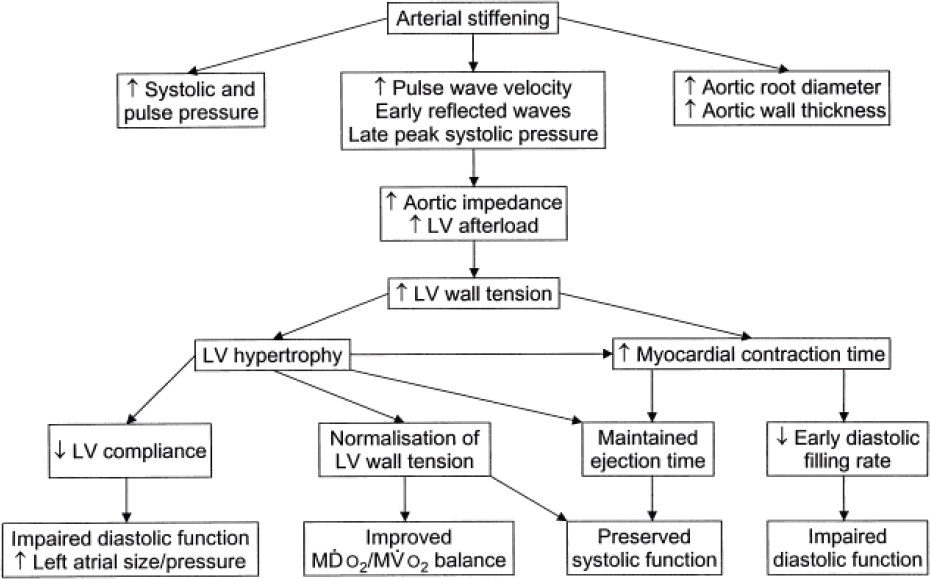
Aging is associated with numerous molecular and physiological changes in the heart muscle that affect energy usage, excitation–contraction coupling, and cell maintenance (Tables 5.1 and 5.2).20 These underlying biochemical changes in turn lead to changes in cardiac function, eventually leading to decreased contractility and stiffening of myocytes and vascular structures. Systolic blood pressure increases in response to this arterial impedance, which drives left ventricular afterload and leads to left ventricular hypertrophy (Fig. 5.1).20
Renal Changes
Glomerular filtration rate (GFR), the best measurement of renal function, slowly decreases with age. A true measurement of GFR is complicated and expensive, thus measurements of creatinine clearance (CrCl) are used. Baseline serum creatinine may slowly increase with age, but used in isolation it is not a reliable marker for renal function.21 In the middle-aged population, an increase in serum creatinine may demonstrate renal impairment, but in the geriatric population serum creatinine may return to normal because of an age-dependent decrease in muscle mass leading to a decrease in creatinine production. Patients diagnosed with diabetes or hypertension or those who have recently undergone imaging with contrast dye are more likely to demonstrate renal insufficiency.
Table 5.1 Age-related changes in cardiac morphology and function
Morphology | Decrease in myocyte number, increase in myocyte size, decrease in matrix connective tissue, increase in left ventricular wall thickness, decrease in conduction fiber density, decrease in sinus node cell number |
Function | Decrease in intrinsic contractility, increase in myocardial contraction time, decrease in myocardial contraction velocity, increase in myocardial stiffness, increase in ventricular filling pressures, increase in left atrial pressure/size, increase in action potential time, decrease in coronary flow reserve, decrease in β-adrenoceptor-mediated modulation of inotropy and chronotropy |
Used with permission from Priebe HJ. The aged cardiovascular risk patient. Br J Anaesth 2000;85(5):763–778. | |
Table 5.2 Age-related changes in vascular morphology and function
Morphology | Increase in diameter and stiffness of large elastic arteries, increase in medial and intimal thickness, increase in endothelial variant cells, increase in elastolytic and collagenolytic activity, change in vascular cell proliferation/migration, change in vascular wall matrix |
Function | Decrease in β-adrenoceptor; flowdependent, endothelium-dependent, and atrial natriuretic-peptide-mediated vasodilation; decrease in nitric oxide production/effect; increase in vascular impedance; increase in pulse wave velocity; early reflected pulse waves |
Used with permission from Priebe HJ. The aged cardiovascular risk patient. Br J Anaesth 2000;85(5):763–778. | |
Fig. 5.1 Cardiac adjustments to arterial stiffening during aging. LV, left ventricular; MDO2, myocardial oxygen delivery. MVO2, myocardial oxygen demand. (Used with permission from Priebe HJ. The aged cardiovascular risk patient. Br J Anaesth 2000;85(5):763–778.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree