Drawing 1
Flexible nasopharyngolaryngoscopy
The flexible nasopharyngolaryngoscopic exam should not be considered an alternate or equal exam to direct laryngobronchoscopy as the entire airway cannot be examined thoroughly with this modality alone at the bedside. Many noisy breathers, such as those with mild laryngomalacia, can be assessed and followed in the office with flexible nasopharyngolaryngoscopy, although some clinicians advocate that all noisy breathers (even those with mild laryngomalacia), should undergo full endoscopy in the operating room to avoid missing a concomitant secondary airway lesion. This is reported to occur in up to 19–27 % of all patients with laryngomalacia and is even higher in children who need a supraglottoplasty [9]. Due to the fact that the subglottis and lower airway cannot fully be appreciated during a flexible exam a full operating room exam should be planned if the findings on flexible endoscopy do not completely explain the child’s airway symptoms. Gonzalez demonstrated that up to 18 % of children who underwent diagnostic laryngo-bronchoscopy for airway obstruction with or without stridor had two or more synchronous airway lesions [10]. Flexible nasopharyngolaryngoscopy is a useful and invaluable starting point in the evaluation of neonatal obstruction or stridor but may require supplementation with operative endoscopy or further imaging.
Documentation
Photo and video documentation are becoming essential in following and tracking progress over the rapid period of growth that occurs during early infancy. Video can help eliminate repetitive scope examinations and the risk of traumatizing the airway (or the child) from repeat scope exams. In an academic teaching environment, it also provides a tool to provide instruction and information for family, students, trainees, and colleagues. With the advent of smartphones that can capture video, these exams can be easily recorded and shared but HIPAA regulations need to be adhered to. Still pictures are also useful but can fail to provide the dynamic structure and function of the laryngeal apparatus that video provides. Photo and video documentation is also useful for preoperative planning and guidance to determine if imaging is necessary and what modality to obtain.
Operating Room
Preparation is essential to a successful endoscopy. Endoscopy can be used for diagnostic purposes if the etiology and diagnosis are unclear. It can also be therapeutic when combined with operating or rigid microlaryngoscopy. It is important to have a plan for securing and protecting the airway before an emergency can arise. Having open communication and an agreed upon plan with the anesthesia team and operating room support staff is crucial. Each physician should have a clear role in the care so that confusion is avoided. Having the necessary supplies, including laryngoscopes, ventilating bronchoscopes, operating microscope, a selection of Hopkins rod telescopes, and appropriate size and lengths of suction catheters, as well as a tracheostomy tray should be available in the room. If the team is prepared for airway complications and the appropriate equipment is available adverse events can largely be prevented. Approaching the airway in the same systematic manner every time will help operating room staff and anesthesia staff become familiar with the routine and it will help to provide a thorough examination of the oral cavity, oral pharynx, supraglottis, glottis, subglottis, trachea, as well as all subsites. Photo documentation should be performed at multiple levels along the upper airway. Real-time video is helpful for anesthesia and OR staff to follow the progress of the procedure as well as for teaching residents/students/fellows.
Rigid Endoscopy–Direct Laryngoscopy and Rigid Bronchoscopy
Indications
There are numerous reasons to perform airway endoscopy. These include urgent and routine diagnostic or therapeutic interventions or simply to follow a child’s chronic airway conditions through planned, periodic airway examinations. A relatively urgent reason for rigid endoscopy is in the work-up of the neonate with stridor. Stridor is often a sign of a very narrow and tenuous airway. The otolaryngologist should be prepared to discuss the operative plan with the anesthesiologist before any airway manipulation occurs. Once the airway has been examined the otolaryngologist can intubate the patient if there is a need. Rigid bronchoscopy with a ventilating port can be used to examine the lower airway if a culture, biopsy, or bronchoalveolar lavage is to be performed. Rigid bronchoscopy also may provide therapeutic relief if an airway obstruction is identified or if the airway is tenuous and a more secure means of ventilation is necessary. Otherwise, the entire diagnostic exam can be performed with just a telescope.
Another indication for endoscopy is the neonate who is not improving on current therapy, whether that is increasing ventilator pressures or collapse of lung segments due to mucous plugging. Early intervention and airway examination can help to solidify a diagnosis and to establish a treatment plan going forward. If bacterial or infectious etiology is suspected, cultures can be obtained to help direct therapy. If a mucous plug is suspected, a therapeutic suctioning can be performed at the time of endoscopy. Other common reasons for endoscopic airway evaluation are to diagnose abnormalities uncovered on imaging or suspected due to other diagnostic testing.
Maintenance and routine airway endoscopy are indicated in patients with chronic conditions such as chronic indwelling tracheostomy tubes placed to bypass glottic, or subglottic stenosis, for ventilator support or for pulmonary toilet. Tracheostomy-dependent children need regular evaluation as they are at risk for developing suction-induced granulation tissue that can cause distal obstruction and supra-stomal granulomas. In the growing child, with a tracheostomy, the need for periodic upsizing can best be assessed at the time of endoscopy.
Tools for Rigid Endoscopy
Laryngoscopes
There are several varieties of laryngoscopes, all of which have varying functions and relative indications. In general there are three broad types of laryngoscope: standard laryngoscopes for general examination and intubation; subglottiscopes and anterior commissure scopes for improved view and access to the subglottis and anterior commissure; and suspension microlaryngoscopes which have a wide opening and distal lumen which are ideal for binocular microscopic procedures utilizing microdebriders, lasers, or other microlaryngoscopy instruments (Pictures 1 and 2).



Picture 1
Side view of three common laryngoscopes with light source attachment

Picture 2
View through a Dedo laryngoscope, anterior commissure laryngoscope, and a Lindholm microlaryngoscope
In choosing the best laryngoscope for direct laryngoscopy, the endoscopist will want to consider the size and age of the child and the potential need for performing a therapeutic intervention. The simplest variety of laryngoscope is that routinely used by anesthesia providers for intubation with a Miller or Mac blade. These are all readily available in most operating rooms and crash carts and come in a variety of sizes. They do suffer, unfortunately, from having less than ideal illumination. A common operating laryngoscope for direct evaluation of the newborn larynx in the operating room is the set of Karl Storz laryngoscopes designed for neonatal and pediatric patients, colloquially referred to as the Parsons laryngoscope [11]. Parsons laryngoscopes have a flat superior blade to accommodate a wide and mobile pediatric tongue. They are equipped with a left side adaptor to connect to anesthesia’s oxygen supply or inhalational anesthetic. This will help to decrease the incidence of desaturation that can accompany direct laryngoscopy in babies with poor pulmonary reserve. The Parsons laryngoscope is illuminated with a proximal xenon light cable that offers superior visualization over that afforded by a standard anesthesia-intubating laryngoscope with its distal fluorescent bulb. The Parsons set come with a wide proximal opening and an open side channel that easily allows the passage of a Hopkins rod telescope for photo documentation or other instrumentation. This side channel also allows for passage of a rigid ventilating bronchoscope or optical cup forceps. The Parsons has the added benefit of being able to be suspended from a rigid arm off of a side table Mayo tray. This allows the surgeon to have both hands free to operate or to bring in an operating microscope for further intervention. Parsons laryngoscopes come in three common sizes for premature infants, neonates/infants, and toddlers (Picture 3). Older children and adolescents can be exposed with the Benjamin laryngoscope, though it lacks the ventilation port that is present on the Parsons. A better option for suspension laryngoscopy needed in longer or more complex cases in children is the Lindholm microlaryngoscope. This laryngoscope offers a wide operating window to facilitate operative microscopy for interventions such as laser or microdebrider resection of airway lesions.


Picture 3
Parsons laryngoscopes three most common sizes from left to right size 8, 9, and 11.5
Using a laryngoscope requires a good understanding of the anatomy of the oral cavity, oropharynx, supraglottis, and glottis. Every time a laryngoscopy is performed the opportunity should be taken to perform a thorough examination as it is often difficult to perform a complete exam on newborns and infants at the bedside. When setting up for the laryngoscopy, it is important to protect the child’s eyes, head, and alveolar mucosa. These areas are at risk for iatrogenic injury if care is not taken.
Regardless of what type of laryngoscope you are using the same basic principles apply to the approach. If the patient will tolerate it, the entire procedure can be done through intermittent periods of apnea by rotating between mask ventilation and endoscopy. This generally is preferred if the procedure is relatively short and is referred to as TIVA or total intravenous anesthesia typically with Propofol as the intravenous agent and supplemental oxygen or sevoflurane delivered by way of the ventilation port of the laryngoscope. If a longer procedure is anticipated, then the patient can be intermittently intubated between examinations and therapeutic interventions. The maxilla and mandible can be retracted with a “scissor technique” to maximally open the mouth. The laryngoscope enters the oral cavity with the blade portion oriented toward the lateral portion of the oral cavity (inferior pole of the tonsil) and then gently used to retract the tongue laterally out of the field of view (Drawing 2). Suctioning should be done gently once the glottis is exposed. If the patient is intubated at the time of the initial examination, care should be taken to not dislodge the tube. For right-handed surgeons, the tube should be taped to the patient’s left oral cavity. The laryngoscope should be advanced along the base of tongue and into the vallecula and then gentle pressure on the lingual-epiglottic ligament is applied to elevate the epiglottis and expose the supraglottis and glottis. An omega-shaped epiglottis or particularly coiled epiglottis, such as those in laryngomalacia and often in premature infants, can be more difficult to elevate. Care should be taken to avoid having the epiglottis fold on itself and cause restricted blood flow to the epiglottis during the exam of the glottis as this can obstruct the glottis as well as being a source for postoperative edema and airway obstruction. Due to the nature of the examination, there is always some degree of edema from the examination that should be expected. Intravenous dexamethasone (0.4–1.0 mg/kg) can be administered to help decrease postoperative airway edema. If another laryngoscope such as a Holinger anterior commissure scope is selected, then you will place the tip of the laryngoscope under the epiglottis to completely remove it from the view of the laryngoscope. Care should be taken to avoid trauma to the anterior commissure of the vocal cords as this can result in scarring and anterior webbing. Once the vocal cords are in view, a weight-based dose of topical Lidocaine can be sprayed onto the vocal cords to allow for topical anesthesia. This helps to reduce the propensity that neonates have for laryngospasm due to stimulation of the glottis and distal airway.
Drawing 2
Proper placement of a Parsons laryngoscope for a right-handed surgeon
Once the airway is exposed, an age-appropriate sized 0° Hopkins rod telescope can be introduced through the lumen of the laryngoscope and photo documentation can be performed. If the airway is tenuous, a ventilating bronchoscope can be introduced instead of the telescope to secure the airway and allow ventilation during the examination.
A new generation of video-assisted laryngoscopes is becoming more commonly used in the operating room by pediatric anesthesiologists. Video-guided laryngoscopy has become the tool of choice for intubating children with a difficult airway. One study done in adults showed that patients with risk factors for difficult intubation were more likely to be intubated on the first attempt with a video laryngoscope than with conventional direct laryngoscopy [12]. The three most common video laryngoscopes on the market include the C-MAC®, GlideScope, and Bullard video laryngoscopes. The CMAC (Karl Storz, Tuttlingen, Germany) has a laryngoscope blade similar to the Macintosh laryngoscope blade, and can have either a separate video monitor or a video viewer in the handle. The GlideScope® Video Laryngoscope (Verathon, Bothell, Washington, USA) has only one pediatric size and has a separate video monitor screen. The Bullard scope also has only one pediatric size but its handle is specially designed to expose the larynx in children with micrognathia. Video laryngoscopy is frequently being turned to if a difficult intubation is suspected; however, one study showed that although the view of the airway was improved, there was a significantly longer time period between paralytic administration and intubation when using a video laryngoscope [13]. Video laryngoscopy is becoming more commonplace in the operating room and is particularly helpful in teaching institutions where anesthesia providers (residents, fellows, CRNAs, and EMTs) are building their skills in training programs.
Bronchoscopes
With the development of ventilating bronchoscopes able to accommodate Hopkins rod telescopes for improved optics, the use of bronchoscopy for neonates has become a safer and practical procedure (Picture 4).
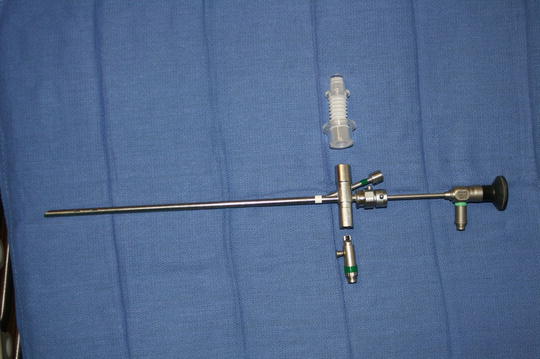
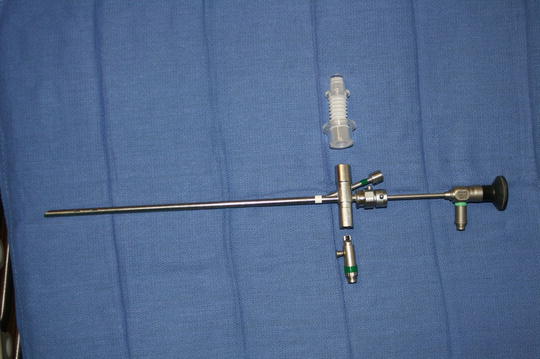
Picture 4
Partially dissembled ventilating bronchoscope
Bronchoscopy has the ability to simultaneously examine, treat, and ventilate the patient. In combination with an optical telescope, it provides excellent views of the glottis, subglottis, tracheal rings, and bronchi. Through the instrument side port, biopsies, cultures, and assays can be performed. There have been several bronchoscope-specific optical instruments developed that allow one to continue with the telescopic view and ventilate the patient while grasping a foreign body or taking a biopsy. Optical cup forceps are used for biopsy or removal of lesions such as papillomas. Optical alligator or peanut forceps are commonly used for foreign body removal. Other useful tools that can be advanced through the instrument port of a bronchoscope include several types of lasers (CO2, KTP, ND:Yag) that can feed a laser fiber through the instrument port and under direct visualization shrink or resect lesions. One example is the Omniguide® laser fiber system, a CO2 laser that can be guided directly to lesions such as papilloma, scar tissue, granulation tissue, and other lesions of the trachea or airway. Another example is the Erbe coagulation catheter which is a plasma laser used for resecting and coagulating vascular lesions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


