44

Ocular Parasitic Disease
Rafael Cortez  Gema Ramirez
Gema Ramirez  Lucienne Collet
Lucienne Collet
In 1950, Wilder reported the first cases of larval forms of nematodal intestinal roundworms causing intraocular disease (1). This chapter focuses on two disorders associated with parasitic infections: ocular toxocariasis and diffuse unilateral subacute neuroretinitis (DUSN).
OCULAR TOXOCARIASIS
Human infection by toxocara, the common roundworms of dogs and cats, can take one of two forms: visceral larva migrans (VLM) (2) and ocular toxocariasis (OT) (1, 3). The form of the infection depends on the amount of parasites, site of infection, migratory behavior, and the host immunological response (4, 5).
VLM is a generalized systemic involvement due to migration of T. canis second stage larvae. The patient with VLM is typically a child 6 months to 5 years of age, generally the course of the disease is subclinical, but it can be characterized by self-limited fever, malaise, irritability, pallor, anorexia, hepatomegaly, pulmonary signs, and marked eosinophilia (6–9).
OT appears in patients older than those with VLM, with an average age of 7.5 to 8.6 years and rarely have a history of pica (4, 5). Toxocara and other VLM were found to be the cause of intraocular inflammation in 9.4% of all pediatric uveitis cases (10, 11). Rarely, a patient presents with VLM and OT at the same time or at later times (4).
Epidemiology and Life Cycle of Toxocara Canis
The adult dog usually acquires T. canis infection by eating eggs or second stage larva found in contaminated soil or infected meat or feces. The larva encysts, and if the animal becomes pregnant some of the larvae may reactivate, at that time they can infect the fetal puppies in the uterus. Following birth the larvae migrate to the puppy’s lungs, then pass through the bronchioles to the trachea and pharynx where they are swallowed, and finally grow to become egg-producing adult worms in the gastrointestinal tract. The eggs begin to be excreted about four weeks after birth (12). Toxocara eggs are found in soil throughout tropical and temperate climates. In the United States and Western Europe samples taken from parks and other public places have yielded 10% to 30% contamination rate (13).
Humans are infected primarily from ingestion of soil (pica) contaminated with T. canis larvae or ingestion of contaminated foods (14). Humans are not natural hosts of toxocara.
After humans ingest eggs from the parasite, they develop into second stage larvae in small intestine, enter the portal circulation, hematogenous and lymphatic routes and encyst in tissues (15). Afterwards the parasites reach the eye through the retinal, ciliary and choroidal circulation.
Clinical Presentation
Patients with OT present with unilateral decreased vision, strabismus or leukocoria. The disease is typically unilateral, cases with bilateral involvement are extremely rare (16). Youngest children do not report visual changes, even if visual acuity is deeply affected, parents may seek attention only when signs become striking. Consequently, diminished visual acuity is frequently detected on routine examination (17–19).
Several ocular presentations have been recognized. Probably the most common presentation is a granuloma either on posterior pole or periphery (14, 17, 18). In some cases the child may develop overt signs of ocular inflammation. In others inflammation may have resolved (19). Some patients may present with a more marked chronic inflammation in the retina and vitreous known as nematode endophthalmitis.
Posterior Pole Granuloma
In the acute stage, retinochoroiditis appears clinically as a hazy, ill defined white lesion with overlaying inflammatory cells in the vitreous. As the acute inflammatory reaction subsides the lesion appears as a well-defined elevated mass ranging from one-half to four disc diameters in size (19, 20). In some cases traction bands may extend from the lesion to the optic disc or macular area. In chronic granuloma large retinal vessels may enter the mass and disappear into its substance, probably representing retinochoroidal anastomosis (21) (Fig. 44-1).
Peripheral Granuloma
OT can occur as an acute inflammatory process in the peripheral retina and ciliary body region (22). It may be preceded by a mild acute inflammation in anterior or posterior segment, or the eye may be quiet. The peripheral granuloma appears as a hazy, white, elevated reaction in the peripheral fundus, associated with retinal folds from the peripheral mass to the optic nerve head or to other areas of the fundus. In some cases the traction may lead to macular ectopia and severe vision loss (Fig. 44-2A and B). Wilkinson and Welch described peripheral involvement in 44% of eyes with OT (17). It is likely that many cases of “congenital” retinal folds are acquired in peripheral T. canis retinal granulomas (21).

Figure 44-1. Posterior pole toxocara granuloma. Note a traction band extending from the lesion to the optic disc, and retinochoroidal anastomosis.
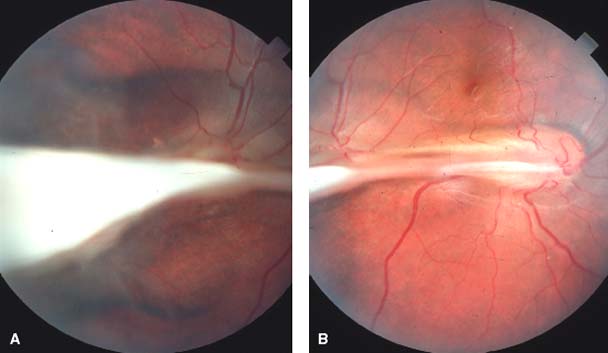
Figure 44-2. A and B: Toxocara peripheral granuloma with retinal fold extending to the optic nerve and macular ectopia.
Chronic Endophthalmitis
These cases are usually associated with a cyclitic membrane, retinal detachment, low grade anterior uveitis, posterior synechiae (Fig. 44-3). The cyclitic membrane begins in the quadrant of the most intense peripheral fundus inflammation and progresses across the posterior surface of the lens (21) (Fig. 44-4). Severe vitreitis may manifest as leukocoria (1). The clinician may observe through the hazy vitreous a yellow white mass, usually in the peripheral retina, which may resemble an endophytic retinoblastoma (21). Toxocara endophthalmitis does not produce much pain or photophobia and external ocular examination reveals only minimal signs of inflammation, usually with no ciliary flush (21) though hypopyon may develop in severe cases (23). The cicatricial stage is characterized by tractional bands that may pull retina and ciliary body. Patients with endophthalmitis are usually younger than patients with posterior pole granuloma.
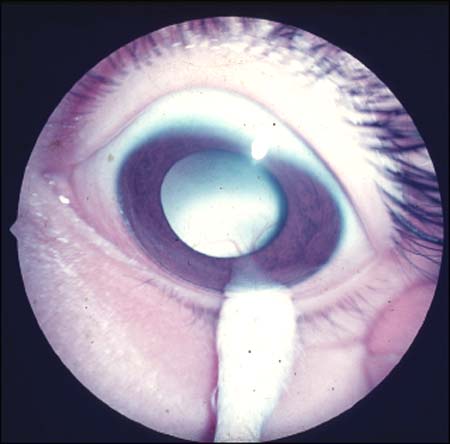
Figure 44-3. Cicatricial peripheral inflammatory mass and cyclitic membrane in a child with ocular toxocariasis.
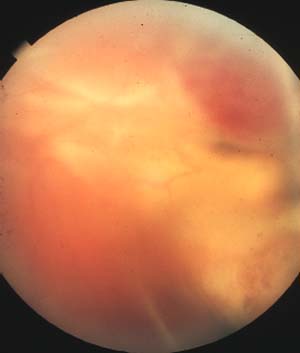
Figure 44-4. Toxocara chronic endophthalmitis with partial retinal detachment.
Atypical Presentation
OT atypical presentations may include: optic nerve granuloma (24), papillitis (25), inflammatory iris mass, intracorneal larvae (26–33), motile larvae in the vitreous and retina (25), and scleritis (18). We evaluated two cases with vitreous hemorrhage; and after the hemorrhage cleared, typical fundus changes of a posterior pole granuloma were detected.
Differential Diagnosis
Toxocara endophthalmitis may closely resemble an endophytic retinoblastoma (RB). Shields et al. found that 42% of patients with presumed RB had pseudoretinoblastoma, and among them 16% had OT (26). There are several clinical features that may help differentiate both entities. The mean age at presentation for RB is 22 to 23 months, while for OT is 7.5 to 8.9 years (4, 5). RB show tumor growth. Finally, RB does not cause inflammation.
In OT cases there is vitreoretinal traction and signs of inflammation, and a posterior subcapsular cataract, which is unusual in patients with RB. In cases in which the differential diagnosis is relatively difficult, ultrasonography and computed tomography are valuable in demonstrating intraocular tumor and calcium (17).
Additionally, OT may present with eosinophils in the vitreous or aqueous humor without evidence of malignant cells and normal levels of dehydrogenase lactate and phosphoglucose isomerase (27). Other entities to be excluded are toxoplasmic retinochoroiditis, pars planitis, retinopathy of prematurity, familial exudative vitreoretinopathy, persistent fetal vasculature, Coat’s disease, and organized vitreous hemorrhage.
Diagnosis
The current test of choice to document systemic or ocular infection with Toxocara canis is the ELISA test (17, 21) with 90% of sensitivity and specificity. Although the Center for Disease Control and Prevention consider serum ELISA titers less than 1:32 to be insignificant in the diagnosis of systemic toxocariasis (17), others have stated that a serum titer of 1:8, or even lower is sufficient to support the diagnosis of OT if the patient has signs and symptoms compatible with that disorder (17). However a positive serum titer cannot be used to absolutely confirm the diagnosis of OT, although the absence of serologic evidence of toxocara infestation may assist in reducing the odds of this organism as being the cause of ocular disease (17). Authors have found that 31.8% of 333 children without sings of OT exhibited a serum titer ≥1:16. Elisa testing of intraocular fluids has demonstrated to be of great value in diagnosing OT (19).
Treatment
Treatment depends primarily on the stage of inflammation initially observed and the secondary structural changes in the vitreous and retina associated with this infestation (17). In most cases of severe nematode endophthalmitis, the natural course of the disease is characterized by numerous complications which frequently result in total blindness. Therefore, prompt treatment in cases of severe endophthalmitis is justified (19).
Medical Treatment
In OT the treatment objective is to reduce inflammation in order to prevent the formation of membranes that consequently can affect intraocular structures (28). Periocular and systemic steroids (0.5 to 1 mg/kg prednisone daily) are the mainstays for eyes with active vitreitis. Cycloplegic agents should be employed when signs of anterior segment involvement are present (17). In OT patients treated with antihelmintic agents, clinical improvement have been reported. Thiabendazole (25 mg/kg twice daily for 5 days with a maximum of 3 g/day), albendazole (800 mg twice daily for 6 days), or mebendazole (100 to 200 mg twice daily for 5 days) (28, 29). Although it has been suggested that antihelmintic treatment may initiate an intraocular inflammation due to a hypersensitivity response to the dead larvae (30) clinical and experimental evidence indicate that this is not the case (28, 31). The ultimate utility of antihelmintic therapy remains an open question (19, 28).
Surgical Treatment
Surgery is saved for post-inflammatory complications such as persistent vitreous opacification, retinal detachment, epiretinal membrane formation with vitreomacular or optic nerve traction, vitreous opacification. (Fig. 44-5A and B) The most common surgical indication in OT is retinal detachment (32–35). Studies have shown that the retina can be reattached in 71% to 88% of the cases, with visual improvement in most patients (34).
DIFFUSE UNILATERAL SUBACUTE NEURORETINITIS
DUSN was first described by Gass and Scelfo in 1978 (36). They reported 29 patients between the ages 5 and 22 years, with severe visual loss in one eye, vitreitis, mild papillitis, and recurrent crops of evanescent, gray-white lesions affecting the outer retina and retinal pigment epithelium (RPE). These lesions are followed by progressive loss of visual field, optic atrophy, narrowing of the major retinal vessel, diffuse as well as focal RPE depigmentation throughout the fundus, and a moderate to marked reduction of the b-wave amplitude in the multifocal electroretinogram (mfERG). Previously this condition was described as “unilateral wipe-out syndrome” (37). In a later report, 12 additional patients were described, and in two of them a motile subretinal nematode was observed (38).
DUSN is prevalent in southeastern USA and the Caribbean, although some cases have been reported in the upper midwestern USA, Canada, the Caribbean, the northern part of South America, Europe, and China (39–41). In the United States, DUSN probably is caused by at least two different nematodes. The smaller one measures between 400 and 1000 um in length, and has a diameter of approximately one twentieth of its length (39, 41). It is found in patients mainly from the southeastern US, the Caribbean, and the northern part of South America (39–41). A larger nematode, 1500 to 2000 um in length, is responsible for DUSN in patients in the northern midwestern USA, and in some patients from Brazil, however one case was reported in Brazil caused by a large nematode (41–43).
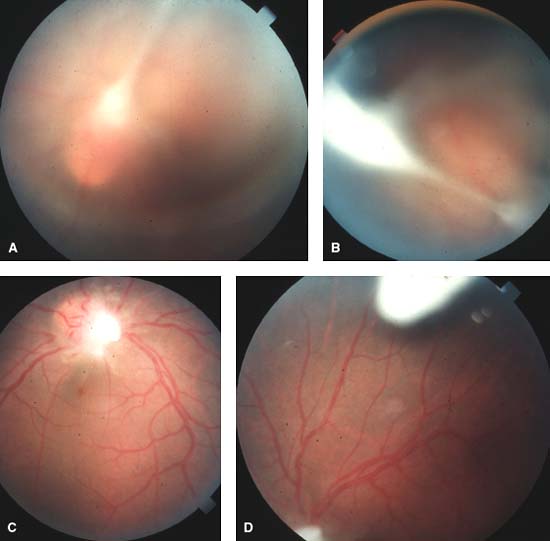
Figure 44-5. A1 and B1: Toxocara peripheral granuloma with tractional fibrotic band extending to the optic nerve. A2 and B2: Same case as A1 and B1 after pars plana vitrectomy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


