Ocular Disorders Associated with Systemic Diseases: Introduction
Examination of the eye provides invaluable information for the diagnosis and monitoring of systemic disease. Nowhere else in the body can a microcirculatory system be directly visualized, investigated with such precision or neural tissue so easily examined, and nowhere else are the results of minute focal lesions so devastating. Many systemic diseases involve the eyes, and therapy demands some knowledge of the vascular, rheologic, and immunologic nature of these diseases.
Vascular Disease
The blood supply to the eye is from the ophthalmic artery, which is the first branch of the internal carotid artery (see Chapter 1). The first branches of the ophthalmic artery are the central retinal artery and the long posterior ciliary arteries. The retina is perfused by retinal and choroidal vessels that provide contrasting anatomic and physiologic circulations. The retinal arteries correspond to arterioles in the systemic circulation. They function as end arteries and feed a capillary bed consisting of small capillaries (7 μm) with tight endothelial junctions. Dependent on this anatomic arrangement is the maintenance of the blood-retina barrier, and this system is autoregulated, there being no autonomic nerve fibers. Most of the blood within the eye, however, is in the choroidal circulation, which is characterized by a high flow rate, autonomic regulation, and an anatomic arrangement with collateral branching and large capillaries (30 μm), all of which have fenestrations in juxtaposition to Bruch’s membrane. Examination of the retinal vessels is facilitated by the use of red-free light and fluorescein angiography, whereas indocyanine green angiography gives further information about the choroidal vessels.
The sources of fundal hemorrhages may be arteries, capillaries, or veins, and their configurations depend on the site and severity of the disruption of vascular integrity (Figure 15–1). They usually indicate some abnormality of the retinal or choroidal vascular system but they may be caused by any condition that alters the efficacy of the endothelial barrier. The contribution of systemic factors should be considered in relation to (1) vessel wall disease (eg, hypertension, diabetes), (2) blood disorders (eg, thrombocytopenia, anemia, leukemia), and (3) reduced perfusion (eg, carotid artery–cavernous sinus fistula, acute blood loss).
These result from damage to superficial disk or retinal vessels, which commonly are the consequence of retinal neovascularization, and are usually large with a crescentic shape, a gravity-dependent fluid level forming the superior border, and the extent of posterior vitreous detachment determining the lower border.
These lie in the superficial nerve fiber layer and their shape, often so-called flame-shaped, reflects the orientation of the retinal ganglion cell axons in the affected area of the fundus.
These are situated deeper in the substance of the retina, their source being capillaries and smaller venules. Their circular appearance reflects the compact arrangement of the deeper retinal tissues.
Normally there are no blood vessels between the retina and the choroid, but these may arise due to optic disk abnormalities or whenever there is subretinal neovascularization. They are large and red, with a well-defined margin and no fluid level.
Hemorrhages situated under the retinal pigment epithelium are usually dark and large, their source being choroidal vessels. They need to be differentiated from choroidal melanomas and hemangiomas.
Although commonly thought to be peculiar to subacute bacterial endocarditis, superficial retinal hemorrhages with pale or white centers are not pathognomonic of any disease process. They may be due to (1) a cotton-wool spot (see later in the chapter) with surrounding hemorrhage; (2) retinal hemorrhage in combination with extravasation of white blood cells (eg, leukemia); or (3) retinal hemorrhage with central resolution.
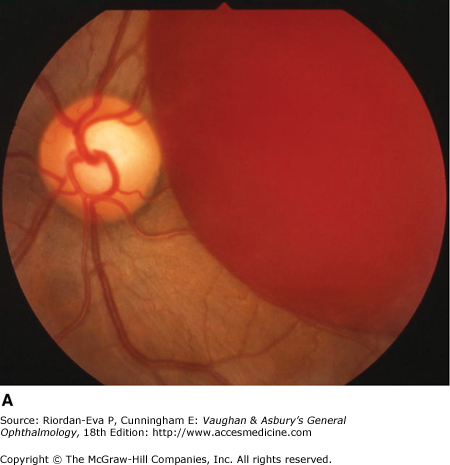
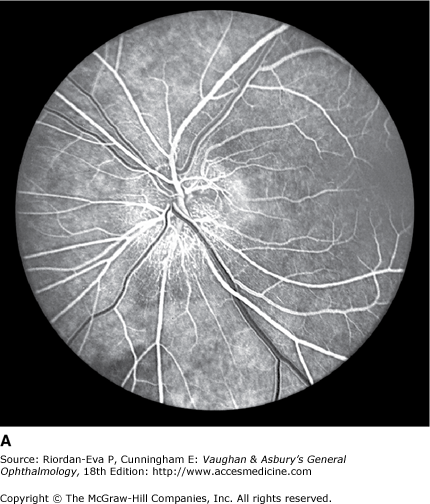
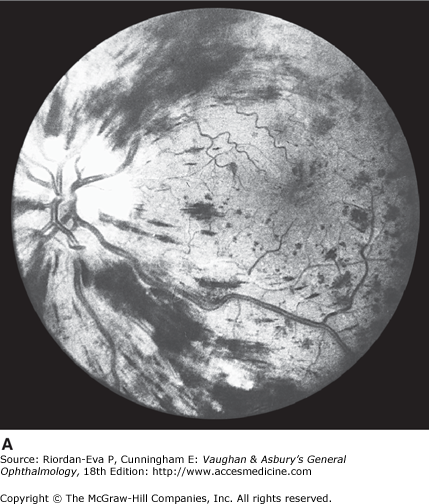
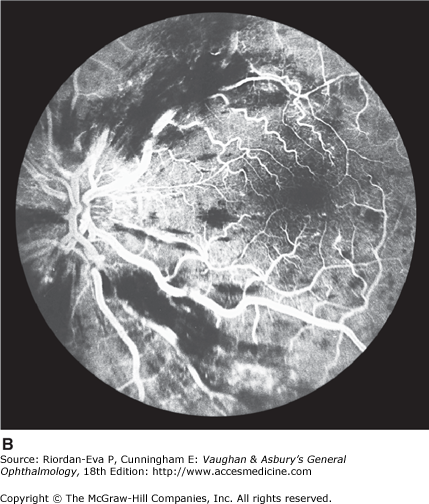
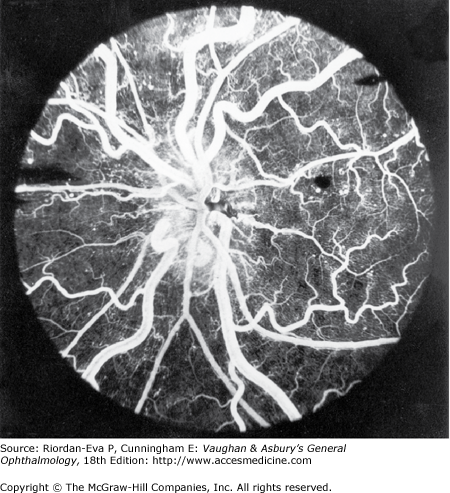
Impairment of the blood supply to the optic disk produces sudden visual loss, usually with an altitudinal field defect, and sectoral pallid swelling of the optic disk. The primary abnormality is complete or partial interruption of the choroidal blood supply to the disk, while the retinal capillaries on the surface of the disk appear dilated. Fluorescein angiography confirms the circulatory alterations (Figure 15–2). Pathologic studies show infarction of the retrolaminar region of the optic nerve. The explanation for the vulnerability of the short posterior ciliary vessels supplying this region is unclear.
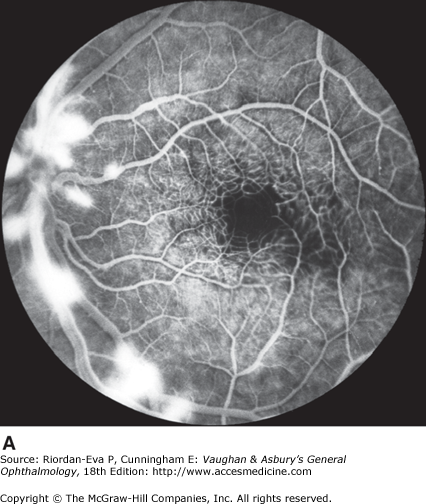
Figure 15-2.
Ischemic optic neuropathy. Sudden visual loss in a 48-year-old man produced a complete inferior altitudinal field loss. A: Fluorescein angiogram shows impaired filling of the upper part of the disk with dilation of retinal capillaries at the lower part of the disk. B: Photograph taken 10 minutes after injection shows leakage of dye mainly at the lower part of the disk.
The most common cause is non-arteritic anterior ischemic optic neuropathy (NAION), in which the optic disk is small, the so-called “disk at risk,” and hypertension and arteriosclerotic disease are the commonly identified additional factors in middle age, although it is uncertain whether vascular occlusion or a perfusion deficit is the precipitating event. With increasing likelihood with increasing age over 50 years, optic disk infarction may be caused by giant cell arteritis. Other systemic vasculitides (such as ANCA-associated vasculitis) may also present with anterior ischemic optic neuropathy. The visual loss is usually less severe than in GCA and the disc may not be small as in NAION. Bilateral optic disk infarction can be seen after sudden hypotension following acute blood loss, but posterior (retrobulbar) optic nerve infarction without optic disc changes in the acute stage is more typical.
This is extremely rare, although certain clinical appearances have been attributed to ciliary vessel occlusion. These include small pale areas in the equatorial region that resolve to leave mottled pigmentary areas (Elschnig’s spots) due to necrosis of the pigment epithelium. Larger infarcts may occur and may be triangular (Amalric’s sign) or linear (Siegrist streaks) (Figure 15–3).
The funduscopic appearance of arteriolar occlusion depends on the size of the vessel occluded, the duration of occlusion, and the time course. Occlusion of major arterioles (retinal arteries) produces total, hemispheric, or segmental pallid swelling of the retina, with corresponding visual loss (Figure 15–4) (see Chapter 10). Central retinal artery occlusion is usually due to atherosclerosis but can result from embolic disease. It can also be a manifestation of giant cell arteritis in the elderly. Branch retinal artery occlusion is more commonly due to emboli (see later in the chapter).
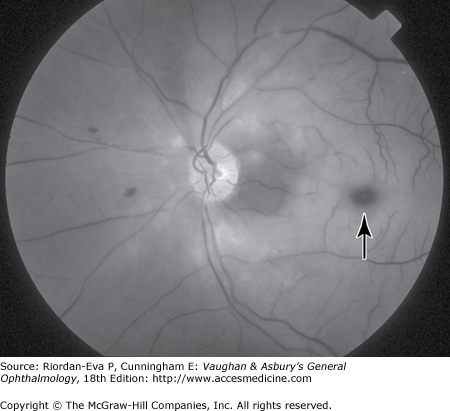
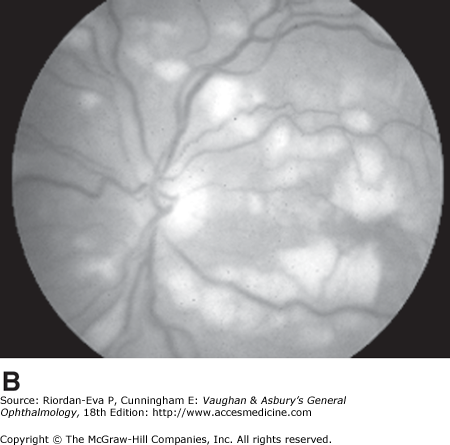
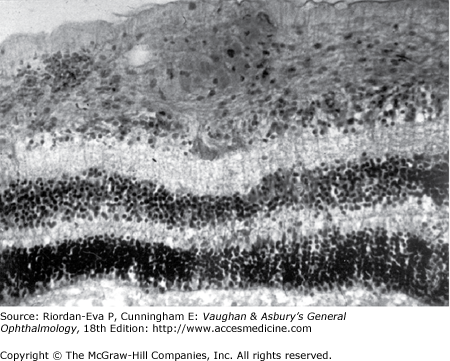
A cotton-wool spot (Figure 15–5), representing interruption of axoplasmic transport in the axons of the retinal nerve fiber layer due to superficial retinal ischemia, is usually due to occlusion of a precapillary retinal arteriole but occasionally may result from more proximal impairment of retinal blood flow. It consists of pale, slightly elevated swelling usually one-fourth to one-half the size of the optic disk. Pathologic examination shows distention of neurons, with cytoid bodies (Figure 15–6); electron microscopy shows accumulation of axoplasm and organelles.
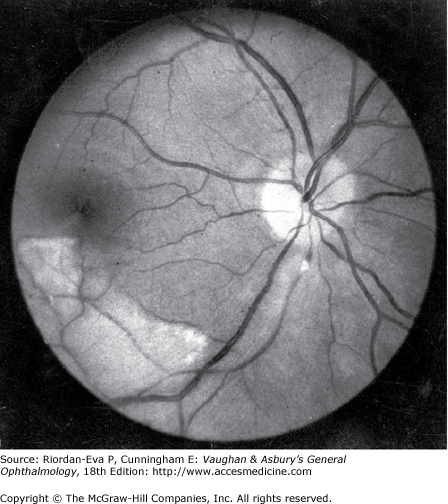
Figure 15-5.
Cotton-wool spots. Numerous cotton-wool spots are seen in the posterior poles in three patients. (A) A young woman with acute systemic lupus erythematosus and neurologic disease. (B) A young man with pancreatitis (Purtscher’s retinopathy). (C) A patient with HIV infection. Cotton-wool spots resolve over 6 weeks regardless of their cause.
Episodes of complete monocular visual loss with full recovery after 5–10 minutes, the beginning and end often being described as a curtain passing vertically across the vision, are characteristic of transient retinal ischemia due to transit of platelet-fibrin emboli through the retinal circulation (amaurosis fugax). Paresthesias or weakness in the contralateral limbs confirm involvement of the vascular territory of the internal carotid artery, with embolization into the ophthalmic and middle cerebral arteries.
Retinal emboli most commonly arise from carotid artery disease (see Chapter 14). A cardiac cause such as atrial fibrillation, mitral or aortic valve disease, or subacute infective endocarditis needs to be considered, particularly in patients under 40 years of age or those with a history of cardiac disease. It is important for the ophthalmologist to search the fundus for emboli, although frequently they are not seen; auscultate for carotid bruits and cardiac murmurs; check the pulse for atrial fibrillation; and arrange investigations for disease of the carotids, including for underlying risk factors, and cardiac disease as appropriate. Retinal emboli, whether or not associated with retinal dysfunction, indicate a risk of stroke and the incidental discovery of usually cholesterol emboli should prompt similar assessment.
The three main types of retinal emboli are:
Cholesterol emboli—These so-called Hollenhorst plaques usually arise from an atheromatous plaque in the carotid artery. They initially lodge at the bifurcation of retinal arterioles, are refractile, and may appear larger than the vessel that contains them but may not obstruct the blood flow (Figure 15–7). Passage of a cholesterol embolus may result in permanent focal arteriolar whitening.
Platelet-fibrin emboli—These are usually broken up as they traverse the retinal circulation, and hence are rarely seen, although occasionally they produce retinal infarction. Usually arising from abnormalities of the great vessels or heart, they may be reduced by drugs that reduce platelet aggregation (eg, aspirin).
Calcific emboli—Originating from damaged cardiac valves, these solid emboli usually lodge permanently within a retinal arteriole, producing complete occlusion and infarction of the distal retina.
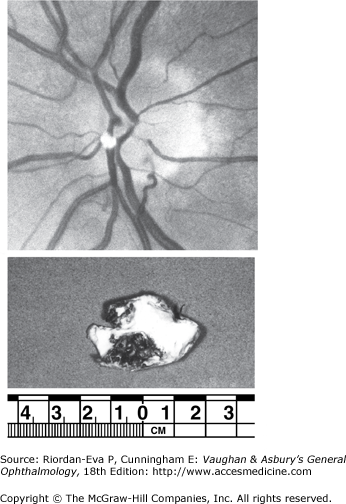
Figure 15-7.
Cholesterol embolus (Hollenhorst plaque). Top: A cholesterol embolus at the optic disk, which is refractile and appears larger than the vessel that contains it. A collateral vessel is seen at the lower border of the disk. Bottom: Surgical specimen from a patient with a similar embolus shows an atheromatous ulcer at the bifurcation of the common carotid artery.
There are several other causes of transient visual loss, including cerebral emboli, arterial occlusive disease, including giant cell arteritis, hematologic disease, systemic hypertension, systemic hypotension that may be due to various entities, migraine, raised intraocular pressure, and raised intracranial pressure (Table 15–1).
| Retinal emboli (amaurosis fugax) or cerebral emboli |
| Carotid artery stenosis, ulceration, or dissection |
| Basilar or vertebral artery disease (cerebral not retinal emboli) |
| Cardiac dysrhythmia (eg, atrial fibrillation) |
| Cardiac valvular disease (eg, mitral leaflet prolapse) |
| Left ventricular aneurysm with mural thrombus secondary to myocardial infarction |
| Arterial occlusive disease |
| Internal carotid artery occlusion |
| Basilar or vertebral artery occlusion |
| Arteritis (eg, giant cell arteritis) |
| Hematologic disease |
| Anemia |
| Polycythemia |
| Macroglobulinemia |
| Sickle cell disease |
| Other |
| Systemic hypertension |
| Systemic hypotension |
| Drugs |
| Cardiac dysrhythmia |
| Impaired left ventricular function |
| Autonomic dysfunction (eg, diabetes mellitus) |
| Endocrine dysfunction (eg, Addison’s disease) |
| Blood loss |
| Shock |
| Migraine, including retinal (choroidal) migraine |
| Raised intraocular pressure |
| Raised intracranial pressure |
Central retinal vein occlusion is an important cause of visual morbidity in elderly people, particularly those with hypertension or glaucoma.
Fundus examination shows dilated tortuous veins with retinal and macular edema, hemorrhages all over the posterior pole, and cotton-wool spots. The arterioles are usually attenuated, indicating generalized microvascular disease.
Fluorescein angiography demonstrates two types of response: a nonischemic type, with dilation of retinal vessels and edema; and an ischemic type, with large areas of capillary nonperfusion or evidence of retinal or anterior segment neovascularization. In less than 10% of ischemic but over 80% of nonischemic central retinal vein occlusions, the ultimate visual acuity is better than 20/200.
Central retinal vein occlusion has an increased incidence in certain systemic conditions such as hypertension, hyperlipidemia, diabetes mellitus, collagen-vascular diseases, chronic renal failure, and hyperviscosity syndromes (eg, myeloma, Waldenström’s macroglobulinemia). Smoking is also a risk factor. Central retinal vein occlusion is associated with increased mortality from ischemic heart disease, including myocardial infarction. Investigations include measurement of serum lipids, plasma proteins, plasma glucose, and assessment of blood viscosity by hemoglobin, hematocrit, and fibrinogen estimations. In young patients, the antiphospholipid antibody syndrome should be excluded, and protein C, protein S, factor V Leiden, homocysteine, and antithrombin III levels should be measured to exclude abnormalities of the thrombolytic system. If hypertension is present, simple renal function tests, including urea and electrolytes, estimation of creatinine clearance, microscopic examination of the urine, and renal ultrasound are indicated.
Treatment of retinal vein occlusion is unsatisfactory. Randomized controlled trials treating patients with hemodilution have reported variable results. Trials with anticoagulants and fibrinolytic agents have not been successful. Intravitreal vascular endothelial growth factor (VEGF) inhibitors or steroid may be indicated, and surgical procedures are being investigated (see Chapter 10). In ischemic central retinal vein occlusion, pan-retinal laser photocoagulation is effective in preventing and treating secondary neovascular glaucoma.
Occasionally, central retinal vein occlusion occurs in young people and may be associated with cells in the vitreous. Rheologic investigations are usually negative, and the prognosis for vision is good.
Occlusion of a branch vein should be viewed as part of the spectrum of central retinal vein occlusion. Investigations are similar in the two conditions, but arterial disease—particularly hypertension—is common. Branch retinal vein occlusion occurs more frequently in the superotemporal and inferotemporal regions and particularly at sites where arteries cross over veins, and only rarely where veins cross over arteries.
The roles of laser treatment, intravitreal anti-VEGF agents or steroid, and surgery in the management of branch retinal vein occlusion are discussed in Chapters 10 and 24.
The process of atherosclerosis occurs in larger arteries and is due to fatty infiltration of a patchy nature occurring in the intima and associated with fibrosis. Involvement of smaller vessels (ie, < 300 μm) by diffuse fibrosis and hyalinization is termed arteriosclerosis. The retinal vessels beyond the disk are less than 300 μm; therefore, involvement of the retinal arterioles should be termed arteriosclerosis, whereas involvement of the central retinal artery is properly termed atherosclerosis.
Atherosclerosis is a progressive change developing in the second decade, with lipid streaks in larger vessels, progressing to a fibrous plaque in the third decade. In the fourth and fifth decades, ulceration, hemorrhages, and thrombosis occur, and the lesion may be calcified. Destruction of the elastic and muscular elements of the media produces ectasia and rupture of the large vessels, although in smaller vessels obstruction is usually seen. The clinical results of atherosclerosis are seen several decades after the onset of the process. Factors contributing to atheroma include hyperlipidemia, hypertension, and obesity.
Arteriosclerosis is characterized by an enhanced light reflection, focal attenuation, and irregularity of caliber. These signs may also be seen in the arterioles of normotensive individuals in middle age. In elderly individuals with arteriosclerosis and associated mild hypertension, it is difficult to differentiate the changes of arteriosclerosis from those due to hypertension.
A normal arteriolar wall is transparent, so that what is actually seen is the column of blood within the vessel. A thin, central light reflection in the center of the blood column appears as a yellow refractile line about one-fifth the width of the column. As the walls of the arterioles become infiltrated with lipids and cholesterol, the vessels become sclerotic. As this process continues, the vessel wall gradually loses its transparency and becomes visible; the blood column appears wider than normal, and the thin light reflection becomes broader. The grayish yellow fat products in the vessel wall blend with the red of the blood column to produce a typical “copper wire” appearance. This indicates moderate arteriosclerosis. As sclerosis proceeds, the blood column-vessel wall light reflection resembles “silver wire,” which indicates severe arteriosclerosis; at times, even occlusion of an arteriolar branch may occur.
Red-free light (a white light with a green filter) allows details of hemorrhages, focal irregularity of blood vessels, and nerve fibers to be seen more clearly (Figure 15–10).
Figure 15-10.
Acute retinal infarction. Red-free photograph shows acute arterial occlusion in a congenitally anomalous vessel at the disk. The inferior retina is infarcted, but axoplasm has accumulated beneath the fovea in an irregular pattern owing to preserved neuronal function of the distal ganglion cells.
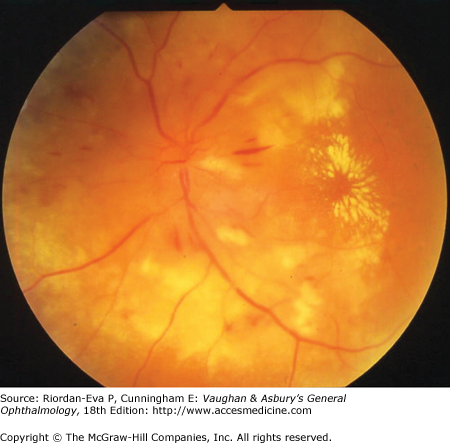
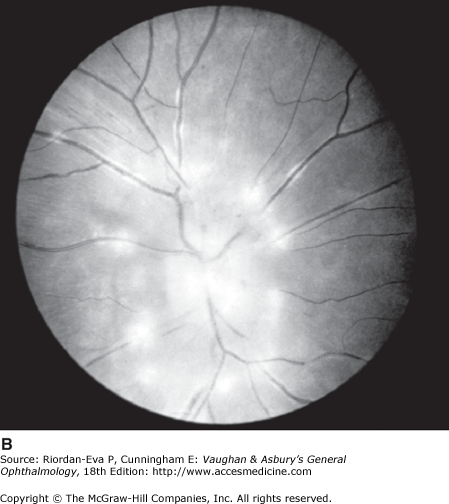
The appearance of the fundus in hypertensive retinochoroidopathy is determined by the degree of elevation of the blood pressure and the state of the retinal arterioles. In mild to moderate systemic hypertension, the retinal signs may be subtle. Focal attenuation of a major retinal arteriole is one of the earliest signs. Diffuse arteriolar attenuation, broadening of the arteriolar light reflex, and arteriovenous crossing changes also occur. However, in young patients with accelerated malignant hypertension, an extensive retinopathy is seen, with hemorrhages, retinal infarcts (cotton-wool spots), choroidal infarcts, and occasionally serous detachment of the retina. Severe disk edema is a prominent feature and may be accompanied by a macular star of hard exudates (Figure 15–11). Vision may be impaired and may deteriorate further if blood pressure is reduced too quickly.
In contrast, elderly patients with arteriosclerotic vessels are unable to respond in this manner, and their vessels are thus protected by the arteriosclerosis. It is for this reason that elderly patients seldom exhibit florid hypertensive retinochoroidopathy (Figure 15–12).
In young patients with hypertension, fluorescein angiography demonstrates arteriolar attenuation and occlusion and capillary nonperfusion in relation to a cotton-wool spot, which is surrounded by abnormal dilated capillaries and microaneurysms with increased permeability. Resolution of the cotton-wool spots and the arteriolar changes occurs with successful hypotensive therapy. In elderly patients, the underlying arterio-sclerotic changes are irreversible.
A severe retinochoroidopathy may be seen in advanced renal disease, in patients with pheochromocytoma, and in preeclampsia–eclampsia. All such patients should receive a complete medical workup to establish the nature of the hypertension.
Reduction in the retinal arteriovenous pressure gradient may produce acute signs of ocular ischemia (see preceding pages) or the less frequently recognized chronic changes.
Carotid occlusive disease usually presents in middle-aged and elderly patients and is due to involvement of both the carotid artery and its smaller branches. Contributory factors include hypertension, smoking, and hyperlipidemia.
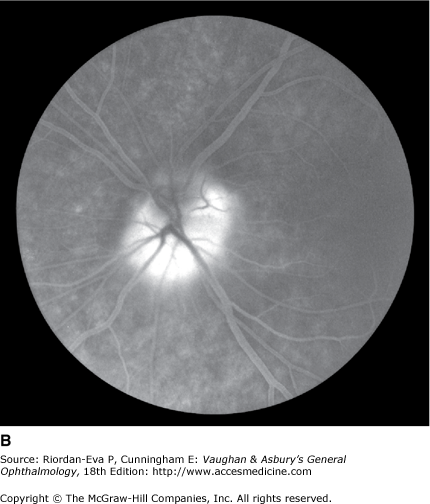
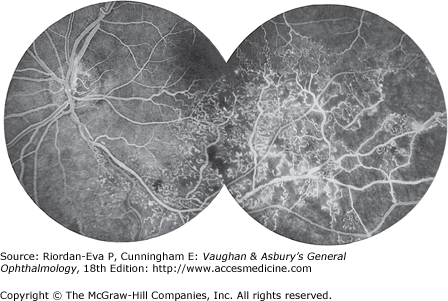
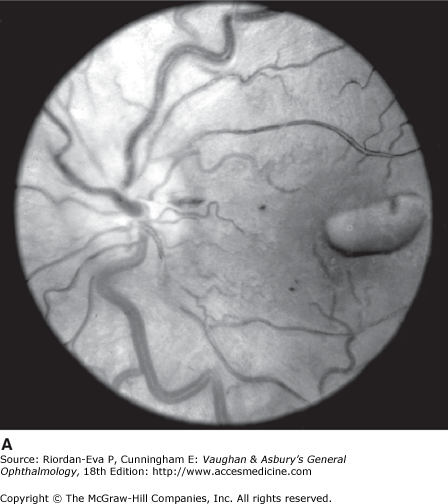
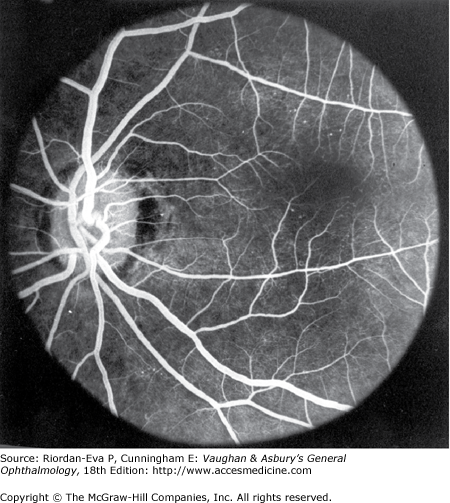
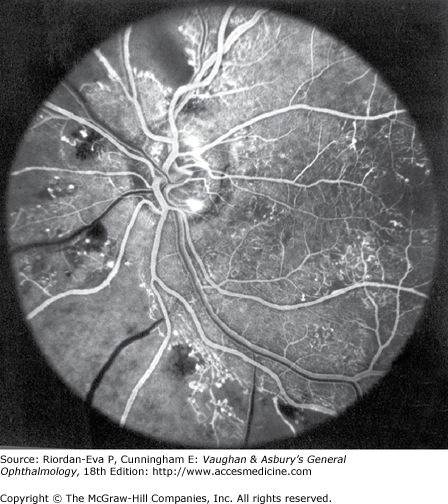
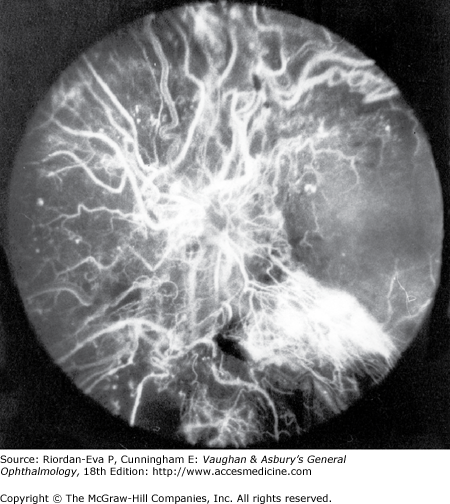
In anterior segment ischemia, patients develop iritis, intraocular pressure changes, and pupillary abnormalities. In retinal ischemia (Figure 15–13A), patients show evidence of capillary dilation and hemorrhages, capillary occlusion, new vessels at the optic disk, and cotton-wool spots.
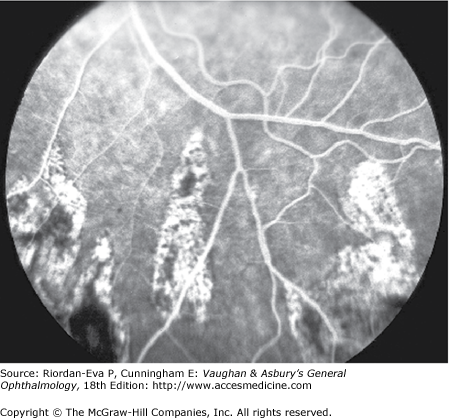
Figure 15-13.
A: Fluorescein angiogram of left fundus in a patient with chronic ocular ischemia secondary to Takayasu’s disease. Note capillary dilation, leakage of dye, retinal hemorrhages, cotton-wool spots, and neovascularization of the optic nerve head. B: Fluorescein angiogram, showing leakage at optic disk and macula in a patient with chronic ocular ischemia secondary to dural arteriovenous fistula.
Carotid artery–cavernous sinus fistula results from a communication between the carotid artery or its branches and the cavernous sinus. Direct fistulas occur as a consequence of rupture of the intracavernous internal carotid artery, due to aneurysm, weakened vessel wall (eg, collagen vascular disease and Ehler’s Danlos syndrome), or trauma. They usually have an acute, florid presentation and commonly require closure. Indirect (dural) fistulas are chronic and mild. They are associated with diabetes and systemic hypertension and may be a consequence of thrombosis of dural veins. Frequently they resolve spontaneously. Clinical features of carotid artery–cavernous sinus fistulas include dilated conjunctival and episcleral vessels, elevated intraocular pressure, dilated retinal vessels with hemorrhages and fluorescein leakage (Figure 15–13B), ophthalmoplegia (usually lateral rectus), and bruit. Computed tomography (CT) and magnetic resonance imaging (MRI) show thickened ocular muscles and a dilated superior ophthalmic vein, the latter being a differentiating feature from thyroid eye disease. Reversal of flow (“arterializations”) in the superior ophthalmic vein is a characteristic finding on orbital ultrasound blood flow studies. When required, closure of carotid artery–cavernous sinus fistulas is usually achieved by interventional radiological techniques.
Idiopathic intracranial hypertension is characterized by raised intracranial pressure with normal cerebrospinal fluid constituents and normal radiologic studies, particularly no evidence of cerebral venous sinus occlusion. The cause of the increased intracranial pressure is unknown, although diminished absorption of cerebrospinal fluid due to impaired venous sinus drainage is suspected. Usually patients are young overweight women and present with headache; transient visual obscurations, blurred vision, and diplopia are the ophthalmologic features. Etiologic factors that need to be excluded include (1) drug therapy, particularly tetracyclines, retinoids including vitamin A, prolonged steroid therapy or in children steroid withdrawal, and possibly hormonal contraceptives; (2) endocrine abnormalities; and (3) sleep apnea syndrome. Idiopathic intracranial hypertension is very rare in adult men.
Initially visual fields are normal apart from enlarged blind spots due to papilledema. Generalized field constriction and inferonasal and arcuate defects may occur. CT or MRI usually shows distended optic nerve sheaths, flattened globes, and an empty pituitary sella. The aims of treatment are to minimize permanent visual loss, which occurs in up to 50% of patients, and relieve symptoms. Treatment options include weight loss, oral acetazolamide or other diuretics, cerebrospinal fluid shunt, and optic nerve sheath fenestration (see also Chapter 14).
Inflammatory changes on the cardiac valves may produce multiple embolization with frequent ocular manifestations that range from retinal and choroidal infarction to a mild infective vitritis. The emboli may be composed of platelet-fibrin aggregates or calcified endocardial vegetations (Figure 15–14).
Hematologic & Lymphatic Disorders
The ocular changes of leukemia occur primarily in those structures with a good blood supply, including the retina, the choroid, and the optic disk (Figure 15–15). Changes are most common in the acute leukemias, where hemorrhages are seen in the nerve fiber and pre-retinal layers.
Increased viscosity results in reduced flow ocular perfusion, producing dilation of the retinal arteries and veins, hemorrhages, microaneurysms, and areas of capillary closure (Figure 15–16). The main causes are polycythemia, either primary or secondary, macroglobulinemia, and multiple myeloma. Treatment of the hyperviscosity can reverse the retinal changes.
Sickle cell hemoglobinopathies are heritable disorders in which the normal adult hemoglobin is replaced by sickle hemoglobin in the red cell. This causes “sickle-shaped” deformity of the red cell on deoxygenation.
Ocular abnormalities include conjunctival changes, with “comma-shaped capillaries,” and retinal changes, including arterial occlusions and peripheral capillary closure, which leads to new vessel formation, particularly a sea-fan pattern. Retinal detachment may develop. Laser therapy is rarely needed, since the complexes fibrose and reperfusion can occur.
Neoplastic disease may involve the eye and optic pathways by direct spread, metastases, or immunologic mechanisms.
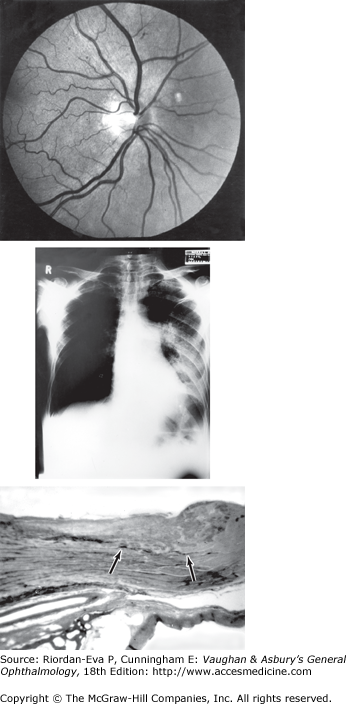
Figure 15-17.
Neoplastic disease. A: Normal fundus of a patient with rapid visual loss in his only eye. B: Chest x-ray showed left lower lobe consolidation and a hilar mass. C: Carcinoma of the bronchus was confirmed at autopsy, and metastasis was found in the optic nerve in the region of the canal (arrows).
The consequences of metastatic spread depend on the size and site of the metastatic tumor and the site of the primary lesion. The most frequent primary tumor metastasizing to the eye is carcinoma of the breast in women and bronchial carcinoma in men (see Chapters 7 and 10). Most patients have a known history of cancer, but in a third of patients presenting with ocular metastasis the primary tumor has yet to be diagnosed. Visual loss may occur from nonmetastatic disease, due to so-called cancer-associated retinopathy (CAR), melanoma-associated retinopathy (MAR), each associated with specific retinal autoantibodies and characteristic electrophysiological abnormalities, or diffuse uveal melanocytic proliferation.
Metabolic Disorders
Diabetes mellitus is a complex metabolic disorder that involves the small blood vessels, often causing widespread damage to tissues, including the eyes.
The risk of ocular complications is increased by poor diabetic control but they still occur approximately 20 years after onset despite apparently adequate control. The lengthened life span of diabetics has resulted in a marked increase in the incidence of retinopathy and other ocular complications. The visual outlook is generally better for type 2 than for type 1 diabetics.
The possibility of diabetes should be considered in all patients with unexplained retinopathy, cataract, extraocular muscle palsy, optic neuropathy, or sudden changes in refractive error. Absence of glycosuria or a normal fasting blood glucose level does not exclude a diagnosis of diabetes.
Diabetic retinopathy is a common cause of blindness. In the Western world, it accounts for almost one-fourth of blind registrations and is the commonest cause of new blindness in the population of working age.
Good control of diabetes and hypertension retards the development of retinopathy and other diabetic complications.
Type 1 diabetics develop a severe form of retinopathy within 20 years in 60%–75% of cases even if under good control. The retinopathy is usually proliferative. In the usually older type 2 diabetic patients, retinopathy is more often nonproliferative, with the risk of severe central visual loss from maculopathy.
The clinical features and treatment of diabetic retinopathy are detailed in Chapter 10.
Bilateral cataracts occasionally occur with a rapid onset in severe juvenile diabetes. The lens may become completely opaque in several weeks.
Typical senile nuclear sclerosis, posterior subcapsular changes, and cortical opacities occur earlier and more frequently in diabetics.
Especially when diabetes is not well controlled, changes in blood glucose levels may cause changes in refractive power by as much as 3 or 4 diopters of hyperopia or myopia.
Glycogen infiltration of the pigment epithelium and sphincter and dilator muscles of the iris may cause diminished pupillary responses. The reflexes may also be altered by the autonomic neuropathy of diabetes.
Rubeosis iridis is a serious complication of the retinal ischemia that is also the stimulus to retinal neovascularization in severe diabetic retinopathy. Numerous small intertwining blood vessels develop on the anterior surface of the iris. Spontaneous hyphema may occur. Formation of peripheral anterior synechiae blocks aqueous outflow resulting in secondary (rubeotic) glaucoma.
This common occurrence in diabetes is manifested by a sudden onset of diplopia, caused by paresis of one or more extraocular muscles due to infarction of one of the ocular motor nerves. It may be the first manifestation of diabetes. When the third nerve is involved, pain may be a prominent symptom. Differentiation from a posterior communicating aneurysm is important; in diabetic third nerve palsy, the pupil is usually spared. Recovery of ocular motor function begins within 3 months after onset and usually is complete. The fourth and sixth nerves may be similarly involved.
Visual loss is usually due to infarction of the optic disk (nonarteritic anterior ischemic optic neuropathy). Diabetic papillopathy manifests as chronic optic disk swelling, usually with mild visual impairment.
Endocrine Diseases
Thyroid Gland Disorders
The term Graves’ disease denotes hyperthyroidism due to an autoimmune process. A small proportion of patients with Graves’ disease develop characteristic eye signs known as Graves’ ophthalmopathy or thyroid eye disease (see also Chapter 13). In addition to signs of thyrotoxicosis, patients may have pretibial myxedema and (rarely) clubbing of the fingers. The ophthalmopathy may appear before any manifestations of thyrotoxicosis. It also may occur in autoimmune hypothyroidism (Hashimoto’s thyroiditis); thyroid dysfunction due to amiodarone (see later in the chapter); in association with thyroid antibodies without thyroid dysfunction; and occasionally in the absence of thyroid antibodies and clinical and laboratory evidence of thyroid dysfunction. It is exacerbated by radioiodine therapy, especially if the patient smokes cigarettes.
Patients may present with nonspecific complaints such as dryness, discomfort, or prominence of the eyes. Mourits developed a clinical scoring system that uses the signs and symptoms which reflect the cardinal features of inflammation (Table 15–2). The Mourits score can be used to assess changes in disease activity with time and response to therapy.
| Pain |
| Painful, oppressive feeling on or behind globe |
| Pain on attempted up, side, or down gaze |
| Redness |
| Redness of the eyelids |
| Diffuse redness of the conjunctiva |
| Swelling |
| Chemosis (conjunctival edema) |
| Swollen caruncle |
| Edema of the eyelids |
| Increase in proptosis of 2 mm or more over a period of 1–3 months |
| Impaired function |