Chapter 47 Non-Neural Complications of Thyroid and Parathyroid Surgery
Introduction
Complications of contemporary thyroid and parathyroid surgery are infrequent. Paramount in the minds of surgeons are the avoidance of laryngeal nerve injury, both superior and recurrent, and the preservation of functional parathyroid glands. Many other important complications, however, may occur perioperatively. These complications include metabolic disturbances, hemorrhage, wound problems, tracheal or esophageal injuries, airway obstruction, and other case-specific problems. This chapter focuses on the non-neural complications of head and neck endocrine surgery (see Chapters 45, Pathophysiology of Recurrent Laryngeal Nerve Injury, and 46, Management of Recurrent Laryngeal Nerve Paralysis).
Hypoparathyroidism
Hypoparathyroidism is a potentially serious complication following neck surgery that can lead to myriad metabolic and physiologic disturbances, prolonged hospitalization, and the need for lifelong supplementation. It is recognized as the most common complication of thyroid and parathyroid surgery. Temporary hypoparathyroidism occurs in approximately 10% to 15% of patients, whereas permanent hypoparathyroidism rates are much less common being in the 1% to 3% range.1–10
Both direct (excessive manipulation, cautery, or unintended removal) and indirect (devascularizing) injury can result in hypoparathyroidism. The risk of hypoparathyroidism increases with the extent of thyroidectomy, completion thyroidectomy, or reoperative procedures. Additionally, central compartment neck dissection increases the risk for hypoparathyroidism.10–13 In general, intimate knowledge of parathyroid anatomy and careful tissue handling reduce the risk of this complication (see Chapter 30, Principles in Thyroid Surgery).
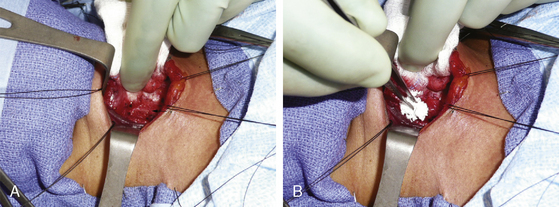
During the course of surgery, any parathyroid gland that appears to be devascularized should be autoimplanted after frozen section confirmation.10 This is recognized by a gland that becomes dusky or even black throughout the course of surgery or a gland that accompanies the thyroid specimen as the latter is removed (Figure 47-1). Autoimplantation is accomplished by sectioning the gland with a sharp scalpel into 1-mm pieces and placing it into a pocket of strap musculature14 and tagging it with a permanent suture or vascular clip. Another technique involves suspending the tissue in saline and injecting it with a syringe and needle into the muscle (Figure 47-2). These maneuvers have been shown to decrease rates of permanent hypoparathyroidism.14–17 Implanted glands have a more predictable survival compared to devitalized glands that are left in situ.15 Following thyroidectomy, a thorough examination of the surgical specimen should be undertaken to identify any parathyroid gland that has been inadvertently removed. Any glands that are identified should be considered for autoimplantation. A complementary practice is for the pathologist to comment on any parathyroid tissue that accompanies the surgical specimen when reviewed to inform the surgeon of inadvertently removed glands. This provides important information regarding the number of remaining glands.
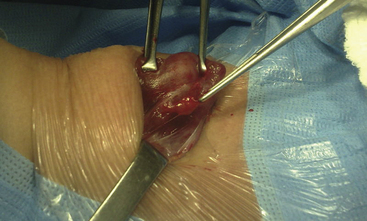
Figure 47-1 Right superior parathyroid gland devitalized and attached to the delivered thyroid specimen.
The signs and symptoms of hypocalcemia can be subtle and include perioral or digital paresthesias, muscle cramping, or anxiety. Furthermore, Chvostek sign, facial twitching when the facial nerve is tapped, and Trousseau sign, ischemia-induced carpal spasm (i.e., from a sphygmomanometer), highlight the state neuromuscular excitability during hypocalcemia. Importantly, Chvostek sign may be positive in up to 20% of normocalcemic individuals. More overt and alarming signs and symptoms include tetany, altered mental status, seizures, prolonged QT interval, heart failure, bronchospasm, and laryngospasm. Postoperative calcium and rapid PTH assays have been shown to predict those patients who are at risk for hypocalcemia.18–24 Those patients who have positive sloping calcium levels over 12 hours or who remain in the normal range are predicted to have normocalcemia.18,20 Additionally, those with rapid PTH levels of less than 10 mg/dL at 1 hour or 4 hours postoperatively are at risk for hypocalcemia.21,24 Both corrected serum and ionized calcium levels can be followed serially to monitor trends and response to treatment.
Treatment for hypocalcemia relates to its degree and duration. The goal is to maintain a low-normal calcium level, thereby controlling symptoms while avoiding any toxicity. Acute symptomatic hypocalcemia is treated with intravenous calcium gluconate when a peripheral intravenous catheter is used to avoid tissue necrosis, should intravenous fluid extravasation occur. Calcium chloride may be used when a central venous catheter is present. Concurrently, oral calcium supplementation is started to provide 2 g to 10 g daily in divided doses. It is important to note that different calcium preparations provide different levels of elemental calcium25 (Table 47-1). Furthermore, calcium carbonate requires an acidic environment for absorption. Therefore, it is best taken with meals and avoided in those patients who take histamine blockers or proton pump inhibitors. Calcitriol can be started simultaneously when oral calcium supplementation is initiated. Temporary hypocalcemia usually resolves within 4 weeks of surgery but may last longer.26 Interval calcium and parathyroid hormone levels should be checked to monitor for recovery. Permanent hypocalcemia is defined as those who require continued calcium and vitamin D supplementation at 1 year postoperatively.
Table 47-1 Elemental Calcium by Preparation
| Percentage of Elemental Calcium | |
|---|---|
| Calcium carbonate | 40 |
| Calcium citrate | 21 |
| Calcium lactate | 13 |
| Calcium gluconate | 9 |
| Calcium glubionate | 6.6 |
Hypothyroidism
Hypothyroidism after total thyroidectomy is expected, and this should be discussed with the patient preoperatively. Naturally, this iatrogenic state requires replacement therapy. The starting dose of L-thyroxine is 1.8 mcg/kg daily. The does is then adjusted based on serum thyroid-stimulating hormone (TSH) levels that are measured between 4 to 6 weeks after treatment is initiated. In those who require suppression therapy for the treatment of well-differentiated thyroid carcinoma, the dose is adjusted such that the TSH is low (i.e., suppressed; see Chapter 50, Postoperative Management of Differentiated Thyroid Cancer).
Following thyroid lobectomy, hypothyroidism occurs in 15% to 50% of patients.27–32 Those with low preoperative levels of free T4, higher preoperative TSH levels, Hashimoto’s thyroiditis, and a small remnant thyroid lobe are at increased risk.31,32 Patients may have subclinical hypothyroidism and routine thyroid function tests should be checked 4 to 6 weeks after surgery. Of those who are initially determined to be hypothyroid, a minority of patients may become euthyroid over time30 and subsequently can be weaned from replacement therapy. In such patients, routine monitoring of thyroid function is required to ensure that a euthyroid state persists.
Thyrotoxic Storm
Thyrotoxic storm or crisis is a rare but life-threatening complication of thyroid surgery. This entity represents the extreme manifestations of thyrotoxicosis. It most frequently occurs in patients with Graves’ disease, toxic thyroid nodules, and multinodular goiters (see Chapter 9, The Surgical Managment of Hyperthyroidism). Typically, a precipitating event such as surgery, trauma, infection, myocardial infarction, and other systemic events will transform thyrotoxicosis to thyroid storm. Also, this can be precipitated with excess iodine intake such as with iodinated contrast agents or amiodarone exposure. The physiology surrounding this event is the sudden disassociation of thyroid hormone from its binding proteins. This increase in free thyroid hormone can then lead to the constellation of signs and symptoms as it affects the neurologic, cardiopulmonary, gastrointestinal, and other systems. Common signs and symptoms include fever, tachycardia, cardiac arrhythmias, and, in extreme cases, cardiovascular collapse, hepatic failure, and death.33 Perioperatively, these events should not be confused with malignant hyperthermia.
Thyroid storm is best prevented. Patients who undergo thyroid surgery for thyrotoxicosis should be evaluated by an endocrinologist. Antithyroid medications are universally administered, and beta-blockade is commonly used to control the systemic effects. In those with poorly controlled thyrotoxicosis requiring urgent thyroidectomy, preoperative iopanoic acid (i.e., 500 mg bid), dexamethasone (i.e., 1 mg bid), propylthiouracil or methimazole, and beta-blockade have been shown to decrease the likelihood of thyroid storm.34
Hemorrhage and Hematoma
Hemorrhage and hematoma formation after thyroid and parathyroid surgery can be life threatening. Fortunately, this complication occurs in less than 2% of thyroid and parathyroid operations.35–40 Predicting those patients who are at risk for this complication is difficult. Two recent studies have identified age and male gender as risk factors.35,41 Furthermore, malignancy and bilateral surgical procedures also increase the risk for postoperative hemorrhage.41 Traditionally, placement of either a passive or active neck drain was advocated to reduce the likelihood of this complication. Multiple studies, however, have shown that postoperative hemorrhage and hematoma rates are equivalent in patients who have and have not been drained.42–45 These conclusions are supported by two recent meta-analyses.46,47 Therefore, the need for wound drainage should be determined by the surgeon on a case-by-case basis, and a drain should not be relied on to prevent hematoma formation.
Intraoperatively, meticulous hemostasis should be maintained. Any bleeding encountered near the recurrent laryngeal nerve should be treated with judicious use of bipolar electrocautery. Additionally, cellulose-based hemostatic agents or microfibrillar collagen may be a useful adjunct when electrocautery is deemed unsafe (Figure 47-3). Furthermore, fibrin sealants and thrombin have been examined as a potentially useful adjunct in thyroid surgery.48–50 At present, newer vessel-sealing devices have not been shown to decrease hematoma rates.51–55
Prior to closing the wound, the Valsalva maneuver can be performed repetitively or the patient placed in the Trendelenburg position, and any identified bleeding sites are identified and controlled. Cervical pressure dressings, such as the Queen Anne, have been advocated in the past. These dressings, however, are cumbersome and may delay the recognition of a hematoma. These dressings do not prevent hematoma formation56 and, therefore, are not recommended. The patient should be awakened from anesthesia deeply to avoid coughing. Perioperative antiemetics are used to decrease the risk of emesis even though they have not been shown to affect hematoma rates.37 Taking these precautions and utilizing meticulous surgical technique will decrease the risk of hemorrhage.
The timing of postoperative hematomas can range from immediate to several days postoperatively. The majority of hematomas, however, occur within the first 24 hours of surgery.38,44 The signs and symptoms of hematomas include neck swelling, pain, oozing from the suture line, ecchymosis, dysphagia/odynophagia, stridor, and respiratory distress (Figure 47-4). Hematomas are classified as superficial or deep depending on their relationship to the strap muscles.36 Deep hematomas are thought to cause respiratory distress and airway compromise by causing venous congestion and subsequent laryngopharyngeal edema. It has been advocated that the strap muscles be reapproximated loosely or incompletely to allow for egress of any accumulating deep neck hematoma.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree