Nasopharyngeal Carcinoma
William Ignace Wei
Daniel T. T. Chua
Anatomically, the nasopharynx is situated behind the posterior choanae and is continuous with the posterior aspect of the nasal cavities. Inferiorly, it is separated from the oropharynx by the soft palate and it is the air passage during breathing. Because of its bony framework, it remains patent under normal circumstances. Nasopharyngeal carcinoma (NPC) is a squamous cell carcinoma (SCC) arising from the epithelial lining of the nasopharynx. This neoplasm may arise from any site in the nasopharynx and is more frequently seen at the lateral wall, from the fossa of Rosenmüller, the recess located medial to the medial crura of the opening of the auditory tympanic tube or the Eustachian tube.
A group of 14 patients suffering from this malignancy was first reported in the English literature in 1901 (1). The first comprehensive series reporting clinicopathologic features of 114 patients suffering from NPC in Hong Kong was published in 1941 (2).
NPC is a relatively uncommon malignant disease in most countries with its age-adjusted incidence being less than 1 per 100,000 (3). It constitutes 0.7% of all cancers, and is rated the 23rd common new cancer in the world (4). It occurs frequently in the Inuits of Alaska (5) and ethnic Chinese in Southern part of China, especially from the province of Guangdong. The recent reported incidence of NPC among men and women in Hong Kong, in the southern part of the Guangdong province, was 17.8 per 100,000 and 6.7 per 100,000, respectively (3). A range of intermediate rates are observed in populations of North Africa (6) and the Middle East (7). The incidence of NPC remains high among those Chinese who have immigrated to Southeast Asia countries or North America, but is low among those Chinese born in North America (8,9). This suggests that genetic, ethnic, and environmental factors may play a role in the etiology of the disease.
One of the etiologic factors of NPC frequently referred to is the consumption of salted fish. This may be related to the carcinogenic compound, nitrosamine, detected on the salted fish (10). A case-control study has shown that weekly consumption of salted fish before 10 years of age is associated with a threefold increased risk of developing NPC (11). The consumption of salted fish at childhood rather than adulthood contributes to the increased incidence (12). The Epstein-Barr virus (EBV) has also been considered to play an oncogenic role in this tumor, as the EBV genome is frequently detected in the biopsy specimens of NPC (13). Additionally, patients suffering from NPC also have higher EBV antibody titers than controls, especially the IgA antibodies to viral capsid antigen (VCA) and early antigen (EA) (14,15).
In view of the ubiquitous presence of this virus in the human population, it is unlikely that EBV is the only causative agent of NPC. In the first-degree relatives of patients suffering from NPC, their incidence of developing this malignancy is 4 to 10 times higher than controls (16). This suggests that genetic factor might have an important role in the etiology of NPC. Comparative genomic hybridization studies have demonstrated several genomic spots where chromosomal losses and gains were identified in NPC (17). These losses on chromosomes 3p, 9p, 11q, 13q, and 14q suggested that tumor suppressor genes at these loci might be involved in NPC development (18,19).
HISTOPATHOLOGY
The malignant epithelial cells of NPC are large polygonal cells with a syncytial character. Their nuclei are round or oval with scanty chromatin and distinct nucleoli. The cells are frequently intermingled with lymphoid cells in the nasopharynx, giving rise to the term lymphoepithelioma (20). Electron microscopy studies have confirmed the squamous origin of these cells including those undifferentiated
carcinoma that are a form of epidermoid SCC with minimal differentiation (21).
carcinoma that are a form of epidermoid SCC with minimal differentiation (21).
The histologic classification of NPC proposed by the World Health Organization (WHO) (22) in 1978 categorized tumors into three groups:
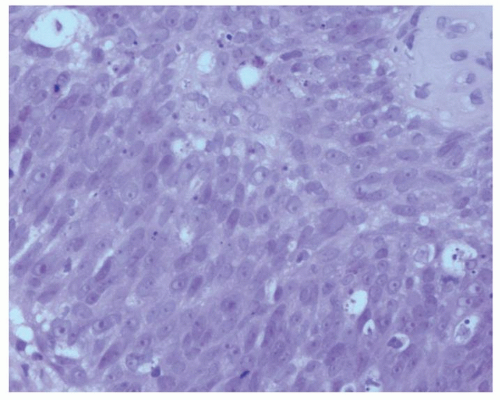
Type I included those typical keratinizing SCCs with intercellular bridges, similar to those found in the rest of the upper aerodigestive tract (Fig. 120.1).
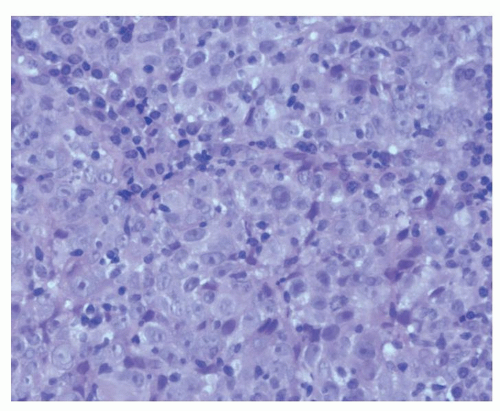
Type II included nonkeratinizing epidermoid carcinomas. They showed evidence of maturation but without definite squamous differentiation (Fig. 120.2).
Type III included undifferentiated carcinomas or poorly differentiated carcinoma. These cells have indistinct cell margins with hyperchromatic nuclei (Fig. 120.3).
In North America, around 25% of patients have tumor with Type I histology, 12% with Type II, and 63% with Type III. The corresponding histologic distribution in southern Chinese patients is 3%, 2%, and 95%, respectively (23).
An alternative classification divided tumors into two histologic types, namely, SCCs and undifferentiated carcinomas of the nasopharyngeal type (UCNTs) (24). This second classification took into consideration the correlation of the tumor with EBV serology. Patients with SCCs have a lower EBV titer, while those with UCNTs have elevated titers.
On clinical grounds, biopsies obtained from patients suffering from NPC sometimes show a mixed histologic pattern. The recent WHO classification has taken this mixed pattern into account as well as the association of the EBV with Type II and III tumors. The histologic types of NPC are classified into two groups; the first group comprises the SCCs or nonkeratinizing carcinomas, and the second group is subdivided into differentiated and undifferentiated carcinomas (25). This new classification has also been shown to have a prognostic bearing; the undifferentiated carcinomas have a higher local tumor control rate with radiotherapy (RT) and a higher incidence of distant metastasis (26,27).
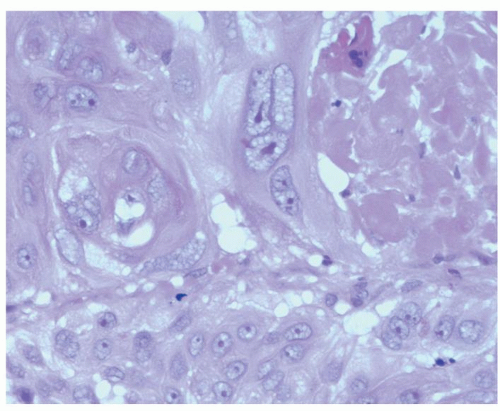 Figure 120.1 SCC of the nasopharynx. The tumor cells are large with eosinophilic cytoplasm and show features of keratinization (hematoxylin and eosin ×400). |
CLINICAL PRESENTATIONS
Comparing with other head and neck cancers, NPC affects relatively younger age group of patients (28). Patients suffering from NPC may present with one or more of the four groups of symptoms. These groups of symptoms are
related to the location of the primary tumor, infiltration of structures in the vicinity of the nasopharynx, or metastasis to cervical lymph nodes.
related to the location of the primary tumor, infiltration of structures in the vicinity of the nasopharynx, or metastasis to cervical lymph nodes.
The presence of tumor mass in the nasopharynx may lead to the symptoms of nasal obstruction and discharge. With a small tumor, the obstruction is unilateral and with tumor growth the symptoms may become bilateral. When the tumor ulcerates, the patient may present with epistaxis. The amount of bleeding is usually trivial and the frequent presentation is the presence of altered blood in the postnasal drip, especially in the morning.
The tumor bulk in the nasopharynx with or without posterolateral extension into the paranasopharyngeal space is frequently associated with dysfunction of the Eustachian tube. This may lead to the collection of fluid in the middle ear and the patients may experience unilateral deafness that is conductive in nature and other otologic symptoms such as otalgia and tinnitus. When a Chinese adult patient presents with serous otitis media, the otolaryngologist should consider the possibility of NPC (29).
When the primary tumor grows superiorly to infiltrate the skull base, the patient experiences headache. When the upward extension of tumor affects the cavernous sinus and its lateral wall, cranial nerves III, IV, and VI may be affected and the patient will present with diplopia (Fig. 120.4). When the tumor extends to involve the foramen ovale, the cranial nerve V may be affected (30) and there may be facial pain and numbness. Cranial nerve involvement in patients suffering from NPC is in the region of 13% (31) to 30% (32) depending on the stage of the disease.
 Figure 120.4 Clinical photograph showing a patient with paralyzed right eye lateral rectus muscle due to involvement of the right abducent nerve by NPC. |
In view of the high propensity of NPC to metastasize to cervical lymph nodes, the most frequent presenting symptom is painless neck masses, frequently appearing in the upper neck (Figs. 120.5 and 120.6). As the nasopharynx is a midline structure, it is not uncommon to see patients presenting with bilateral cervical lymph nodes.
Patients presenting with symptoms related to distant metastasis are relatively uncommon in NPC. Common distant metastatic sites are the vertebra, liver and lung.
Unfortunately, because of the nonspecific nature of the nasal and aural symptoms and the inconspicuous nature of the painless cervical lymph node, the majority of NPC patients are only diagnosed when their tumor have reached advanced stages. A retrospective analysis of 4,768 patients showed that the symptoms at presentation were neck mass
in 76%, nasal symptoms in 73%, aural symptoms in 62%, and cranial nerve palsy in 20% of patients (33). In most reports, the male-to-female ratio was 3:1, and the median age was 50 years.
in 76%, nasal symptoms in 73%, aural symptoms in 62%, and cranial nerve palsy in 20% of patients (33). In most reports, the male-to-female ratio was 3:1, and the median age was 50 years.
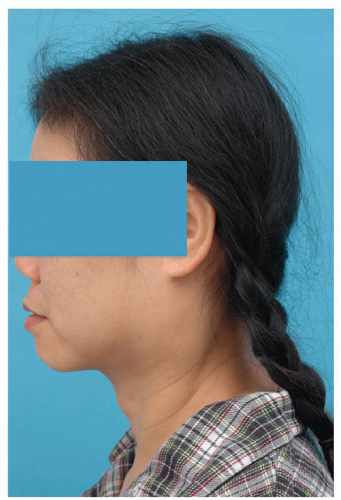 Figure 120.5 Clinical photograph showing a patient with an enlarged upper cervical lymph node (lateral view). |
DIAGNOSIS
When patients present with symptoms of NPC, they should be evaluated clinically for physical signs of NPC such as the presence of lymph nodes in the neck, fluid in the middle ear, and cranial nerve involvement. Indirect examination of the postnasal space should be carried out with a mirror although, in some patients, the anatomical variation of the nasopharynx precludes an adequate evaluation of the region. Other investigations toward the diagnosis of NPC are the estimation of antibody levels against EBV, imaging studies and endoscopic examination of the nasopharynx, and biopsy.
SEROLOGY
EBV affects human in various forms. It may cause infectious mononucleosis and has also been found to be associated with Burkitt lymphoma and NPC. EBV belongs to the herpes virus family, and the EBV-specific antigens can be grouped into early replicative antigens, latent-phase antigens, and late antigens. In patients suffering from NPC, their antibody, immunoglobulin A (IgA), response to the EA of the first group, and the VCA of the third group have been shown to be of diagnostic value (34). When a spectrum of antibodies against one of the latent-phase antigens, the EBV-associated nuclear antigen (EBNA), was evaluated, both the specificity and sensitivity of the test exceed 92% (35).
Most of the studies on the EBV serology for early diagnosis of NPC were carried out in the 1980s. In a recent meta-analysis on 20 these types of studies showed that IgA anti-VCA when elevated has a sensitivity of 91% and specificity of 92% in the diagnosis of NPC (36). A recent report from Taiwan studied 9,699 men, who had a one-off blood sample for their EBV serology, and this was subsequently correlated with the cancer registry and death registry over a 15-year period. Those with elevated anti-EBV titers have a 30 times more chance of developing NPC (15). The level of IgA anti-VCA in monitoring tumor response to treatment and in the detection of recurrence has not been established.
In recent years, cell-free DNA of the EBV in NPC patients was detected by real-time quantitative PCR, and it has been evaluated as a tumor marker (37). Increased copies of EBV DNA were found in the blood during the initial phase of RT as the viral DNA was released into the circulation after cell death (38). This has been shown to be more sensitive than the antibody titers against the various EBV antigens in the diagnosis of NPC (39). The quantity of free plasma EBV DNA has been shown relating to the stage of disease (40), and it is reliable in detecting distant metastases (41). The quantities of EBV DNA copies detected before and after treatment were significantly related to the rates of overall and disease-free survival (42). It has also been used to monitor recurrent disease following treatment (43); however, elevated levels of EBV DNA were only detected in 67% of patients with small locoregional recurrence (44).
IMAGING STUDIES
Clinical examination together with endoscopic examination can provide valuable information on tumor extension on the mucosal surface in nasopharynx. This procedure cannot determine the third dimension of tumor growth, that is, its deep extension and this includes skull base erosion and intracranial spread. This information is provided by cross-sectional imaging studies (45). These investigations are essential to document the extent of disease in the nasopharynx and its involvement of surrounding tissue. They are mandatory for the planning of RT.
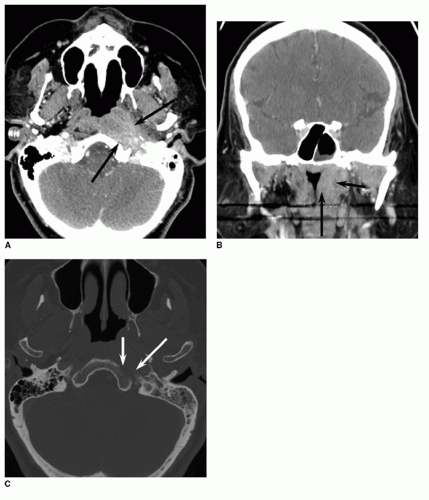
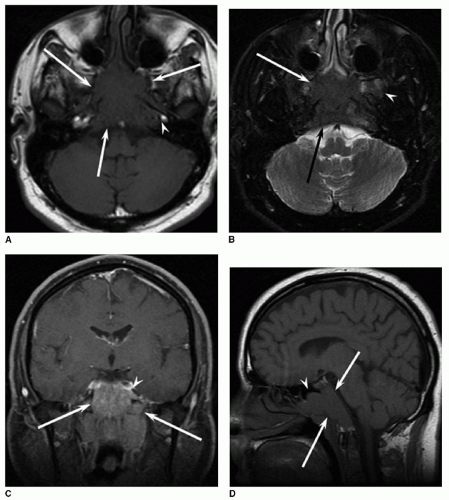
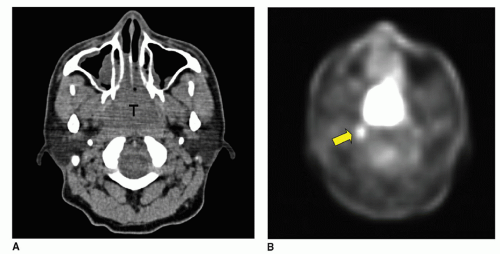
Computed tomography (CT) can demonstrate the soft tissue extension in the nasopharynx and laterally into the paranasopharyngeal space (Fig. 120.7). It is sensitive in detecting bone erosion especially that of the skull base (46) (Fig. 120.7). Intracranial tumor extension through the foramen ovale with perineural spread can also be detected and this provides evidence of cavernous sinus involvement without skull base erosion (47). The information provided through CT is important for staging and also the choice of therapeutic measures for some patients (48). CT is capable of showing bone regeneration after therapy and this indicates complete eradication of tumor (49). CT, however, in general has poor tumor enhancement and in contrast magnetic resonance imaging (MRI) has better soft tissue specificity. Besides its ability to provide multiplanar imaging abilities (Fig. 120.8),
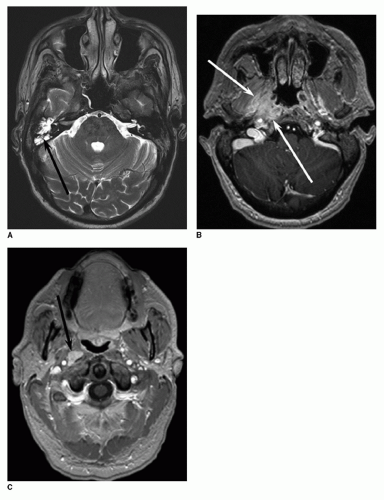
MRI is better than CT in the differentiation of tumor from soft tissue inflammation, especially in the paranasal sinuses (Fig. 120.9). MRI is also more sensitive at evaluating retropharyngeal and deep cervical nodal metastases (Figs. 120.10 and 120.11). MRI is able to detect bone marrow infiltration by tumors (50), while CT can only detect this kind of infiltration when there is associated bony erosion. MRI, however, is unable to evaluate details of bone erosion.
MRI is better than CT in the differentiation of tumor from soft tissue inflammation, especially in the paranasal sinuses (Fig. 120.9). MRI is also more sensitive at evaluating retropharyngeal and deep cervical nodal metastases (Figs. 120.10 and 120.11). MRI is able to detect bone marrow infiltration by tumors (50), while CT can only detect this kind of infiltration when there is associated bony erosion. MRI, however, is unable to evaluate details of bone erosion.
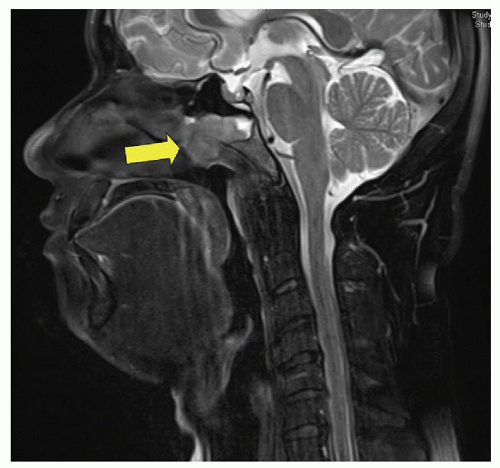
Another contribution of cross-sectional imaging in NPC is the therapeutic aspects. As CT or MRI determines the primary tumor extent with precision (Figs. 120.12, 120.13 and 120.14), it enables RT treatment to be designed and administered accurately and effectively, resulting in an improved outcome (51). This is particularly applicable with the intensity modulated radiotherapy (IMRT), which makes use of composite CT-MRI targets (52), enabling radiation energy to be targeted even more accurately to
tumor while at the same time sparing adjacent normal tissues.
tumor while at the same time sparing adjacent normal tissues.
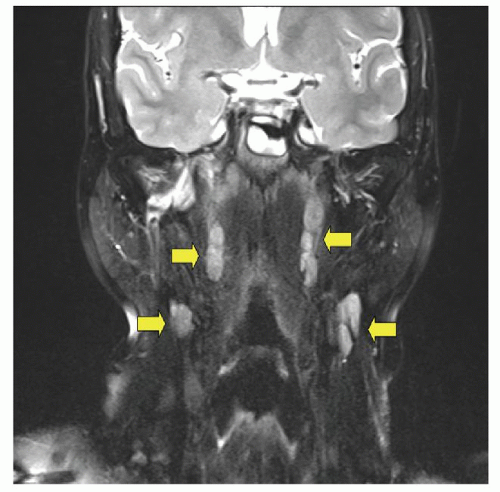 Figure 120.10 Coronal T2-weighted MRI demonstrates multiple bilateral pathologically enlarged cervical lymph nodes (arrows), representing metastatic NPC. |
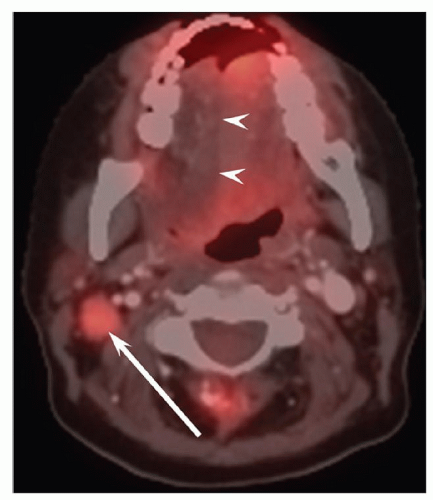
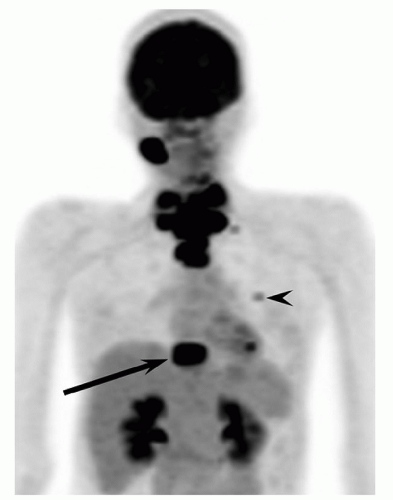
Positron emission tomography (PET) is useful to show the primary NPC with the metastatic lymph nodes (Figs. 120.15 and 120.16). For locally advanced NPC, the fluor-18-fluorodeoxyglucose (18F-FDG) uptake as measured by standard uptake value (SUVmax) has been shown to have prognostic significance (53); those patients with SUVmax of higher than five have poor outcome (54). The hypermetabolic site locates the presence of tumor (Fig. 120.17).
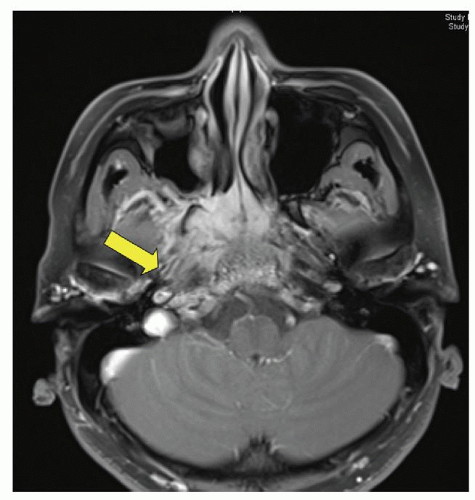 Figure 120.12 Axial fat-suppressed enhanced T1-weighted MRI shows NPC invading the greater sphenoid wing (arrow). |
The detection of distant metastases at diagnosis is difficult. Conventional studies such as bone scans, liver scintigraphy (55), and marrow biopsy (56) are of little value. They should only be carried out for those patients with high risk of distant spread such as those with N3 disease (57).
The role of PET in the detection of distant metastases in NPC and other malignancies was first noted in 2003 (58) (Fig. 120.18). In newly diagnosed NPC, PET is not more sensitive than MRI in the detection of distant metastasis (59). PET, however, has also been reported to
be more sensitive than cross-sectional imaging studies in detecting persistent and recurrent NPC (60), both at the primary site and in the neck. A recent systemic review showed that PET was better with dual-section and multisection helical CT (61).
be more sensitive than cross-sectional imaging studies in detecting persistent and recurrent NPC (60), both at the primary site and in the neck. A recent systemic review showed that PET was better with dual-section and multisection helical CT (61).
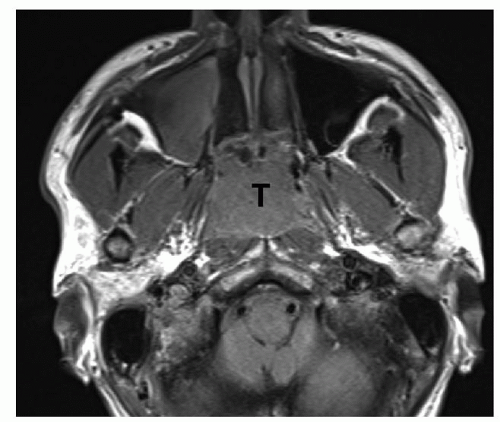 Figure 120.13 Axial unenhanced T1-weighted image shows a bulky tumor (T) filling the nasopharynx and extending into the nasal cavity bilaterally. |
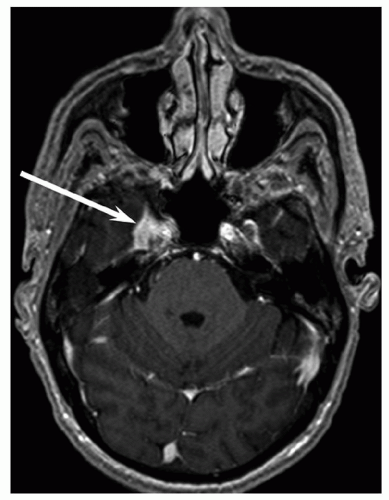 Figure 120.14 Axial T1-weighted MRI shows an enhancing mass (arrow) in the cavernous sinus and right middle cranial fossa, representing direct spread of NPC. |
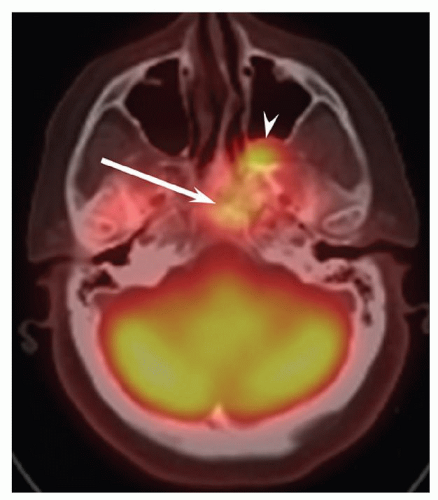 Figure 120.15 Combined PET-CT axial image shows increased activity in the middle skull base (arrow) and in the pterygopalatine fossa (arrowhead), demonstrating direct spread of primary NPC. |
In summary, MRI is the preferred modality for local staging and detection of local recurrence. In patients with advanced disease, a PET/CT from the skull base to mid-thigh is useful to ascertain the extent of disease in the body.
ENDOSCOPIC EXAMINATION
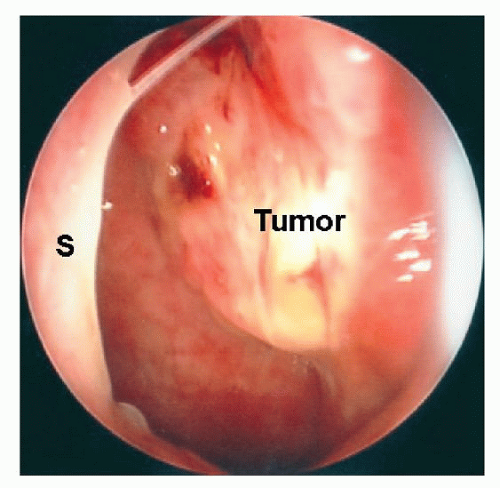
The confirmation of the diagnosis of NPC requires a positive biopsy taken from the tumor in the nasopharynx. The nasopharynx can be adequately examined under topical anesthesia with endoscopes (Fig. 120.19). The rigid Hopkins telescopes, both 0° and 30°, give an excellent view of the nasopharynx on the side of insertion (Figs. 120.20 and 120.21). A 70° endoscope inserted behind the soft palate allows visualization of the roof of nasopharynx and both Eustachian tube openings (Fig. 120.22). These 3- or 4-mm-diameter rigid endoscopes do not have a suction or biopsy channel. Blood and mucus covering the tumor have to be removed by a separate suction catheter for a clear view of the pathology. Biopsy forceps should also be inserted alongside the endoscope for taking a biopsy of the tumor under direct vision.
The flexible endoscope allows thorough examination of the entire nasopharynx even when it is inserted through one nasal cavity. Its tip can be maneuvered behind the nasal septum to the opposite side. It has a suction channel and a biopsy forceps can be inserted through it to take a biopsy of the tumor under direct vision (Figs. 120.23
and 120.24). Despite all these advantages, the visual image gathered with the flexible endoscope is inferior to that of the rigid endoscope. The size of the biopsy forceps is also small thus the amount of tissue obtained might not be enough. Sometimes a larger biopsy forceps might have to be inserted by the side of the flexible endoscope to obtain more substantial amount of tissue for histologic examination.
and 120.24). Despite all these advantages, the visual image gathered with the flexible endoscope is inferior to that of the rigid endoscope. The size of the biopsy forceps is also small thus the amount of tissue obtained might not be enough. Sometimes a larger biopsy forceps might have to be inserted by the side of the flexible endoscope to obtain more substantial amount of tissue for histologic examination.
STAGING
A clinical staging system for NPC is essential for treatment planning and evaluation of therapeutic outcome. Over the years, a few staging systems were used for NPC; the Union International Contre le Cancer (UICC) system and the American Joint Committee on Cancer Staging (AJCC) system are preferred in Europe and America, respectively, while Ho system (62) is frequently used in Asia.
Both the UICC and the AJCC systems assess tumor extent in the nasopharynx by considering the number of tumor-affected sites within the nasopharynx while the
Ho system classifies all tumors confined to the nasopharynx as T1 disease. UICC and AJCC systems have unified since 1992. In the recent staging system of 2009, T1 stage included all tumors that confine to the nasopharynx or extend locally such as inferiorly to the oropharynx or anteriorly to the nasal cavity (63,64) (Table 120.1). On the other hand, lateral tumor extension to the paranasopharyngeal space indicates more advanced disease. T2 stage includes tumor that has extended to the paranasopharyngeal space. The T3 disease covers tumors that have involved the skull base or the paranasal sinuses. T4 tumors are those that have extended to the infratemporal fossa, orbit, hypopharynx, and cranium, or have affected the cranial nerves.
Ho system classifies all tumors confined to the nasopharynx as T1 disease. UICC and AJCC systems have unified since 1992. In the recent staging system of 2009, T1 stage included all tumors that confine to the nasopharynx or extend locally such as inferiorly to the oropharynx or anteriorly to the nasal cavity (63,64) (Table 120.1). On the other hand, lateral tumor extension to the paranasopharyngeal space indicates more advanced disease. T2 stage includes tumor that has extended to the paranasopharyngeal space. The T3 disease covers tumors that have involved the skull base or the paranasal sinuses. T4 tumors are those that have extended to the infratemporal fossa, orbit, hypopharynx, and cranium, or have affected the cranial nerves.
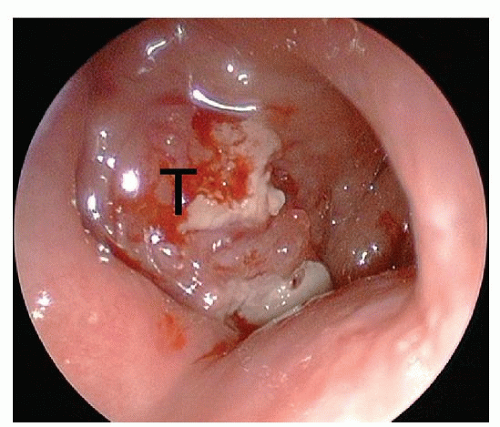 Figure 120.19 Rigid endoscope (0°) inserted through the right nasal cavity showing a fleshy tumor in the nasopharynx (T). |
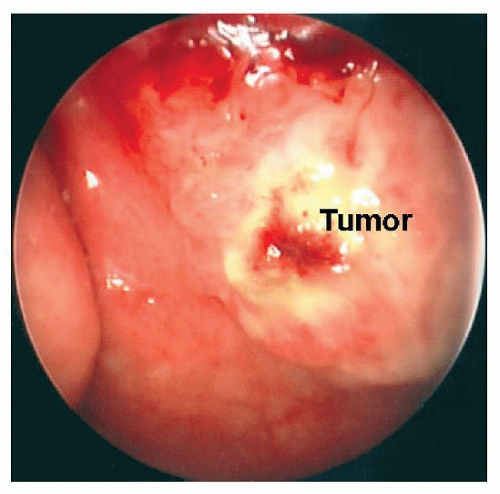 Figure 120.20 Rigid endoscope (0°) inserted through the right nasal cavity and tumor in the nasopharynx is identified (Tumor). |
The UICC/AJCC staging systems recognize the size of the cervical lymph node as an important factor. For other head and neck cancers, N1 is less than 3 cm in size and N2 is greater than 3 cm. The difference between N2 and N3 is a nodal size of 6 cm. The retropharyngeal nodes, which are the first-echelon nodes, are not taken into account by all staging systems. CT or MRI now detects these nodes (65).
 Get Clinical Tree app for offline access 
|