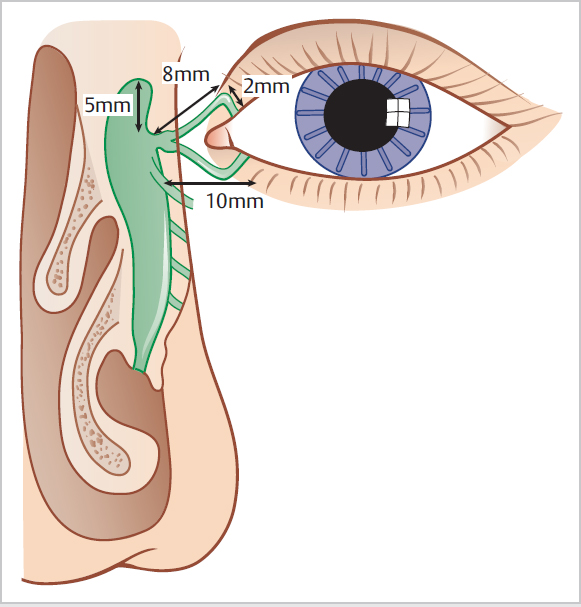
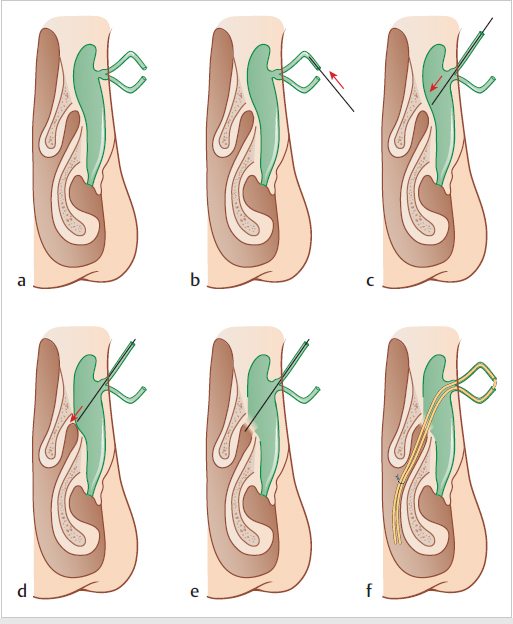
35 Nasolacrimal Disorders • The anatomy of the lacrimal system can be divided into the secretory, distributory, and drainage components: • Lacrimal sac sits in the lacrimal fossa that comprises the frontal process of the maxilla anteriorly and the lacrimal bone posteriorly • Frontal process of the maxilla is the dominant bone encountered during lacrimal surgery • The upper punctum lies slightly medial to the lower punctum • During blinking, the puncta come together • Initial portion of the canaliculi underneath the puncta is vertical and 2 mm in length • Canaliculi terminate in a saccular dilatation called “ampulla” surrounded by muscle, which can expand and contract with blinking, and may play a role in the drainage of tear through the canaliculus • The upper and lower canaliculi meet medially to form the common canaliculus • Average length of the common canaliculus is 1.2 mm (range 1–5 mm) • Enters lacrimal sac at an acute angle rather than at right angle (believed to prevent reflux of fluid back to the canaliculus when the sac is full) • The lacrimal sac varies in size, being 12 to 15 mm long and 4 to 8 mm deep • The anterior to posterior dimension of the lacrimal sac often limits the size of the lacrimal window in dacryocystorhinostomy (DCR) • The lacrimal sac courses posteriorly and inferiorly to become the nasolacrimal duct that terminates in the inferior meatus beneath the inferior turbinates • With blinking, closure of the palpebral aperture occurs from lateral to medial, thus propelling the tears toward the puncti—the compressive action of one lid against the other is important in the drainage of ears through the canaliculi • The transfer of tears through the lacrimal drainage system is predominately through active pumps in the eyelids, puncti, canaliculi, and sac • The valves within the lacrimal outflow system allow the unidirectional flow of tears from the canaliculi to the inferior meatus • The valve of Rosenmuller is situated at the internal opening of the common canaliculus within the lacrimal sac • The valve of Hasner lies at the distal opening of the lacrimal duct at the inferior meatus • Proximal: • Distal: sac and duct • Functional: related to poor lacrimal pump function, which may be due to a displaced punctum, eyelid laxity, weak orbicularis, or facial nerve palsy • Signs and symptoms of lacrimal blockage can be flow-related or volume-related. – The blurring is worse on down-gaze when the visual axis passes near the enlarged tear meniscus in the lower lid. Spillage of tear can lead to skin soreness – The intermittent backflow of the sac content causes blurred vision by strings of mucus making the lids stay closed in the morning – The dead space within the lacrimal sac causes bacterial overgrowth and predisposes the eye to recurrent conjunctivitis – Sometimes, a mass can appear at the inner canthus, from which debris can be expressed into the tear lake – If untreated, the lump can develop into a mucocele or pyocele, perhaps even resulting in a fistula • A well-performed dacryocystorhinostomy procedure with a complete marsupialization of the lacrimal sac within the nose should theoretically overcome 100% of volume-related symptoms. However, it may not eliminate all flow-related symptoms as they are limited by the conductance of the canaliculi • Congenital obstruction of the nasolacrimal duct: • Acquired obstruction of the lacrimal sac/duct can be non-specific or specific: – Most common in the elderly and female populations – Sarcoidosis – Wegener granulomatosis – Trauma—nasal fractures or injury from surgery on the maxilla or sinuses – Neoplasms involving the nasolacrimal sac/duct can arise: – Squamous cell papilloma – Transitional cell papilloma – Squamous cell carcinoma – Adenocarcinoma – Maxillary and ethmoid sinus tumour – Lymphoma • Approximately 1 in 3 cases of epiphora • Proximal lacrimal apparatus includes the canaliculi and their puncta with the caruncle separating the puncta • Aetiology: – Ocular pemphigoid – Stevens–Johnson syndrome – Phospholine iodide – Fluorouracil – HSV or iatrogenic effect of antivirals – Herpes zoster (and vaccine)—canalicular obstruction – Chlamydial infections – Radiotherapy—especially with dosing to basal cell carcinomas in the inner canthal area and for sinonasal tumours – Surgical removal of adjacent skin lesions – Papillomas – Basal cell carcinomas – Failed lacrimal surgery (10%) – Facial nerve palsy (2%) – Maxillary sinusitis (0.3%) – Lid abscess (0.3%) – Sarcoidosis (nasal) (0.3%) – Idiopathic (9%) • In the UK, patients with epiphora are initially referred to an ophthalmologist • However, there are certain lacrimal assessments that otolaryngologists should be familiar with • Inspection of the lid • Nasal examination • Fluorescein dye disappearance test • Jones I test • Finger pressure is applied on the lacrimal sac area; look for mucous or purulent discharge from the puncti • A positive test indicates patent canaliculus and the presence of dacryocystitis • The ophthalmologist may perform other tests to locate the level of lacrimal blockage, such as lacrimal irrigation, Jones II dye test, and lacrimal probing – Performed after a negative Jones I test – Lacrimal system is flushed by syringing and washing of excess fluorescein from the conjunctival sac – Test is positive if dye is detected on the cotton bud and this suggests functional obstruction of the nasolacrimal duct – Negative test indicates punctal or canalicular stenosis – Regurgitation indicates complete nasolacrimal duct obstruction or complete common canaliculus block – May be part diagnostic and part therapeutic, e.g., dislodging a stone – May be used in an attempt to palpate or localize the site of obstruction – Can measure the length of canalicular patency distal to the punctum, and from that estimate the length of the canalicular blockage • Contrast material is injected into the canaliculi • Enables visualization of the anatomical details of the lacrimal drainage system • Definitive test for assessing the nasolacrimal system • Digital subtraction techniques are now usually employed • Physiological assessment in which a drop of technetium is placed in the conjunctival culdesac and followed through the lacrimal system using a gamma camera • 10-μL drop of technetium-99 pertechnetate is placed on the marginal tear strip • Useful for assessing functional lacrimal duct obstruction—indicated by a delay or absence of transit of technetium into the nose • May be used as complementary investigation to ophthalmology tests • This may be indicated if trauma or neoplasms are suspected, or in certain cases where DCR is performed • If the stenosis is partial, or if the stenotic segment is limited, trephenation and bicanicular intubation is the treatment of choice.
35.1 Anatomy and Physiology of the Lacrimal System
 Secretory system = lacrimal glands
Secretory system = lacrimal glands
 Distributory system = eyelids
Distributory system = eyelids
 Lacrimal drainage system = lacrimal puncta, canaliculi, sac, and nasolacrimal duct (Fig. 35.1)
Lacrimal drainage system = lacrimal puncta, canaliculi, sac, and nasolacrimal duct (Fig. 35.1)
35.2 Classification of Lacrimal Obstruction
 Punctal stenosis/absence
Punctal stenosis/absence
 Single canalicular
Single canalicular
 Common canalicular (lateral or medial)—medial common canalicular blockage could be regarded as a distal blockage as it is usually caused by a membrane within the lacrimal sac closing offthe internal opening of the common canaliculus within a fibrotic lacrimal sac
Common canalicular (lateral or medial)—medial common canalicular blockage could be regarded as a distal blockage as it is usually caused by a membrane within the lacrimal sac closing offthe internal opening of the common canaliculus within a fibrotic lacrimal sac
35.3 Symptoms and Signs of Lacrimal Blockage
 Flow-related symptoms are due to low conductance within the canaliculi or nasolacrimal duct. This leads to excessive aqueous tears building up in the tear lake causing blurred vision
Flow-related symptoms are due to low conductance within the canaliculi or nasolacrimal duct. This leads to excessive aqueous tears building up in the tear lake causing blurred vision
 Volume-related symptoms are due to accumulation of fluid in the lacrimal sac and the backwash of the debris into the tear lake
Volume-related symptoms are due to accumulation of fluid in the lacrimal sac and the backwash of the debris into the tear lake
35.4 Diseases of the Lacrimal Sac and Duct
 Thought to be due to an imperforate valve of Hasner within the inferior meatus
Thought to be due to an imperforate valve of Hasner within the inferior meatus
 Common in children during their first year of life
Common in children during their first year of life
 High rate of spontaneous resolution
High rate of spontaneous resolution
 Persistent epiphora beyond the age of 1 year may require lacrimal probing to identify the level of the blockage
Persistent epiphora beyond the age of 1 year may require lacrimal probing to identify the level of the blockage
 Non-specific acquired nasolacrimal blockage is by far the commonest
Non-specific acquired nasolacrimal blockage is by far the commonest
 Specific acquired nasolacrimal blockage includes:
Specific acquired nasolacrimal blockage includes:
 Once the sarcoidosis and Wegener granulomatosis are controlled by steroids, the residual epiphora can be treated by dacryocystorhinostomy
Once the sarcoidosis and Wegener granulomatosis are controlled by steroids, the residual epiphora can be treated by dacryocystorhinostomy
 From tissues within the sac/duct:
From tissues within the sac/duct:
 Growth invading the sac/duct from the outside:
Growth invading the sac/duct from the outside:
35.5 Proximal Lacrimal Obstruction
 Congenital causes (10%): Absence or imperfection of lacrimal puncta and/or canaliculi (± obliteration of more distal parts of the lacrimal apparatus)
Congenital causes (10%): Absence or imperfection of lacrimal puncta and/or canaliculi (± obliteration of more distal parts of the lacrimal apparatus)
 Ciactrical conjunctival disorders (~2%)—subepithelial fibrosis of the conjunctiva
Ciactrical conjunctival disorders (~2%)—subepithelial fibrosis of the conjunctiva
 Drug-induced canalicular stenosis (2%)
Drug-induced canalicular stenosis (2%)
 Infective causes (30%)
Infective causes (30%)
 Thermal and traumatic injuries and radiotherapy-induced injury (34%)
Thermal and traumatic injuries and radiotherapy-induced injury (34%)
 Canalicular neoplasms (2%)
Canalicular neoplasms (2%)
 The causes cited above can cause lateral common canalicular obstructions in the same manner as they affect the individual canaliculi
The causes cited above can cause lateral common canalicular obstructions in the same manner as they affect the individual canaliculi
 Other miscellaneous causes
Other miscellaneous causes
35.6 Investigation of Lacrimal Obstruction
35.6.1 Examination
 Look for signs of punctual involvement, including position of puncta
Look for signs of punctual involvement, including position of puncta
 Any sign of weakness in opening and closing the eyelid should be noted
Any sign of weakness in opening and closing the eyelid should be noted
 If sclera show is evident on examining the relationship of the lower lid to the inferior limbus, a lacrimal pump problem may be present
If sclera show is evident on examining the relationship of the lower lid to the inferior limbus, a lacrimal pump problem may be present
 The role of the otolaryngologist is to pick up other nasal pathologies that may be of importance
The role of the otolaryngologist is to pick up other nasal pathologies that may be of importance
 Gross nasal septal deviation may hinder the intranasal access to the lacrimal sac, and the patient should be counselled for septal surgery together with the DCR
Gross nasal septal deviation may hinder the intranasal access to the lacrimal sac, and the patient should be counselled for septal surgery together with the DCR
35.6.2 Jones Dye Tests
 A drop of 2% fluorescein dye is placed in the inferior fornix
A drop of 2% fluorescein dye is placed in the inferior fornix
 Disappearance of the dye from the eyes is assessed after 10 to 15 min
Disappearance of the dye from the eyes is assessed after 10 to 15 min
 Retention of dye indicates blockage in the lacrimal drainage system
Retention of dye indicates blockage in the lacrimal drainage system
 Dye is instilled in patient’s eye, and a cotton bud is placed in the inferior meatus
Dye is instilled in patient’s eye, and a cotton bud is placed in the inferior meatus
 If dye is present after 5 min this indicates a patent system
If dye is present after 5 min this indicates a patent system
 Absence of dye indicates the anatomical obstruction between the punctum and valve of Hasner
Absence of dye indicates the anatomical obstruction between the punctum and valve of Hasner
 False-negative rate of up to 20%
False-negative rate of up to 20%
35.6.3 Regurgitation Test
35.6.4 Ophthalmology Tests
 Jones II dye test
Jones II dye test
 Lacrimal probing/irrigation
Lacrimal probing/irrigation
35.6.5 Dacryocystography
35.6.6 Dacryoscintigraphy
35.6.7 CT Scan
35.7 Current Management Strategies
35.7.1 Proximal Stenosis
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree