28 Core Messages • Oral mucositis (OM) is a major problem for patients with cancer receiving head and neck radiotherapy, stem cell transplantation, and myelosuppressive chemotherapy for solid tumors. • Poorly managed OM is one of the leading causes for unplanned treatment interruptions, which are responsible for increased cost and time in delivering optimal treatment to the patients with head and neck cancer. • Well-timed intervention and effective treatment is required to prevent or reduce the incidence and severity of mucositis. • The better understanding of its pathologic basis has led to the development of targeted agents to combat mucositis. • The Multinational Association of Supportive Care in Cancer and the International Society for Oral Oncology advocate guidelines for the prevention and treatment of mucositis. Significant advancements have been made in the management of patients undergoing cancer chemotherapy (CT) and radiotherapy (RT). However, many debilitating side effects, such as nausea, vomiting, diarrhea, and mucositis, remain critical issues that often delay or restrict the therapy and impede recovery. Mounting evidence indicates that more aggressive regimens improve locoregional tumor control and survival in patients with head and neck cancer (HNC). The better treatment outcome, however, has come at the expense of increased patient morbidity, notably, an increase in severe (grades 3 to 4) mucositis that causes substantial pain, interferes with the patient’s ability to chew and swallow, and worsens the patient’s quality of life. Virtually all patients with HNC develop some degree of mucositis during their treatment by either RT or CT. Nowadays; a majority of patients with HNC are being treated by concurrent chemoradiotherapy (CRT) as radical or adjuvant management, which in turn increases the probability of flaring up of mucosal inflammation. In general terms, mucositis is the inflammation of the mucous membrane lining of the digestive tract from the mouth on down to the anus. When it involves the mucous membrane of oral and oropharyngeal region, it is termed as oral mucositis (OM). It is due to systemic effects of chemotherapeutic agents and the local effects of radiation on the oral mucous membrane. Thus, OM, if not detected or treated adequately, can lead to pain, discomfort, and inability to tolerate food or fluids, with increased propensity for opportunistic infections in the mouth. Poorly managed OM is one of the leading causes for unplanned treatment interruptions1 and therefore increases the overall treatment time. Prolongation of overall treatment time adversely affects the tumor control probability.2 It also increases the overall cost of treatment. Trotti et al3 studied more than 6000 patients with squamous cell cancers of the head and neck who received RT with or without CT. The overall incidence of OM in this patient population was 80%, with 39% of the cases being grade 3/4 (Table 28.1), which limited or prevented alimentation. Patients who received altered fractionation RT (AF-RT) were particularly at risk; all patients in this subgroup experienced OM, with 57% scored as grade 3/4.3 A smaller, but still significant proportion (approximately 40%) of patients who receive standard-dose CT also develop OM as a result of therapy, with the lowest risk occurring by “gentler” chemotherapeutics, such as gemcitabine, and the higher risk occurring with more aggressive agents such as 5-fluorouracil (5-FU) and cisplatin. Higher OM incidence rates of 60% are seen in the stem cell transplantation setting, with reported incidence rates of up to 78% for ulcerative mucositis as a result of high-dose CT or total body irradiation. The severity of OM may be higher with allogeneic transplants than with autologous transplants.4 The potential for developing OM after RT or CT is influenced by a variety of patient- and treatment-related risk factors (Table 28.2).5 Table 28.1 Incidence of Oral Mucositis among Cancer Patients3
Mucositis
Incidence
Predictive Indices/Risk Factors
Incidence (%) | Grade 3/4 (%) | |
Radiotherapy for head and neck cancer | 85–100 | 25–45 |
Stem-cell transplantation | 75–100 | 25–60 |
Solid tumors with myelosuppression | 5–40 | 5–15 |
Adapted from reference 3.
Patient-Related Risks
Numerous patient-related factors appear to increase the frequency and severity of OM after CT or RT, including gender, age of the patient, type of malignancy, pretreatment oral condition, oral care during treatment, nutritional status, and pretreatment neutrophil counts (Table 28.2). Disagreement exists relating to the effects of age and the development of OM. Younger individuals (< 20 years) are more susceptible because of the more rapid epithelial mitotic rate or the presence of more epidermal growth factor receptors in the epithelium. On the contrary, decline in renal function associated with aging is the possible reason of increased incidence of OM in older patients. (> 65 years) Poor oral hygiene, chronic periodontal disease, smoking, alcoholism, and oropharyngeal infection may contribute significantly to the development of OM. Decrease in neutrophil count results in an impaired ability to mount an adequate inflammatory response, leading to increased probability of OM.
Treatment-Related Risks
Treatment-related factors consist of specific chemotherapeutic drug, dose, schedule, whether continuous or bolus, and use of radiation therapy.6 All these factors are summarized in Table 28.2.
Table 28.2 Risk Factors for Oral Mucositis
Patient-related • Gender • Age older than 65 y or younger than 20 y • Inadequate oral hygiene • Periodontal diseases • Chronic low-grade oral infections • Salivary gland secretory dysfunction • Herpes simplex virus infection • Inborn inability to metabolize chemotherapeutic agents effectively • Poor nutritional status • Exposure to oral stressors including alcohol and smoking • Ill-fitting dental prostheses |
Treatment-related • Radiation therapy: dose, schedule, and type such as conformal or intensity-modulated radiation therapy • Chemotherapy: agent, dose, and schedule • Myelosuppression • Neutropenia • Anemia • Immunosuppression • Reduced secretory immunoglobulin A • Insufficient oral care during treatment • Infections of bacterial, viral, and fungal origin • Use of drugs such as antidepressants, opiates, antihypertensive, antihistamines, diuretics, and sedatives • Deranged renal and/or hepatic function • Protein or calorie malnutrition • Dehydration |
Adapted from reference 5.
y, year.
Pathogenesis
The pathogenesis of cancer treatment–related OM is not fully elucidated. Recent advances in molecular cellular biology and translational research propose a complex multistep process taking place in the development of OM. Healthy oropharyngeal mucosa has a rapid cell turnover with a renewal period of 7 to 14 days, and it serves as a barrier to infections. Soon after CT or RT administration, acute inflammatory/vascular changes occur. Sonis7 has described a five-phase model to characterize the major steps in the development and resolution of OM:
1. Initiation: Reactive oxygen species generated by exposure to CT or RT result in DNA strand breaks and damage to cells, tissues, and blood vessels, which ultimately cause apoptosis.
2. Message generation: Such damage triggers the activation of transcription factors such as nuclear factor kappa B, which in turn causes increased production of proinflammatory cytokines such as interleukin (IL)-1β and IL-6. These increased levels of cytokines trigger the initiation of various pathways that damage epithelial cells and surrounding fibroblasts, causing tissue injury and apoptosis.
3. Signaling and amplification: Proinflammatory cytokines, such as tumor necrosis factor α (TNF-α), activate ceramide and caspase pathways; these signals further increase the production of TNF-α, IL-1β, and IL-6, thus causing an amplification effect.
4. Ulceration and inflammation: Inflammatory infiltrate composed of polymorphonuclear and round inflammatory cells is found in the mucosa. As there is a breach in the mucosal barrier, penetration of the epithelium into the submucosa can occur and the mucosa is prone to bacterial infections, which further lead to an increase in the production of TNF-α, IL-1β, and IL-6. This further enhances the mucosal injury, thus causing more severe OM in the form of ulceration, allowing colonization by oral bacteria and increasing the risk of sepsis. It is likely that in each of these OM stages, pathogenesis occurs in a continuous, overlapping manner.
5. Healing: Healing of oral lesions starts with a signal from the extracellular matrix in the nonmyelosuppressed patient within 2 to 3 weeks after cancer treatment. Mechanisms of healing include renewal of epithelial proliferation and differentiation in parallel with white blood cell recovery and reestablishment of normal local microbial flora.
Pathogenesis of OM has suggested a variety of potential therapeutic targets, which have resulted in the development of agents that can prevent or ameliorate associated symptoms. Several such compounds are thought to inhibit one or more steps in these pathways, thus enhancing their effectiveness. Because some agents act to downregulate nuclear factor kappa B activation, which is involved in upregulating numerous genes encoding proinflammatory cytokines, the resulting inhibition may be greatly enhanced.
Diagnosis
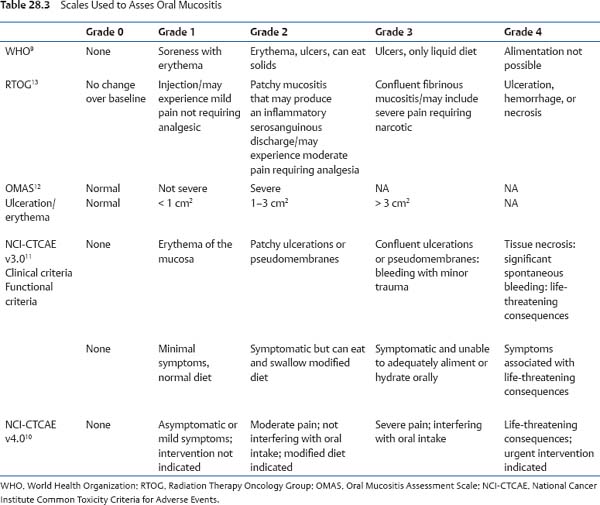
OM is typically diagnosed on the basis of the clinical appearance, location, timing of oral lesions, and use of certain types of therapies known to be associated with OM. Consistent and frequent oral cavity assessment under intense white light is needed to visualize all soft and hard tissues and dentition before, during, and after the treatment time course. Systematic assessment of the oral cavity permits early identification of the lesion. All assessors should have a thorough familiarity regarding clinical signs and symptoms of oral complications. Systemic effects of OM may result in the symptom complex, characterized by fatigue, taste alterations, anemia, anorexia, cachexia, neurocognitive alterations, and depression, which may often be termed as “sickness syndrome.”8 Mucosal damage by CT or RT results in the release of inflammatory mediators and the activation of biologic processes, which result in systemic effects. Several scoring systems have been defined to assess the severity of OM (Table 28.3), but no one scale is uniformly used. These evaluative tools vary in complexity. Some established guidelines are those proposed by the World Health Organization9 and the National Cancer Institute’s Common Toxicity Criteria.10,11 In the World Health Organization scale, both objective mucosal changes (redness, ulceration) and functional outcomes (ability to eat) have been integrated. In contrast, National Cancer Institute’s Common Toxicity Criteria have been developed to classify OM in patients receiving radiation therapy, CT, and conditioning regimens for bone marrow transplantation.10,11 On clinical examination, four distinct stages/grades can be identified (Fig. 28.1). Patients are able to maintain oral intake in grade 1, oral intake is compromised in grade 2, patients are unable to take anything (food or liquids) in grade 3, and grade 4 is life-threatening.
In addition, Sonis et al12 have devised an Oral Mucositis Assessment Scale. This scale separates objective and subjective findings. Degrees of ulceration and redness measured in specific sites in the mouth were primary indicators of OM, while oral pain, difficulty in swallowing, and the ability to eat were taken as secondary indicators. A single score is not produced from this scale, rather a score for ulceration and redness based on different locations in the mouth are used. This scale is more quantitative for clinical research but may be difficult to use in routine clinical care.
Other scoring systems by Radiation Therapy Oncology Group have been proposed,13 but the lack of standardization has hampered their acceptance.
Other common conditions that may confuse OM include oral candidiasis (thrush), herpes simplex virus (HSV), and graft-versus-host disease (GVHD) in patients with transplant. Candidal overgrowth (candidiasis), which occurs in response to RT or CT, usually responds well to systemic antifungal medication. HSV is frequently seen in patients with immunocompromised cancer receiving CT, with lesions appearing on the lips (cold sores) or intraoral mucosa. Initiation of antiviral therapy may ameliorate HSV-associated OM and reduce symptoms. OM can also occur in patients receiving myeloablative conditioning regimens for allogeneic hematopoietic stem cell transplantation and in those with GVHD, affecting the oral mucosa. Consequently, an accurate diagnosis of OM is critical to ensure selection and timely initiation of optimal therapy.
Management Guidelines
A standardized approach for the prevention and treatment of CT- and RT-induced OM is essential. Numerous agents and protocols have been developed for the management or prevention of OM, but the most widely accepted guidelines were issued in 200414 and were updated by the Multinational Association of Supportive Care in Cancer and International Society for Oral Oncology (MASCC/ISOO).15 These guidelines are based on a comprehensive review of more than 8000 English-language publications (1966 to 2001). Discussions by the panel resulted in the development of a set of recommendations for the prevention and treatment of OM. Guidelines that are relevant to the care of patients with HNC are discussed here (Table 28.4). The MASCC/ISOO Mucositis Study Group has continued to monitor the literature and in 2007 updated OM management guidelines.16
These guidelines emphasize multiprofessional interventions for appropriate management of OM. An interdisciplinary approach to oral care, routine assessment of oral cavity, pain management using validated instruments, and regular dental assessment and dental care before the start of cancer therapy is the foundation of care. The panel stressed the need for education of staff as well as patients and their families on proper oral care and the importance of outcome assessment using quality-improvement processes.
Treatment Options
Although several approaches to OM management have been advocated, a single efficacious intervention or agent for the prophylaxis or management of RT- or CT-induced OM has not yet been identified. Many different treatments are used to prevent or treat OM, and these interventions have been categorized under the following headings, though in the absence of double-blind and placebo-controlled clinical trials, many of the management recommendations are only subjective.
Basic Oral Care
Poor oral hygiene along with associated dental and periodontal pathology, such as dental caries, ill-fitting prostheses, and orthodontic appliances leads to a greater risk for OM in the course of RT or CT. The MASCC/ISOO recommends “basic oral care” as a standard practice to prevent and alleviate mucosal symptoms.16 The “basic oral care” typically includes careful inspection of the oral cavity, evaluation by dental specialists, and dental work to eliminate caries and existing gum disease before beginning cancer treatment and should be repeated in the course of treatment.15 Such practice not only helps in the differentiation of OM from preexisting changes, such as pemphigoid, lichen planus, leukoplakia, and GVHD, but also permits the identification and elimination of preexisting potential sources of infection that may affect the severity of the OM.
< div class='tao-gold-member'>