23 Microscopic and Endoscopic Transsphenoidal Pituitary Surgery: A Reasoned and Balanced Dialectic
The transnasal or endonasal transsphenoidal approach to the sella, developed in the early 20th century, was a remarkably elegant solution to the problems that early surgeons faced with intracranial access to the pituitary gland.1–12 This approach has evolved over the last century, resulting in the application of radiofluoroscopy,13 the operative binocular microscope14 (by which most pituitary surgery is performed today), ultrasound, magnetic resonance imaging (MRI)-based image guidance, and intraoperative MRI. More recently pituitary neurosurgeons have rediscovered the endoscope, deploying it in endoscopic-assisted and endoscopic-based transsphenoidal operations to refine illumination and visualization of the sella and parasellar regions during pituitary procedures.15,16 Endoscopic surgery of the pituitary was an extension of the use of endoscopy for sinus disease. As experience with endoscopic sinus surgery increased, endoscopic endonasal techniques were adapted and expanded for use in other conditions affecting the paranasal sinuses and skull base. Initially this was directed toward nonneoplastic conditions. Endoscopic treatment of cerebrospinal fluid (CSF) leaks was reported in the early 1980s, and then endoscopic repairs of encephaloceles and mucoceles were reported.17–19 Pituitary tumors were soon managed by endoscopic removal, and there followed debate as to the relative merits and demerits of each instrument—microscope or endoscope. Evangelism and proselytism now compete with cautious clinicians and careful analysis. Opinion and bias now rival balanced consensus and equanimity.
The arguments are by now familiar: “minimally invasive” (yet both are endonasal—endonasal microscopic or endonasal endoscopic); shorter length of stay (length of stay has nothing to do with a microscope or an endoscope); nasal packing (packing has nothing to do with a microscope or an endoscope); the view is three-dimensional (3D) and stereoscopic versus two-dimensional (2D) and somewhat distorted (yes, but 3D endoscopes are now being developed); panoramic visibility and ability to see around corners (yes, but this provides little added advantage in cases where the lesion is small and straight ahead at 0 degrees). Both hands are free to handle instruments (yes, bimanual surgery is safer and more effective, but get an endoscope driver or holder and you can free up the neurosurgeon to use both hands); enhanced illumination at the source versus loss of illumination with depth (fine, just as long as the lens is clean and free of blood); enhanced resection (yes, if it is safe without added complications, and the enhancement results in 100% removal and disease remission or cure; otherwise little additional benefit has been achieved if adjuvant therapy is still needed); operating times are shorter or longer (that depends on whom one reads and his or her veracity). The litany of claims and counterclaims goes on and on as protagonists are swept up in the tide and emotion.
A careful consideration of the advantages and disadvantages of both techniques allows the rational surgeon to individualize the approach to each patient’s lesion. Not every patient is best served by the exclusive use of either a microscopic or an endoscopic approach. In fact, in certain situations, a combination of microscopic and endoscopic techniques may provide the best combination of safety and efficacy. Surgeons need to be comfortable with all the available technology to address a patient’s pathology, or they may fall into the trap of seeing everything as a nail when all they have is a hammer. Conversely, any tool in the hands of surgeons must be carefully deployed; “a fool with a tool is still a fool, only a more dangerous fool.”
No instrument or equipment can make one a surgeon. Surgeons achieve expertise by years of training and the acquisition of experience. Good judgment comes from experience, whereas experience comes from bad judgment (Jim Horning). The critical question facing pituitary neurosurgeons today becomes when and how to deploy endoscopic and microscopic techniques, based on available data and experience. In this chapter, we present clinical decision-making factors that should guide the discerning and discriminating neurosurgeon as to whether microscopy-based, endoscopy-based, or a hybrid of the two techniques represents the optimal procedure for successfully resolving pituitary lesions.
 A Comparison of Microscopic Versus Endoscopic Transsphenoidal Methods
A Comparison of Microscopic Versus Endoscopic Transsphenoidal Methods
The state of the literature surrounding this debate is at present polarized between traditional microscopists and evangelical endoscopists, both arguing in favor of their procedural biases. To be sure, there is a middle ground. Most descriptions of these techniques occur with little attempt to appreciate their common features, which are many.
Planning and Positioning
The differential diagnosis of pathologies that may occupy the sella turcica includes tumors and nonneoplasms and is extensive.20 Even the most common lesion, pituitary adenomas, frequently have parasellar extensions (Fig. 23.1). Thus, the strategy of how microscopic and endoscopic techniques are applied must begin at the planning stage, which should be given considerable thought.
Assistant surgeons, most commonly otorhinolaryngologists, may be included if an endoscopic approach is under consideration. This multidisciplinary approach, although still institution-dependent, is a very common and reasonable practice, especially when planning for complex lesions. In this scenario, the operating room should be accommodated to facilitate both teams. If a pure microscopic approach is planned, the use of fluoroscopy or MRI/computed tomography image guidance, depending on the neurosurgeon’s preference, may be included at the beginning of the procedure without requirements for an endoscopic setup. If fluoroscopy is anticipated, care should be taken to make sure the head pin position does not obstruct the sella and sphenoid on a lateral view. With both procedures, induction of general anesthesia and placement of a lumbar drain (if needed) are identical. Positioning of the head should be fixed approximately 10 degrees toward the surgeon. For sellar lesions, the head is generally flexed approximately 20 degrees and even more so if the disease is clival in origin. The head should be extended if the lesion is suprasellar. That being said, some surgeons do not use a Mayfield head holder in endoscopic approaches. If an endoscope will be used, typically the endoscope monitor is positioned behind the patient; the surgeon stands on the right, the assistant stands on the left, and anesthesia is situated on the side opposite the surgeon behind the assistant. If a microscope will be used, this is an appropriate time to balance and drape it. Also, intraoperative guidance systems, if any, should be readied. Next, the nasal mucosa is prepared with a vasoconstrictive agent, for example, 4% cocaine or oxymetazoline. In the endonasal transseptal microscopic-based procedure, the nasal mucosa may be injected with local anesthetic to aid in the dissection of the rhinoseptal mucosa. In the direct endonasal microscopic approach there is no septal mucosal dissection.21
Approach and Exposure
In practical terms, the ergonomics of the operation are dependent on the hardware used, whether a microscope or endoscopic instrumentation. When the microscope is used, the entire procedure is usually performed independently by a neurosurgeon, with the assistant observing through the observer scope. An array of nasosphenoidal routes exist, including sublabial-paraseptal, endonasalunilateral-septal,22 and direct endonasal.21,23 The sublabial route is presently the least used. If a septal mucosal dissection is done, it is usually necessary to insert a nasal speculum to hold the nasal mucosa out of the line of sight and to push the middle turbinate laterally. If a direct endonasal approach is performed, there is no septal dissection and the nasal speculum is inserted into the nostril and opened at the face of the sphenoid between the ostium and the septum, subluxing the septum and exposing the face of the sphenoid.21 The operation usually takes place through the nostril containing the nasal speculum. As mentioned, in endoscopic-based procedures, the procedure is typically multidisciplinary, with the otolaryngologist completing the endoscopic endonasal approach to the sphenoid sinus and the neurosurgeon opening the sella and resecting the tumor. However, many neurosurgeons perform the approach without an otolaryngologist. A unilateral or bilateral nostril approach may be used, and the assistant usually drives the camera. The use of a speculum is not necessary, as there is no need for mucosal retraction and no “line-of-sight” vision requirements. Moreover, a speculum would limit the space available for the endoscope and surgical instruments. However, because no speculum is present, the endoscope and instruments can abrade the mucosa and cause bleeding that can obstruct the endoscope lens. Because of this, and due to the proximity of the lens to the operative field, during endoscopic-based procedures frequent and repeated cleansing of the endoscope is often required. In contrast, the microscope, at a fixed distance away from the field, does not usually get soiled with blood and does not require frequent cleaning, if at all.
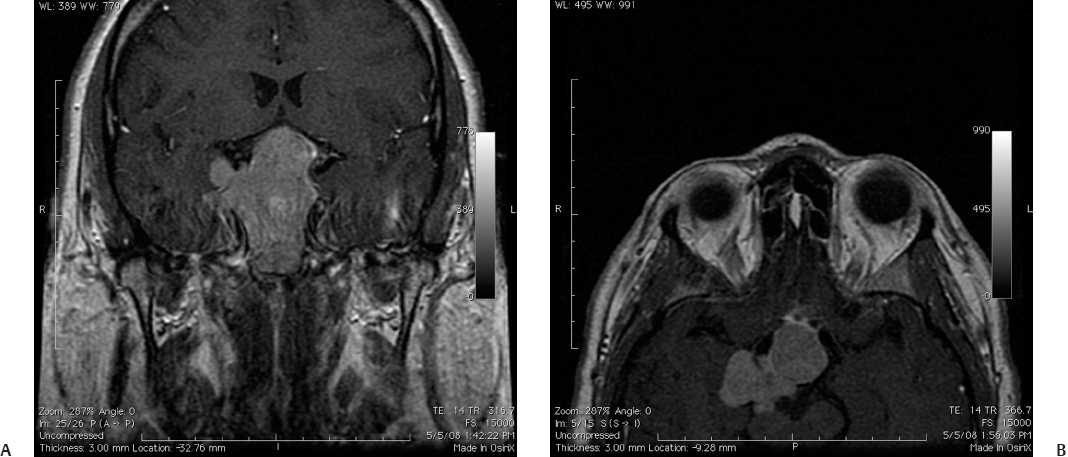
Fig. 23.1 (A,B) A pituitary lesion with asymmetric parasellar extension suitable for hybrid or pure endoscopic resection, permitting the surgeon to look “around the corner.”
As the endoscopic procedure commences, the camera and instruments are introduced parallel to one another through one or both nostrils. It is important not to lose sight of the instruments in front of the endoscope to prevent trauma to the mucosa or important neurovascular structures. The surgeon is offered a wide viewing angle with the endoscope that provides a panoramic view of the sphenoid sinus, the face of the pituitary gland, and the interior of the tumor cavity in trajectories unavailable to the microscope. In a combined approach, the bulk of the tumor is resected using the microscope, and the endoscope then provides illumination and magnification of regions of interest outside the view of the microscope, including the cavernous, suprasellar, anterosellar, parasellar (Fig. 23.1), and retrosellar regions. In a study of cadaver sellae, Spencer et al24 quantified the volume of space accessible under both microscopic and endoscopic guidance. In this study, a significantly greater volume of 3D space was visualized using the endoscope versus the microscope in both the endonasal-transsphenoidal (225 mm3 versus 75 mm3, p <.0001) and sublabial-transsphenoidal (350 mm3 versus 200 mm3, p <.0001) approaches.
Apart from differences in optical properties, another difference between the procedures is in the exposure of the nasal passage and sphenoid sinus. In the microscope-based transseptal (but not the direct endonasal procedure), a small vertical buried incision is made within the nasal mucosa in either nare but usually ipsilateral to the operating surgeon. A complete dissection of the rhinoseptal mucosa from the nasal septum is performed following the initial incision. A handheld nasal speculum is inserted medial to the septum and lateral to the rhinoseptal mucosa, taking care not to tear the mucosa. Any remaining attachment of mucosa to the septum is freed at this time. The perpendicular plate of the ethmoid and the vomer between the surgeon and the sella are removed. The nasal speculum is then arranged in the newly formed submucosal cavity with the tips of the blades nearly at the base of the sphenoid sinus. Once the speculum is in good position, the blades are gently opened to keep the mucosa out of the operative field.
The endoscopic procedure and the direct endonasal microscopic procedure both obviate an initial nasal mucosal incision.21 However, in the endoscopic approach, in lieu of the nasal mucosal incision, a large bilateral sphenoidectomy and posterior one-third septectomy are created to provide for entry of the instruments and the endoscope into the sphenoid sinus. This opening is invasive and indeed quite so in that the mucosa and bone over the sphenoid sinus wall are extensively debrided and approximately one third of the posterior septum is removed (fortunately this is not externally visible).
In contrast to the microscopic approach, with the endoscopic approach, one of the nuances that must be mastered is driving the camera. Upon entry of the endoscope into the nare, the camera is oriented with the following important landmarks identified: (1) the inferior turbinate and eustachian tube in the lateral field, (2) the nasal septum in the medial field, (3) the nasal cavity floor in the inferior field, and (4) the middle turbinate head in the superior field. It may sometimes be necessary to decongest and perhaps laterally dislocate the middle turbinate head, which usually closely approximates the nasal septum.
Next, in both the microscopic and endoscopic procedures, the sphenoid ostia are identified. These are normally located approximately 1.5 cm above the roof of the choana and are of variable shape and size. The ostia initially may not be visible, as the view can be obstructed by the superior turbinate. Again, it may be necessary to lateralize or partially remove this structure. The surgeon should note, however, that the lateral lamella of the cribriform plate is thin, which poses a risk of ethmoid CSF leak. Starting 0.5 cm from the top of the choana while taking care to avoid the sphenopalatine artery branches, the sphenoethmoid recess and sphenoid ostia are carefully coagulated. At this point, the nasal septum may be detached from the sphenoid rostrum and the bone of the vomer between the ostia can be removed. In both procedures, the sphenoid ostia are opened using a bone punch or microdrill. Once the sphenoid sinus is opened, the midline is identified. Surgeons should note the location of the septum in relation to the midline on preoperative imaging as the midline can be markedly asymmetric.25 Next, the mucosa over the face of the sella is removed or cauterized and the sella itself is opened.
Optical Properties
Once in the sphenoid sinus and the sella, the differences in optical properties between the microscope and endoscope are best appreciated. However, it is imperative to note that these differences are not mutually exclusive but complementary. Within the sphenoid sinus, the endoscope allows direct visualization of the carotid and optic nerve prominences before proceeding with opening the sella turcica. The microscope, conversely, does not offer this ability to look “around the corner” and panoramically inspect the sella widely to identify these landmarks. However, this is neither necessary nor essential if the operation is for retrieval of a small or wholly intrasellar lesion. The microscope, however, does offer depth perception, which the endoscope lacks. Currently, endoscopes provide only 2D (monocular) images that by definition lack depth, and thus restrict the surgeon’s perspective, which can limit the ability to perform critical aspects of some surgeries. To be sure, part of this limitation can be obviated by movement of the endoscope to allow perception of relative positional anatomy. Stereoscopic vision better facilitates understanding of the anatomy, hand–eye coordination, and the use of surgical instruments. Technological refinements from industry (Visionsense, Orangeburg, NY) have led to the development of proprietary miniature sensors that offer natural stereoscopic vision. The technology is based on a single stereoscopic (3D) sensor that imitates an insect’s compound eye26 and offers the ability to surpass the 2D limitation of the endoscope. However, the market penetration and adaptation of this technology are in their infancy, and the ultimate impact it will have on pituitary surgery remains to be seen. Thus, at present, the optical properties of the endoscope present a learning curve for neurosurgeons trained solely using microscopic techniques, a deficiency that can be overcome with preoperative practice in the anatomy laboratory, practical courses, and increasing exposure and experience.25 Furthermore, with the current rediscovery of the endoscope, more neurosurgeons are gaining familiarity with use of the endoscope, particularly in centers with endoscopic surgeons, those with multidisciplinary teams of otolaryngologists and neurosurgeons, and those with neurosurgery faculty trained in both techniques. As a result, increasing numbers of neurosurgeons in training and neurosurgeons recently out of training have gained exposure to endoscopic techniques. This trend is overall positive and likely will facilitate the appropriate and judicious use of one or both techniques dictated by the anatomy of each patient’s tumor rather than by the surgeon’s comfort with one particular technology over the other.
Tumor Removal
Using bayoneted instruments in the microscopic approach, the tumor is resected from normal pituitary glandular tissue under direct visualization.23 Bayoneted instruments may be used in the endoscopic approach as well but are not usually necessary, and straight shafts are preferable.25
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


