Chapter 46 Management of Recurrent Laryngeal Nerve Paralysis
![]() This chapter contains additional online-only content, available onexpertconsult.com.
This chapter contains additional online-only content, available onexpertconsult.com.
Introduction
Recurrent laryngeal nerve (RLN) injury is a dreaded complication following thyroid surgery. Injury to the nerve can result in vocal fold immobility or hypomobility. We tend to avoid using the term paralysis in situations of vocal fold immobility. Paralysis refers to the permanent loss of voluntary movement in a muscle through injury to or disease of its nerve supply. Following injury to the RLN, recovery of individual muscle movement frequently does occur, but in a disorganized fashion resulting in synkinesis—uncoordinated, simultaneous activation of opposing muscle groups. Furthermore, vocal fold immobility can be the result of mechanical fixation of the cricoarytenoid joint (see Chapter 45, Pathophysiology of Recurrent Laryngeal Nerve Injury). However, dysphonia, dysphagia, or dyspnea presenting in the acute setting after thyroidectomy is presumed to be secondary to an RLN injury until proved otherwise. The incidence of RLN injury during thyroid surgery has been reported in the range of 0.3% to 15.4% nerves at risk.1 Management of laryngeal dysfunction after thyroid surgery involves identifying the etiology and nature of the functional deficit, determining prognosis, and developing a treatment plan to address voice and swallowing issues.
Unilateral Vocal Fold Immobility
Evaluation
History and Physical
Dysphonia following thyroid surgery is not an uncommon finding. In fact, 42% of patients in one study had impairment of vocal function postoperatively, although 31% of the subjects had direct injuries to the vocal folds, presumably from endotracheal intubation.2 It is important, therefore, to distinguish the cause of postoperative dysphonia. Equally important is the need to perform careful preoperative videolaryngoscopy so that preexisting laryngeal dysfunction can be differentiated from new findings (see Chapter 15, Pre- and Postoperative Laryngeal Exam in Thyroid and Parathyroid Surgery). Unilateral vocal fold immobility after surgery can present with a variety of symptoms resulting from injury to the RLN, superior laryngeal nerve (SLN), or both. Typically a patient with complete immobility presents with a breathy, weak voice and may have symptoms of dysphagia, in particular aspiration of liquids. Unilateral partial RLN injury is manifest as hypomobility of the vocal fold with resultant dysphonia, vocal fatigue, diplophonia, and odynophonia.3
Often, unilateral RLN injury may not be evident within the first few days (or even weeks) after surgery because of acute vocal fold edema from intubation. The increased bulk of the vocal fold compensates for the inability of the arytenoid to fully adduct. Hoarseness that persists longer than a few days must increase suspicion of RLN injury. Despite the obvious possibilities of surgical injury to the RLN and intubation injury, inquiries regarding other sources for dysphonia should also be made while conducting the history and physical exam, especially following a longer interval after surgery. These sources include infection (viral, Lyme disease), neurologic causes (cerebrovascular accident, myasthenia gravis, multiple sclerosis), neoplasm (skull base, mediastinal or pulmonary lesions), trauma, toxins, or systemic diseases (sarcoidosis, diabetes mellitus, collagen-vascular disease). Subjective evaluation of the voice should also be performed throughout the entire examination. Many clinicians will employ a standardized voice assessment protocol such as the GRBAS scale (grade, roughness, breathiness, asthenia, strain) or CAPE-V (consensus auditory perceptual evaluation of voice) to rate the quality of the voice.4 Patient-based voice surveys such as the Voice Handicap Index-10 (VHI-10) or Voice-Related Quality of Life (V-RQOL) can also be utilized to document the extent of vocal dysfunction.5,6 These instruments are useful for establishing a baseline from which future improvement or deterioration can be measured.
![]() Please see the Expert Consult website for more discussion of this topic.
Please see the Expert Consult website for more discussion of this topic.
Videolaryngoscopy
An essential component of the examination for dysphonia is inspection of the larynx via either flexible or rigid video laryngoscopy, or both (see Chapter 15, Pre- and Postoperative Laryngeal Exam in Thyroid and Parathyroid Surgery). Flexible videonasolaryngoscopy with a distal tip color charge-coupled device (CCD) chip camera allows for observation of the larynx in a physiologic position, as well as acquisition of magnified, high-resolution images of the laryngeal mucosa. Addition of stroboscopy gives further insight into vocal fold vibratory function, vocal fold muscle tone, height discrepancies of the vocal processes of the arytenoids, and glottic closure. Rigid videostroboscopy provides superior image quality to traditional fiberoptic laryngoscopes and distal chip scopes and, in particular, improved visualization of the posterior glottis. It also maintains the alignment of the vocal folds in relation to the endoscope, which lessens the chance of skewing the video image. The disadvantage of rigid endoscopy is the need for tongue protrusion, which places the larynx into a nonphysiologic position during phonation and can make phonatory tasks more difficult.7Newer high-definition (HD) flexible nasolaryngoscopes may combine the benefits of both flexible and rigid endoscopy.
![]() Please see the Expert Consult website for more discussion of this topic.
Please see the Expert Consult website for more discussion of this topic.
During the endoscopic exam, the larynx should be observed for any gross asymmetries in configuration or movement. Sometimes it is necessary to view the video replay in slow motion or frame by frame to pinpoint these irregularities. The patient is asked to perform a series of repetitive phonatory tasks in an attempt to induce vocal fatigue and elicit evidence of subtle paresis. Rubin et al. describe the use of various tasks for this purpose including alternating a sniff with the /i/ vowel repeatedly.8 The SLN is tested by having the patient perform a glissando maneuver—sliding from the lowest note to the highest note and back down. A paresis of the SLN may manifest as a rotation of the posterior larynx toward the side of the injury (see Chapter 32, Surgical Anatomy of the Superior Laryngeal Nerve). Supraglottic hyperfunction with compression of the false vocal folds can obscure proper evaluation of the glottic structures but may also be a harbinger of compensation for an underlying glottic insufficiency as noted by Belafsky.9 The possibility of an arytenoid subluxation or cricoarytenoid fixation should be entertained in addition to neurologic deficits. Subluxation of the arytenoid can occur from trauma during intubation and will result in pain upon swallowing or speaking. No pain is encountered in cricoarytenoid fixation.
Stroboscopic evaluation can reveal several different findings that support the diagnosis of paresis. An anterior glottal gap may be seen, sometimes in conjunction with a posterior gap. Even without a glottal gap, open phase dominance of the glottic cycle—defined as greater than 70% of the time spent in open phase—can be a sign of paresis. Irregular vibratory motion of one vocal fold can be the result of asymmetrical tension of the vocal folds. This manifests as one vocal fold tracking with the strobe while the other vibrates asynchronously. Phase asymmetry with a snake dance, side-to-side movement of the vocal folds has also been described as a finding in paresis.8
Fiberoptic endoscopic evaluation of swallowing (FEES) can be performed on a patient with complaints of dysphagia at the same setting as videolaryngoscopy or as a separate evaluation by a speech-language pathologist. A FEES examination includes a survey of anatomic structures at rest and in motion during the act of swallowing. With a flexible nasolaryngoscope positioned between the nasopharynx and midpharynx, observations are made noting pooling of secretions and penetration (entry of liquid or food into the larynx) or aspiration (passage of liquid or food beyond the vocal folds) of various consistencies of liquids or foods. Therapeutic interventions can be initiated at the time of the swallowing study if abnormalities are found.10 Aviv and colleagues added sensory testing as part of the endoscopic swallowing exam (FEESST) using calibrated pulses of air to elicit the laryngeal adductor reflex.11 Tabaee et al. showed significantly higher rates of dysphagia in patients with decreased pharyngeal squeeze, decreased laryngopharyngeal sensation, and an absent laryngeal adductor reflex.12 Although supraglottic sensory deficits would not be expected following an isolated RLN injury, a preexisting sensory deficit could make a patient more susceptible to aspiration. Detection of a sensory deficit by FEESST may increase consideration of a concomitant hypopharyngoplasty, a procedure to reduce pyriform sinus dead space, at the time of medialization surgery.
Laryngeal Electromyography
Laryngeal electromyography (LEMG) evaluates the electrical activity of the muscles within the larynx (see Chapter 33, Surgical Anatomy and Monitoring of the Recurrent Laryngeal Nerve). It is a useful adjunct to videolaryngoscopy and stroboscopy in identifying vocal fold paresis, distinguishing between neurologic causes for immobility and mechanical causes, and attempting to prognosticate return of function from a nerve injury. Despite the benefits of LEMG, evidence-based reviews have yet to fully recommend its use in diagnosis of vocal fold paresis.13
A thorough discussion of the physiology of LEMG is beyond the scope of this chapter and is covered comprehensively by authors elsewhere.13–15 Briefly, following injury to an axon, no electrical impulses are transmitted distal to the site of injury. Therefore, immediately following injury there is no activity of the affected motor fibers observed on LEMG following injury. Approximately 3 weeks after denervation, muscle cells will begin to spontaneously fire as the resting potentials fall near the depolarization threshold. These events are seen as fibrillation potentials on LEMG. As reinnervation occurs, nerve fibers grow into atrophied muscle fibers in a disorganized fashion resulting in muscle weakness and lack of synchrony. The reinnervation pattern is reflected as polyphasic muscle unit action potentials (MUAPs) with prolonged duration and enlarged amplitude. The process of reinnervation does not guarantee a nerve will grow back to its appropriate muscle fiber. Aberrant reinnervation with adductor nerve fibers synapsing onto abductor muscle units and vice versa results in synkinesis. Although this nonphysiologic innervation may restore muscle bulk and tone, the vocal fold may not be able to move in a useful manner. The presence of synkinesis makes the use of LEMG to predict the return of normal vocal fold movement less accurate because electrical activity does not equate to purposeful movement; however, it is useful when there is no visible motion of the vocal fold. Sulica summarized the positive prognostic factors for recovery of movement from several studies as preservation of normal MUAP waveforms, activation of these during an appropriate voluntary task, preservation of a brisk degree of recruitment, absence of electrical silence or spontaneous activity, absence of aberrant MUAP morphology, and absence of patterns of activation during inappropriate tasks.14
![]() Please see the Expert Consult website for more discussion of this topic.
Please see the Expert Consult website for more discussion of this topic.
The question of when to perform LEMG is based on clinical judgment for each case scenario. In a patient who has clearly suffered a transection of the RLN during surgery or has tumor involvement with the nerve, the prognosis for spontaneous recovery is so poor that LEMG is unnecessary. Such patients can be offered definitive surgery to improve glottal closure without fear of interfering with spontaneous nerve recovery. However, in a case where the prognosis for recovery is in doubt, LEMG can help guide patient decisions on treatment. Min et al. concluded that LEMG results are most valuable if obtained within 6 months of injury and preferably within 6 weeks of onset of symptoms.16 They determined an 89% correct prognosis rate in their study of 14 patients with unilateral vocal fold immobility using LEMG. On the other hand, a larger study of 31 patients by Munin et al. determined that LEMG predicted only 44.4% of outcomes after nerve injury.17 Furthermore, they found LEMG to be better in predicting a positive test result with a fair or poor prognosis (persistent vocal fold immobility = 80%) than in predicting a negative result with an excellent prognosis (resolved motion = 66.7%). This would suggest that early findings on LEMG of poor prognosis for spontaneous recovery can help guide a patient in the choice for early surgical intervention. Further research is required to clarify the role and capabilities of LEMG in the management of laryngeal paralysis.
Direct Laryngoscopy
The role of direct laryngoscopy in the management of vocal fold immobility following thyroid surgery is extremely limited. Careful evaluation of the vocal process of the arytenoid cartilage during phonatory tasks using slow-motion videostrobolaryngoscopy with a distal-chip camera or rigid endoscope can often discriminate between a neural insult or mechanical cause of immobility caused by arytenoid subluxation, soft tissue scarring, or joint ankylosis. If the question remains after awake endoscopy, it can usually be answered with LEMG, saving the patient the inherent risks of general anesthesia and rigid laryngoscopy. In the face of normal LEMG findings, direct laryngoscopy can be performed to allow palpation of the arytenoid, exploration for scarring, and possible closed reduction of an arytenoid subluxation.18
Swallowing Therapy
Once aspiration is identified by history, a speech pathologist familiar with swallowing therapy techniques should initiate MBS or FEES/FEESST therapy (see the preceding discussion). Either MBS or FEES/FEESST can be used to define which consistencies of liquid and food are safe for swallowing. A swallowing therapist can also try different swallowing techniques while performing these exams to determine which techniques will be effective. These include postural techniques such as chin tuck and head turn, heightening preswallow sensory input, voluntary swallow maneuvers (e.g., supraglottic swallow), and swallowing exercises.19 In the case of persistent aspiration despite diet changes and the implementation of swallowing techniques, early vocal fold medialization procedures can be considered as described later. Medialization does not necessarily eliminate aspiration, but it can help the patient generate a stronger cough to protect the airway.
Voice Therapy
A team approach between an otolaryngologist and speech language pathologist for the management of a patient with vocal fold immobility is recommended. After the initial workup and diagnosis by the otolaryngologist, the patient is referred to a speech pathologist for objective voice analysis, assessment, and voice therapy. It is important to document the degree of vocal dysfunction prior to further intervention in order to objectively evaluate progress of the voice. Often patients with mild to moderate dysfunction will respond adequately to voice therapy without the need for surgical intervention. Heuer et al. studied 41 patients with RLN lesions (19 female and 22 male) and found that 68% of females and 64% of males did not elect to have surgery after adequate voice therapy.20 Furthermore, patient satisfaction was similar for both the surgical and nonsurgical groups. It should be noted that there was a tendency for patients with greater severity of glottal incompetence to elect for surgery rather than therapy. In patients who eventually elect for surgical intervention, preoperative voice therapy can help with surgical decision making, provide training for optimal postoperative phonation, and allow the patient to exhaust nonsurgical options prior to surgery. Voice therapy aims to improve glottal closure while eliminating undesirable compensatory hyperfunctional behaviors such as anterior-posterior or lateral supraglottic compression. However, in some cases patients may need ventricular compression to achieve voice, in which case beneficial hyperfunction may be taught. A variety of therapeutic techniques are used to develop abdominal support for breathing and improve intrinsic laryngeal muscle strength and agility. Description of these techniques is beyond the scope of this chapter but can be found in a comprehensive review by Miller.21 Surgeons should also bear in mind the importance of postoperative voice therapy to help patients adapt to a newly altered vocal system without developing unwanted vocal habits.
Surgical Treatment
Injection Laryngoplasty
Wilhelm Brünings initially introduced injection laryngoplasty in 1911 to correct the problem of glottic insufficiency resulting from unilateral vocal fold immobility.22 In this procedure a material is injected into the true vocal fold in an attempt to add bulk and medialize the edge of the vocal fold. Over the years, the procedure did suffer some setbacks because of complications from injectable materials such as paraffin and polytetrafluoroethylene paste (Teflon).23,24 Two significant gains in recent years have greatly advanced our ability to carry out injection laryngoplasty. The first is the development of distal chip camera technology that makes transnasal flexible visualization rival the view available in the operating room. This enables better accuracy of percutaneous injections for the larynx. The second advance is the variety of materials available for injection. There has been a proliferation of different materials available for vocal fold augmentation, spurred on in large part by the demand for injectable fillers in the cosmetic industry. These products have better biocompatibility, producing less inflammation and scar than previous injectables. They also obviate the need for harvest and preparation of autologous materials. These developments have expanded the range of indications, which currently include vocal fold atrophy, hypomobility, immobility, and scar.25
![]() Please see the Expert Consult website for more discussion of this topic.
Please see the Expert Consult website for more discussion of this topic.
Several methods for performing injection laryngoplasty have been described and can be used interchangeably based on surgeon preference or patient tolerance. Although Brünings performed his injections transorally with the patient awake, transoral injections under general anesthesia with suspension microlaryngoscopy were favored through much of the previous century because of the precision required by the unforgiving nature of Teflon. As other injectable materials have been introduced and visualization of the larynx has improved with distal chip flexible laryngoscopes, an increasing number of awake injections are being performed. A recent multicenter study by Sulica et al. reported that 51% of injections were performed in the awake setting using a combination of local and topical anesthesia.25
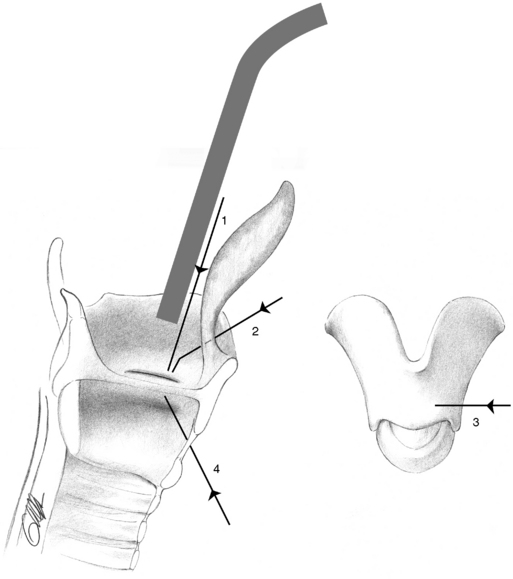
Four main approaches are used for awake injections: (1) transorally using a long, curved injection needle guided by either rigid endoscopy or flexible nasolaryngoscopy (Figure 46-1, line 1), (2) percutaneous transthyrohyoid injection with either a straight or bent needle inserted at the thyroid notch and entering the lumen of the airway at the petiole of the epiglottis (Figure 46-1, line 2), (3) percutaneous transthyroid cartilage injection with needle insertion through the ala of the thyroid cartilage at the approximate level of the vocal fold (Figure 46-1, line 3), and (4) percutaneous transcricothyroid injection where the needle is inserted below the inferior margin of the thyroid cartilage and angled superolaterally into the vocal fold (Figure 46-1, line 4). All of the percutaneous techniques are performed with visual guidance using flexible nasolaryngoscopy. Our preference is to inject via the transthyrohyoid approach using a 25-gauge needle bent at a 45-degree angle in two places (Figure 46-2). The nasal cavity is first anesthetized and decongested with 2% lidocaine and 0.025% oxymetazoline spray, followed by percutaneous transtracheal injection of 4 mL of 4% lidocaine with a 23-gauge needle just inferior to the cricoid cartilage. We feel this approach gives the best visualization and control of the injection needle, allows the tongue and larynx to remain in its natural position, and avoids the need for additional topical anesthesia to suppress the gag reflex. Performing injections with the patient awake also permits auditory feedback from patient phonation during the procedure. This allows fine-tuning of the injection volume in an attempt to obtain the best possible voice outcome.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree