Management of Choanal Atresia
Ken Kazahaya
INTRODUCTION
Choanal atresia is a relatively rare congenital anomaly that occurs in 1 in 5,000 to 10,000 live births. The incidence in females is twice that of males. Approximately 50% of choanal atresia is bilateral, 29% of cases are purely bony, and 71% are mixed bony-membranous type.
Choanal atresia is commonly associated with other congenital abnormalities in 50% to 70% of cases. Common associations include CHARGE syndrome, Apert syndrome, Crouzon syndrome, Treacher Collins syndrome, and malrotation of the bowel. Patients with choanal atresia should be evaluated for associated congenital disorders.
Embryogenesis
Facial development takes place between the 4th and 8th week of gestation. During the 4th week of gestation, prominences develop on the face of the fetus. Migration of neural crest cells from the dorsal neural folds initiates development of the nose. Neural crest cells are the main precursors of facial tissues including bone, cartilage, and ligaments. The migration proceeds laterally around the eyes and across the frontonasal process. The nasal part of the frontonasal prominence develops into the nasal placode bilaterally. The edges of the nasal placodes form medial and lateral nasal prominences. The nasal pit is a central depression between the nasal prominences. The nasal pits deepen to become the anterior nares and nasal cavity.
The oronasal membrane separates the posterior aspect of the primitive nasal cavity from the pharynx. Typically, during the 6th week of gestation, the oronasal membrane ruptures creating the choanae. With the development of the secondary palate, the choanae become located between the nasal cavity and the nasopharynx. Cells lining the nasal cavity proliferate to form an epithelial plug that subsequently resorbs.
Osseous choanal atresia is thought to be the result of the failure of the oronasal membrane to rupture. Membranous choanal atresia is thought to be caused by incomplete reabsorption of the epithelial plug. Patients who have been diagnosed with unilateral or bilateral choanal atresia should also be evaluated for other signs of CHARGE syndrome.
Another potential etiology of choanal atresia is the association with vitamin A metabolism. Dupe published a study in 2003 showing malformations in the eye and nasal regions in mice in which there was a suppression of retinoic acid synthesis in a retinaldehyde dehydrogenase knockout mouse. Notably, these mice had choanal atresia. It was also shown that the choanal atresia could be prevented by treating the mother with retinoic acid.
HISTORY
The presentation of choanal atresia can vary with the extent of nasal obstruction of an infant at birth. Choanal atresia, especially bilateral choanal atresia, causes respiratory distress in newborns, as they are obligate nasal breathers. If an infant is born with unilateral choanal atresia but has adequate patency of the contralateral side, then emergent intervention is usually not required. Infants with significant or complete nasal obstruction typically present with respiratory distress and cyanosis that improves with crying. Sometimes an oral airway or Montgomery nipple is used to maintain mouth breathing. In some cases, intubation may be necessary in order to maintain ventilation. Choanal atresia is also suspected if the physician is unable to pass a nasal suction catheter or nasogastric tube.
Patients with unilateral choanal atresia typically present between 2 and 5 years of age with unilateral nasal obstruction and persistent unilateral rhinorrhea. Because of the patency of one side of the nasal cavity, newborns with unilateral choanal atresia typically do not present with respiratory distress, unless the contralateral nasal cavity is narrowed or otherwise obstructed. Unilateral choanal atresia is sometimes misdiagnosed as a unilateral intranasal foreign body or chronic adenoiditis due to the persistent rhinorrhea.
PHYSICAL EXAMINATION
When examining an infant suspected of having bilateral choanal atresia, the anterior nasal cavity should be inspected to rule out stenosis of the piriform aperture. The nasal cavities are typically filled with secretions, and an 8-French catheter cannot be passed more than 35 mm past the anterior nasal vestibule. A mirror can be held under the nares to look for lack of fogging. A wisp of cotton wool can also be used to look for movement of air from the nares. A tympanometer can sometimes be used to look for large volume or the inability to obtain a seal. Flexible endoscopy of the nasal cavity can also be attempted to visually confirm the presence of choanal atresia. The nasal cavity should be suctioned gently to remove inspissated secretions, and a small amount of topical decongestant (e.g., oxymetazoline) may be useful to improve visualization.
INDICATIONS
Failure to sustain adequate ventilation and alimentation using conservative management.
Urgent repair should be undertaken if the infant is unable to maintain ventilation without intubation.
If it is possible to maintain ventilation and alimentation, delaying repair to allow the infant to grow is optimal to reduce the risks of anesthesia and stenosis.
Consider choanal puncture and dilation in neonates with a membranous or thin bony atretic plates.
Endoscopic transnasal repair is favored in cases of recurrent stenosis following choanal puncture and dilation, unilateral atresia in older patients, and patients with thick bony atresia plates.
CONTRAINDICATIONS
A patient who is medically unstable or unsafe for anesthesia.
The presence of a cranial base defect or abnormality affecting the height of the nasopharynx; the height of the nasopharynx may be inadequate to be able to pierce through from the nasal cavity; if this is the case, alternative airway management may be required.
An obstructive lesion of the nasal cavity, such as severe stenosis of the piriform aperture, stenosis of the nasal cavity, or an intranasal mass, will preclude the ability to open the posterior choanae even by puncture and dilatation.
Agenesis of the nose.
Endoscopic transnasal approach is precluded if the nasal cavity is too narrow.
PREOPERATIVE PLANNING
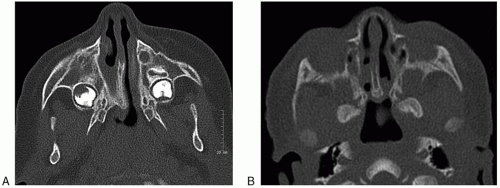
Computed tomography (CT) is the imaging modality of choice to evaluate the choanal atresia (Fig. 19.1A and B). The nasal cavity should be suctioned just prior to scanning to maximize the air-soft tissue borders within the nose. CT imaging will enable assessment of the thickness of the bony atretic plate, the membranous septum, and the degree of involvement of the lateral pterygoid plate and vomer. CT will also allow for estimation of the size and of the nasopharynx. Furthermore, CT may help to differentiate between different causes of nasal obstruction such as stenosis of the piriform aperture, nasolacrimal duct cysts, foreign bodies, nasal masses or tumors, and a deviated nasal septum.
The CT is also important for planning the surgical intervention. CT findings can reveal the amount of bone or soft tissue extending across the choanae. The inward bowing of the lateral wall of the posterior maxilla and lateral nasal wall, as well as the lateral pterygoid plate, can be assessed. Also the hard palate may be high arched and accentuated. There may also be foreshortening of the nasopharyngeal space, and the shape of the skull base and clival region should also be evaluated. The CT can also be useful in determining the amount of bone that will need to be drilled off and how much can actually be taken to open the posterior choanae. The shape of the skull base and clival region as well as the thickness of the vomer and any associated fusion with the bone laterally can also be assessed from the CT.
Image Guidance
Since a CT is obtained prior to surgery for choanal atresia, the scan may be obtained using an image-guidance protocol to allow for the use of computer-assisted image guidance. Most cases of choanal atresia can be managed without the use of image guidance; however, it may be useful if cases where there may be other craniofacial or skull base abnormalities. Given the relatively small size of the neonatal head, headframes and screw-in reference posts are difficult to place. Also given the tolerances of the system and the inaccuracies, a millimeter of error could potentially be disastrous in a newborn. In cases where computer-assisted image guidance may be needed, and the conventional reference frames cannot be used, a reference frame mounted on a Mayfield headframe, typically used in neurosurgical procedures, may be considered.
Intraoperative image acquisition such as with the cone-beam CT or O-arm (Medtronic) can be considered in some cases if available to obtain real-time imaging preoperatively or after repair of the atresia has been performed to visualize if there may be further bone that could be resected in the case of a very narrow posterior nasal cavity.
SURGICAL TECHNIQUE
Bilateral Choanal Atresia
There are a variety of techniques that are available to correct choanal atresia. Prior to the development of transnasal techniques, a transpalatal route was commonly used. Neonates can undergo repair of bilateral atresia within the first week of life.
Choanal Puncture and Dilation
One relatively simple technique used sometimes is a transnasal perforation of the atresia plate and/or membrane with dilation using Fearon dilators, mastoid curettes, ureteral dilators, or probes. This technique is particularly useful in neonates, as their nasal cavity is very small, and therefore, there is little room for instrumentation. The puncture with dilation technique is simple to perform quickly and effectively, especially for cases of membranous atresia and thin bony atretic plates.
After the neonate is anesthetized, the nasal cavity can be decongested using a topical vasoconstrictive agent, for example, oxymetazoline or cocaine. A Frazier suction tip or thin curved ureteral probe is passed into the nasal cavity pointing downward along the floor of the nasal cavity. The instrument should be kept medial along the floor of the nasal cavity to avoid penetrating the cranial base. A weak point at the junction of the nasal septum and the floor of the nose is the preferred site of gentle perforation into the nasopharynx. Once the plate
has been perforated, the probe position in the nasopharynx can be verified either by palpation with a finger passed retrograde from the oropharynx into the nasopharynx or visually using an endoscope or dental mirror to examine retrograde into the nasopharynx from the oropharynx. Increasingly larger probes can then be used to dilate the opening in the atretic plate. Typically, the size of the nares is the limiting factor in determining the diameter of the largest probe that can be used.
has been perforated, the probe position in the nasopharynx can be verified either by palpation with a finger passed retrograde from the oropharynx into the nasopharynx or visually using an endoscope or dental mirror to examine retrograde into the nasopharynx from the oropharynx. Increasingly larger probes can then be used to dilate the opening in the atretic plate. Typically, the size of the nares is the limiting factor in determining the diameter of the largest probe that can be used.
Puncture with dilation without stenting has a relative high rate of stenosis. Therefore, cut Silastic endotracheal tubes are used to stent the nasal cavity and posterior choanae. Standard silastic endotracheal tubes of inner diameter size 2.5 or 3.0 mm can be cut to fit just inside the nasal vestibule, into the nasal cavity, through the choanae and into the nasopharynx. The length and position can be checked using a mirror or endoscope looking up into the nasopharynx from the oropharynx. The stents are secured to the nasal septum with a 4-0 Prolene suture placing the knot between the stent and the nasal septum (outside the lumen of the stent). Stents are typically left in place for 3 to 6 weeks. The neonate is brought back to the operating room for removal of the stents and examination of the nasal cavity using rigid endoscopes. The posterior nasal cavity is debrided of crusts, granulation tissue, and synechiae. Serial dilations using ureteral stents or sinus balloons can be considered if there is evidence of early stenosis.
Endoscopic Transnasal Method
Stankiewicz described the use of endoscopes in 1990. The development of pediatric endoscopes and endoscopic techniques provides an approach that has become more favored than a transpalatal and microscope-assisted approach. An endoscope can be used to visualize the atretic plate and allow for the correction of the choanal atresia to be performed under direct visualization and magnification.
The technique is rather straightforward and can be performed on most neonates, unless they have a very narrow or an anatomically abnormal nose, such as by stenosis of the piriform aperture or another type of congenital nasal malformation. The mucosa of the nasal cavity is decongested with a topical vasoconstrictive agent such as oxymetazoline or cocaine. A sphenopalatine injection with an anesthetic containing epinephrine (e.g., 1% lidocaine with 1:100,000 epinephrine) is performed through the greater palatine foramen using a bent 25-gauge needle. Using the preoperative CT scan, the distance from the oral mucosal surface to sphenopalatine fossa can be estimated and the needle bent to this distance. Care must be taken not to exceed the weight-limited maximal dose of injected anesthetic (e.g., 0.7 mL/kg/dose of 1% lidocaine with 1:100,000 epinephrine), keeping in mind the need for enough volume to inject each sphenopalatine fossa and to be able to inject intranasally on both sides.
After decongestion of the nasal cavity, a 2.7-mm zero-degree or even sometimes a 4-mm zero-degree rod endoscope can be used transnasally to visualize the atretic plate. The septal mucosa and the posterior nasal cavity mucosa are injected with the topical anesthetic containing epinephrine. After allowing adequate time for the vasoconstriction to take effect, a sickle knife or curved knife (e.g., ophthalmic crescent knife) can be used to make a vertical incision through the posterior nasal septal mucosa. The incision is made approximately 1 cm anterior to the atretic plate. On one side of the septum, the incision is continued down onto the floor of the nasal cavity. On the other side, the incision starts at the floor of nose and is carried up the septum and onto the roof of the posterior nasal cavity. Posterior nasal mucosal flaps are then elevated using a Cottle or Freer elevator. A suction elevator may also be useful given the narrow nasal cavity and the potential for oozing that may be encountered.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree