Successful management of facial lesions depends on accurate diagnosis, knowledge of natural history, and use of a specific appropriate treatment. A functional classification scheme, together with history and physical examination, allows narrowing of diagnostic possibilities. Most benign facial lesions are noninflammatory, including various tumors, cysts, and melanocytic lesions (
Table 195.1). Important exceptions include specific infectious, degenerative, and metabolic conditions that clinically appear and behave as inflammatory disorders (e.g., verruca, molluscum contagiosum). “Benign” facial lesions can signal serious systemic diseases (
Tables 195.2,
195.3 and
195.4).
EPIDERMAL LESIONS
Epidermal lesions are most common, including seborrheic keratosis, actinic keratosis, comedones, milia, cutaneous horn, and epidermal cysts (
1,
2,
3,
4,
5).
Actinic keratosis (or solar or senile keratosis) is composed of small, usually multiple erythematous lesions on sun-exposed areas, such as the face, exposed scalp, and dorsum of the hands. They have a rough, adherent scale and are more easily felt than seen. Actinic keratosis can develop into squamous cell carcinoma (10% to 20%), which usually does not metastasize. The lifetime risk of squamous cell carcinoma in an individual with actinic keratosis has been estimated to be 6% to 10% (
6,
7).
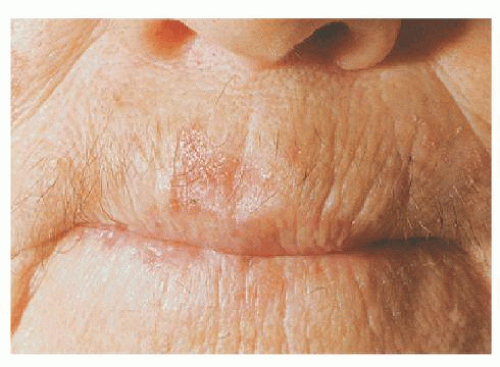
An analogous lesion to an actinic keratosis, actinic cheilitis (
Fig. 195.1), occurs on the lip’s vermilion border. It presents with hyperkeratosis, erosions, and a dull opaqueness.
Cutaneous horns (
Fig. 195.2) are hyperkeratotic conical lesions whose height is at least half their largest diameter. Various types of lesions may be present at their bases (actinic keratosis, verruca, squamous cell carcinoma, seborrheic keratosis, and rarely trichilemmoma or basal cell carcinoma). Cutaneous horns require adequate removal so their bases can be examined histopathologically (
8).
Seborrheic keratoses have brownish-black, verrucous papules or plaques with a “stuck-on” appearance, reflecting their epidermal origin. The sign of Leser-Trélat, the abrupt appearance or explosive expansion in size and number of multiple seborrheic keratoses, especially if accompanied by pruritus, has been implicated as a cutaneous marker of internal malignancy (
9,
10). In black patients, they may appear on the face as multiple brown to black papules over the cheeks, called dermatosis papulosa nigra.
Epidermal cysts are often compressible and may have visible puncta. If they have been inflamed, they may be fixed to surrounding tissue. It may be difficult to tell epidermal cysts from lipomas or neurofibromas. Lipomas are soft and often lobulated, lack puncta, and are movable against overlying skin. Neurofibromas similarly lack puncta and often display “button-holing” (described later).
Milia are small, yellowish-white, 1- to 2-mm papules. Primary milia develop spontaneously, commonly in newborns and people who are predisposed to them. Secondary
milia may develop from trauma; from subepidermal blistering diseases, in areas of topical corticosteroid-induced atrophy; or postdermabrasion. In the latter case, the milia are probably a proliferative postinjury epithelial response.
Comedones superficially resemble milia but occur in specific situations. Open comedones (blackheads) are small (1- to 2-mm) papular lesions with a central black plug. They are usually multiple, occurring with acne vulgaris or actinically damaged skin. Closed comedones (whiteheads) are 1- to 2-mm white lesions seen with acne vulgaris. Histologically, comedones are dilated cystic hair follicles filled with keratinous and lipoid material.
SKIN-APPENDAGE TUMORS
Skin-appendage tumors have diverse clinical presentations. They are common on the face and scalp because of the numerous appendageal structures there.
Many facial appendage tumors are small skin-colored papules. Trichofolliculomas occur in adults as solitary facial lesions. They have a central pore with a white woollike tuft of hair, a diagnostic feature.
Trichoepitheliomas are also small, flesh-colored papules. They are solitary or multiple. Multiple lesions are autosomal dominant, first appearing in childhood, with the number of lesions gradually increasing. Multiple trichoepitheliomas cluster around the central face and can occur with cylindromas, another benign appendage tumor often occurring on the scalp. These can grow together, resembling a turban (turban tumor). At times, trichoepitheliomas can be confused with basal cell carcinomas, both clinically and pathologically.
Trichilemmomas are small, pink to brown facial papules, in solitary and multiple forms. The multiple form can be a feature of the multiple hamartoma syndrome or Cowden disease, an autosomal-dominant genodermatosis associated with a high incidence of neoplasms (both benign and malignant) of the breast and thyroid, which occur in up to two-thirds of patients (
11). Multiple trichilemmomas occur in all patients with Cowden disease and precede development of breast cancer, allowing identification of women at risk. These lesions appear nonspecific or can resemble small verrucae. In Cowden disease, oral lesions appear as 1- to 3-mm skin-colored papules that can assume a subtle cobblestone appearance or be so extensive that they involve the entire oral cavity, including the tongue.
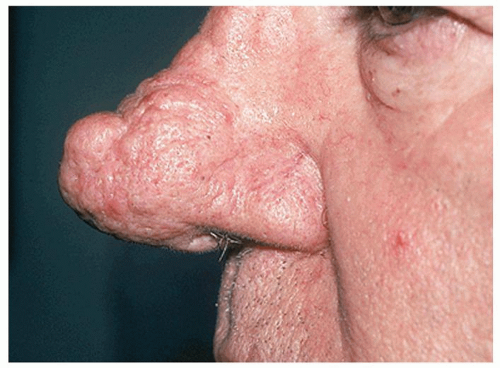
Sebaceous hyperplasia is a common papular lesion occurring in older people. It is composed of 2- to 3-mm yellow to orange lobulated papules with a slight central umbilication. They can be solitary or multiple, commonly on the forehead and nose (highest number of sebaceous glands). They are enlargements of normal sebaceous glands. They also can occur with cyclosporine use and can be a feature of acne rosacea (rhinophyma) (
Fig. 195.3).
Syringomas are small, flesh-colored to translucent papules that are intraepidermal eccrine duct adenomas. A syringoma may occur at any site on the body but are prone to occur in the periorbital area, especially the eyelids.
Syringomas often have a predilection for apocrine areas (axillae, vulva) or eruptive forms on the trunk or in dermatomal patterns. The lesions are removed from women more commonly than men, although it is not entirely clear that this represents a gender predilection rather than biopsy selection bias resulting from cosmetic or social factors.
Hidrocystomas are small, uncommon cystic periorbital lesions, most commonly seen on the eyelid margin. They are 2 to 15 mm in diameter, with a translucent bluish quality. Apocrine hidrocystomas are larger and solitary, whereas eccrine hidrocystomas are smaller and multiple.
Pilomatricomas (
Fig. 195.4) are tumors typified by follicular matrical cornification, usually presenting as a solitary, hard, deep-seated nodule, usually on the face or upper extremities. The nodules may have a faint bluish-red color and are sharply demarcated, ranging in diameter from 0.5 to 3.0 cm. They are common in children and young adults.
Nevus sebaceus (Jadassohn nevus;
Fig. 195.5) is a hamartoma that exhibits follicular, sebaceous, and apocrine malformation to varying degrees (
12). The lesion is a congenital lesion presenting as a solitary, often linear, slightly raised, orange-yellow hairless plaque on the scalp or face. Its morphologic appearance changes with the activity of underlying sebaceous glands by becoming more verrucous and nodular at puberty. It is well-established that nevus sebaceus may develop secondary adnexal neoplasms, most commonly benign but sometimes malignant. Trichoblastoma and syringocystadenoma papilliferum are the most commonly found benign neoplasm, whereas basal cell carcinoma is found in less than 1% of the cases (
13,
14,
15). Patients rarely have extensive nevus sebaceus plaques with an associated neurocutaneous syndrome (epilepsy, mental retardation, skeletal deformities).
NON-SKIN-APPENDAGE TUMORS
Lesions derived from non-skin-appendage elements include vascular, fibrous, neural, fatty, muscular, and osseous tissues (
1,
2,
3,
4).
Vascular Tumors
Cherry angiomas are a very common, benign vascular proliferation found on most adults. They are bright-red, dome-shaped papules, 2 to 4 mm in diameter, most commonly found on the trunk and extremities. Patients usually bring these to the attention of the physician when they are chronically traumatized or cosmetically undesirable.
Vascular malformations include capillary malformations (port-wine stain), venous malformations (cavernous hemangioma), lymphatic malformations (lymphangioma, lymphangioma circumscriptum, cystic hygroma), and arteriovenous malformations. It is important therapeutically and prognostically to distinguish among these. Port-wine stains (capillary malformation) are often present at birth as large, flat, pink, well-demarcated patches that demonstrate a growth pattern that parallels the growth of the child. With age, the affected skin develops a more pronounced red color, thickens, and becomes more nodular. Various syndromes are associated with capillary malformations. Sturge-Weber syndrome is a sporadic neurologic disorder in which a facial capillary malformation (usually V1 distribution of the trigeminal nerve) is associated with ipsilateral ocular and leptomeningeal anomalies. When capillary malformations occur on an extremity, a progressive overgrowth of the affected extremity may occur with underlying osteohypertrophy and arteriovenous fistulae, which is known as Klippel-Trenaunay syndrome.
Capillary hemangiomas are more common in females and premature infants. They appear between the third and fifth weeks of life, grow for several months to 1 year, and then regress. Of capillary hemangiomas, 70% regress by age 7 years. Ultimately, only 6% are cosmetically problematic.
Histologically, there is vascular endothelial cell proliferation. The most common acquired hemangioma is a pyogenic granuloma, often found on the face and extremities. It is a rapidly growing, friable, solitary red papule or polyp that frequently ulcerates and easily bleeds. Pyogenic granulomas are often precipitated by minor trauma or pregnancy.