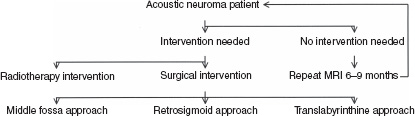
21 Acoustic schwannoma represents the most common neural tumor of the cerebellopontine angle. It results from uncontrolled proliferation of the Schwann cells located along the vestibular nerve. These tumors originate in the region of Scarpa’s ganglion at the junction of peripheral and central myelin of the vestibular nerve located in the internal auditory canal (IAC). The first documented case was reported by Bell in 1830.1 The patient had a large cerebellopontine angle lesion leading to deafness, facial paralysis, dysphagia, and severe headache. Eventual brainstem compression led to emaciation, respiratory compromise, and death. Surgical resection was deemed impossible for the next half century. It was not until 1894 that Ballance successfully removed the first such tumor.2 In the following decades, sporadic resections were performed with an astounding mortality rate of 80%. The high mortality rate led to the concept of subtotal removal. Via the posterior fossa approach, Cushing, in 1917, reported a 30% mortality rate with this strategy. Dandy, using a variant of this technique, reported similar results with total tumor resection in 1923.3 Even in the 1950s, the overall operative mortality rate still approached 40%, as reported by House.4 This led House to investigate the translabyrinthine approach. With refinement in his technique as well as improvement in microsurgical technology, House was able to report 47 consecutive translabyrinthine resection of acoustic neuromas without a fatality in 1964.5 Just as impressive were the preservation of facial nerves, absence of cerebellar trauma, and shortened convalescence in these patients. These low morbidity and mortality rates have since been duplicated by many neurotologists. On the opposite spectrum, neurosurgeons pursued the suboccipital approach during these years. With refinement of technique and microsurgical instruments, the morbidity and mortality rates from this technique had also decreased significantly. Several large series were published demonstrating the technique’s safety and efficacy.6, 7 The single most important contributing factor to these events was the widespread use of the operating microscope, pioneered by Nylen and introduced to the United States by Shambaugh. The surgical techniques have matured over the past 30 years, with only incremental refinements being added to the established procedures. However, the progress in the 21st century should now focus on the prevention of surgical complications by careful candidate selection, team cooperation with neurosurgeons, as well as approach selection. It is in these areas that the surgical complication rates from acoustic neuroma resection can be further reduced. ■ History, Physical Exam, and Patient Selection Surgical complications are best avoided by careful patient selection and surgeons experience. Part of the patient selection process requires a detailed history and physical exam. The presenting complaint, such as hearing loss, tinnitus, or dysequilibrium, must be acknowledged. The presence of dizziness may influence the decision of surgery over radiotherapy. A careful history of how symptoms impact on the patient’s quality of life must be assessed. The patient’s full medical history, including concomitant medical conditions and medications, must be obtained. Complete head and neck exam should be performed, paying special attention to cranial nerve and cerebellar examinations. Facial and trigeminal nerves, in particular, need careful evaluation and documentation. Abnormalities in these nerves, or ataxia, suggest a large tumor causing compressive neuropathy. Asymmetric facial weakness is best detected with maximal facial contraction. Fundic examination and extraocular muscle testing indicate the status of cerebrospinal fluid (CSF) pressure. Spontaneous nystagmus on examination suggests a tumor causing central compression. Similarly, a positive Romberg’s test suggests a large tumor compressing the cerebellum. Audiometric evaluations should be performed on all patients. Of particular importance are the speech reception thresholds and word recognition scores. Together, these two parameters determine the functional capability of the diseased ear. Considerations should also be given to obtaining auditory brainstem response (ABR) and electronystagmography (ENG), especially in cases where hearing preservation procedures are contemplated. Abnormal ENG results in a known tumor case suggest the superior vestibular nerve as the primary tumor site, which would be a surgically more favorable situation for hearing preservation attempts. Similarly, a normal ABR would suggest minimal cochlear nerve involvement, again indicating a more favorable situation for hearing preservation. Although not as sensitive as magnetic resonance imaging (MRI), the ABR is the most reliable and reproducible audio-metric testing available for detecting acoustic neuromas. Recent study places the sensitivity of the test at 89% in tumors less than 1 cm.8 Furthermore, ENG provides prognostic information on the postoperative compensation process. With the completion of preliminary assessment, attention should turn to radiographic analysis. Most commonly, MRI with gadolinium enhancement is obtained for the purpose of tumor diagnosis because of its superb sensitivity and specificity.9, 10 In reviewing the MRI images, several points should be examined carefully. The tumor, enhanced by the contrast, should be clearly seen in both coronal and axial sections. In addition to the size, the tumor location and extension into the cerebellopontine angle should be noted carefully. The intracanalicular component should be measured and the configuration of enhancement noted. Tumors with bright enhancement and bulging configuration within the IAC suggest compression and involvement of the cochlear nerve. In these cases, hearing preservation attempts are usually unsuccessful. The proximity of the medial portion of the tumor to the brainstem should be noted because it would impart significant weight on the selection of the surgical approach. The more medial the location, the more favorable for hearing preservation through a retro-sigmoid approach. Furthermore, gross brainstem compression with no visible CSF-containing area medial to the tumor represents urgent indication for treatment. The configuration of the cerebellopontine component, more specifically the superior and inferior extension of the tumor, should also be examined. If extreme inferior extension is noted (i.e., extension into the jugular foramen), diagnosis of other schwannomas; meningioma, vascular tumors, epidermoids, and other tumors should be entertained because acoustic neuroma rarely extends inferiorly into the region of the jugular foramen. Similarly, extension into or through the tentorium points the diagnosis away from vestibular schwannoma. Computed tomographic (CT) examination for the diagnosis of acoustic neuroma has been supplanted by the MRI. In certain cases, however, CT scan may provide additional information not available on the MRI. In cases of possible middle fossa approach, CT scan will provide depth of the canal superior details on the pneumatization of the temporal bone. This, coupled with newer neuronavigational systems, may enhance accuracy for less experienced surgeons. The relative position of the sigmoid sinus can be clearly delineated on the CT scan. The position of the jugular bulb can also be determined. As a rule of thumb, if the jugular bulb is seen on axial CT at the level of the basal turn of the cochlea, then a high jugular bulb can be assumed. The position of the jugular bulb near the posterior canal or IAC may have an influence on choice of approach in some patients. Furthermore, calcification within the tumor will be demonstrated on the CT scan more clearly than on MRI. This finding suggests a diagnosis of meningioma rather than acoustic neuroma. ■ Indications for Surgery After experience in surgery, careful patient selection is the first and the most important step in avoiding complications. No specific set of rules governs this selection process, and each case should be assessed individually. In a stepwise fashion, the first step involves deciding the need for intervention versus observation. If intervention is chosen, surgical resection versus radiotherapy is considered. Finally, the optimal surgical approach should be chosen based on the given situation. In this time of Internet information, patients still need guidance but are allowed a final choice in their medical care. Fig. 21–1 provides a decision algorithm for patient selection. FIGURE 21-1 Algorithm for initial patient selection. Pending medical status and MRI scans. The risks and benefits should be carefully weighed to arrive at the most appropriate recommendation for surgical intervention. The goals of surgical intervention are to improve the patient’s quality of life, reduce the risk of complication from the tumor, minimize the possibility of surgical morbidity, and minimize the postoperative complication rates. Table 21–1 and 21–2 summarize those factors considered in arriving at the optimal management of the individual with acoustic neuroma. Furthermore, merits and pitfalls of each of the surgical approaches are considered. The complex processes of deciding whether to intervene should begin with the patient’s symptoms as obtained in the history. Signs and symptoms of brain-stem or cerebellar compression constitute urgent indications for intervention. Similarly, debilitating symptoms such as recurrent vertigo and severe dysequilibrium are stronger indications for surgical intervention. Radiographic evidence of brainstem compression also requires intervention. In patients with documented tumor growth by serial imaging examinations, as in patients under the observation category, intervention should be implemented early to reduce the risks of subsequent complications from either the tumor or the intervention. The patient’s individual decision with full understanding of the risks and benefits constitutes the most important aspect of this process. On the contrary, patients with small tumors with minimal symptoms may be better served with observation. An exception to this statement is the patient disabled by intermittent disequilibrium. However, the risk of observing the tumor must be accepted by the patient, particularly the small risk of sudden, unilateral hearing loss. A regular follow-up schedule should be provided to the patient. If new symptoms appear, the patient should be reevaluated. If intervention was not absolutely indicated or declined by the patient, observation with serial imaging examinations is an acceptable alternative. In this case, follow-up MRI examination should lead to review of the case beginning at the top of the algorithm chart. Decision analysis should be renewed with each follow-up visit, especially if there is onset of new symptoms. Problem Prevention/Treatment Determining most appropriate management of acoustic neuroma Determination of patient’s symptoms, effect on quality of life, general health, and preference Asymptomatic acoustic neuroma less than 1 cm in maximum diameter Consider observation with regular imaging of cerebellopontine angle and IAC Asymptomatic acoustic neuroma with demonstrated growth on serial imaging Consider active intervention as either surgical resection or radiotherapy Symptomatic acoustic neuroma less than 1 cm in maximum diameter Consider active intervention as either surgical resection or radiotherapy Patient preference is key, as well as age considerations Acoustic neuroma greater than 1 cm in greatest diameter Consider active intervention as either surgical resection or radiotherapy Patient preference is key Surgical treatment of acoustic neuroma in a patient with serviceable hearing Evaluate likelihood of hearing preservation considering results of caloric and ABR testing Consider tumor morphology (predominantly intracanalicular with minimal CPA component versus a predominantly CPA tumor with minimal involvement of internal auditory canal) Acoustic neuroma with serviceable hearing in a predominantly CPA tumor with extension into up to two thirds of IAC and caloric testing consistent with a superior vestibular nerve tumor and a normal ABR Retrosigmoid approach to CPA Acoustic neuroma with serviceable hearing in a predominantly CPA tumor with extension beyond two thirds of IAC and caloric testing consistent with a superior vestibular nerve tumor and a normal ABR Translabyrinthine approach Acoustic neuroma with a dilated IAC Acoustic neuroma with unfavorable caloric and ABR testing results Acoustic neuroma greater than 2 cm in maximum diameter Acoustic neuroma with serviceable hearing and a predominantly intracanalicular tumor and favorable caloric and ABR testing results
Management of Acoustic Neuromas
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
