26
Malignant Tumors of the Temporal Bone
Chandra M. Ivey and Myles L. Pensak
Malignant tumors of the temporal bone are often diagnosed at late stages of disease and portend a dismal prognosis. Symptoms are often analogous with those of chronic suppurative ear disease, and thus, in the absence of a high suspicion for malignancy, are treated as such. Electrophysiologic and neuroradiologic investigations may assist in the suggestion of malignant characteristics, and this heightened suspicion combined with contemporary skull base surgical techniques, adjuvant radiotherapy, and chemotherapy may improve survival rates over time. This chapter summarizes the pathobiology of temporal bone malignancies, the current literature on management options available at this time, and pain management options for palliative treatment for patients with these tumors.
 Anatomy of the Temporal Bone
Anatomy of the Temporal Bone
The temporal bone is positioned between the middle and posterior cranial fossa and is constituted of four distinct segments: petrous, squamous, mastoid, and tympanic.1 The petrous portion of the temporal bone contributes to the skull base of both the middle and posterior fossa, and is directed anteriorly and medially, juxtaposing the clivus and sphenoid. The squamous portion contributes to the lateral skull enclosing the temporal lobe of the brain. The mastoid portion contributes to the inferior-lateral skull base, and both enlarges and pneumatizes over the first few years of life to eventually overlie the stylomastoid foramen. The tympanic segment, although poorly developed at birth, forms the majority of the bony external auditory canal (EAC) and grows to maturity by age 3. The foramen of Huschke delineates the inadequate closure of the tympanic ring anteriorly.
Pneumatization of the petrous and mastoid portions of the temporal bone vary widely. The mesotympanum defines the largest pneumatized space and communicates directly with the eustachian tube anteriorly. This space communicates with the mastoid central air-cell tract via the aditus ad antrum, which then in turn may lead to perilabyrinthine, retrofacial, perisinus, apical, epitympanic, and sinodural air-cell tracts.2
Although there are many natural retardants to tumor spread within the temporal bone, some specific anatomic relationships within this region may assist in the extension of malignancy. The natural cleavage planes within the fibroelastic cartilage of the EAC, the fissures of Santorini, may allow delivery of tumor anteriorly to the parotid gland and posteriorly to the soft tissue lateral to the mastoid process. Incomplete closure of the foramen of Huschke also permits anterior spread into the parotid and glenoid fossa. If tumor invades the middle ear space, and thus the mesotympanum, there is potential for spread anteriorly through the eustachian tube to the infratemporal fossa and parapharyngeal space. This area also provides unimpeded access to all areas of the petrous bone through the central air-cell tract. Although the bony partitions of the temporal bone may retard direct tumor spread, as bony erosion occurs over time, access is allowed anteriorly toward the infratemporal fossa, inferiorly toward the jugular fossa, superiorly into the middle cranial vault, or posteriorly toward the posterior fossa.
Although there are recognized pathways of lymphatic drainage from the area around the temporal bone, metastatic spread from the area is not common.3–6 When lymphadenopathy occurs, it is often associated with a secondary inflammatory process rather than with direct tumor involvement, but metastases have been reported in 10 to 15% of cases.7,8
Lymph nodes within the parotid and preauricular region receive drainage from the conchal bowl, cartilaginous canal, tragus, and fossa triangularis. Infraauricular lymph nodes receive drainage from the lobule and antitragus. Postauricular, or deep jugulodigastric lymphatics, along with spinal accessory lymphatics receive drainage from the helix and antihelix. The EAC lymphatics drain anteriorly into the preauricular and parotid lymph nodes, inferiorly into the upper cervical and deep internal jugular nodes, and posteriorly into the postauricular nodes. The middle ear has a reticular lymphatic network surrounding the eustachian tube and draining into the upper jugular and retropharyngeal lymph nodes. The inner ear has no known lymphatic drainage.
 Clinical Presentation and Assessment of Malignant Temporal Bone Tumors
Clinical Presentation and Assessment of Malignant Temporal Bone Tumors
Often indistinguishable from chronic suppurative otitis, patients with temporal bone malignancies commonly present with aural discharge, fullness, and hearing loss. Although bloody drainage may occur, it is more concerning in conjunction with pain. Symptoms more alarming for malignancy are cranial neuropathies, including facial paralysis and cochleovestibular deficits. Signs of meningeal involvement, including severe headache, may be late findings. Table 26–1 lists the signs and symptoms found in the University of Cincinnati tumor registry recorded for patients with malignant temporal bone tumors from 1984 to 2005.
A complete history and neurotologic examination is essential in the evaluation of a temporal bone tumor. Audiometric, electrophysiologic, and neuroradiologic studies may also assist in defining the extent of tumor growth and the involvement of surrounding structures. Baseline studies can elaborate the etiology of hearing loss; audiometrics, including discrimination scores and acoustic reflexes, along with auditory brainstem response (ABR) may be used to assess retrocochlear pathology. Impedance assessments and tympanometry may help define middle ear involvement. Electronystagmography, rotation chair analysis, and platform posturography are of limited value, but will be abnormal if the integrity of the vestibular apparatus has been compromised.
Contemporary imaging techniques such as computed tomography (CT) and magnetic resonance imaging (MRI) have become gold standards for temporal bone assessment.9–11 Adjuvant studies such as angiography, magnetic resonance angiography (MRA), and magnetic resonance venography (MRV) may also help in evaluation.12
CT performed at 1-mm intervals in a high-density bone window mode provides significant information regarding the status of the temporal bone and skull base. Bony erosion or disruption of the EAC, tegmen, or jugular foramen/carotid canal region may suggest the presence of a malignant process. The ossicles, semicanal of the tensor tympani muscle, and the eustachian tube are well defined on CT, and extratemporal involvement, including parotid, infratemporal fossa, and intracranial extension, can be easily appreciated11,13 (Fig. 26–1).
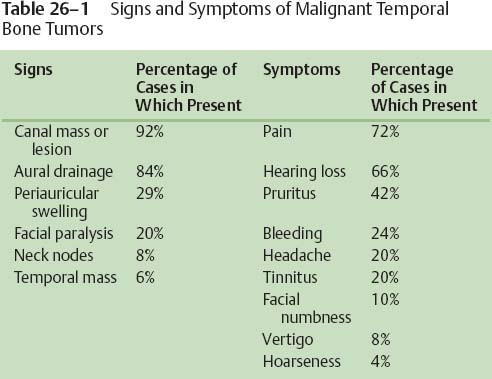

Figure 26–1 Extensive bone erosion is noted in this high-resolution axial computed tomography (CT) of the temporal bone.
Although MRI does not define bony erosion as well as CT does, it provides information about soft tissue involvement within the middle ear or other pneumatized spaces.11,12 MRI may also show enhancement of the foramina, elucidating the spread of tumor along these pathways as well as extratemporal spread to surrounding structures. Dural violation as well as vascular involvement may be easily defined on MRI. MRA and MRV also display tumor vascularity, and may assist in further characterization of the tumor, as well as the patency of the surrounding vasculature due to analysis of flow voids (Fig. 26–2B).
Invasive vascular studies are performed less frequently for simple characterization of tumors since the increasing use of MRA and MRV. These studies may still assist in defining a patient’s vascular arborization and thus the ability to tolerate internal artery compromise by means of xenon-131-assisted or balloon-occlusion studies. Carotid artery sacrifice may be indicated based on involvement of primary tumor or by the need for vascular control if heavy intraoperative bleeding is encountered. Embolization, although infrequently used, may be helpful in the perioperative setting to decrease bleeding from highly vascular tumors.
Although radionuclide studies are less helpful in initial evaluation of malignancy due to inflammation present in the area, they may be used to differentiate between recurrence and areas of osteoradionecrosis or infection.
Staging criteria for temporal bone malignancy have been published, but as of yet there is no universally accepted system. Although the American Joint Committee on Cancer uses the same staging system that has been applied to cutaneous malignancies at other sites, the unique anatomy of the temporal bone makes these criteria inadequate. Suggested staging systems have focused on tumor size and clinical appearance, as well as CT appearance of tumors.12,14,15 Tables 26–2 and 26–3 list the proposed staging systems from Arriaga et al and Pensak et al. Recently, Nakagawa et al16 modified the Pittsburgh staging system to include tumors with infratemporal fossa involvement into the T3 category. Interestingly, research from this group has displayed an increased survival benefit for these tumors after radical surgery and preoperative radiation that has not been previously demonstrated.
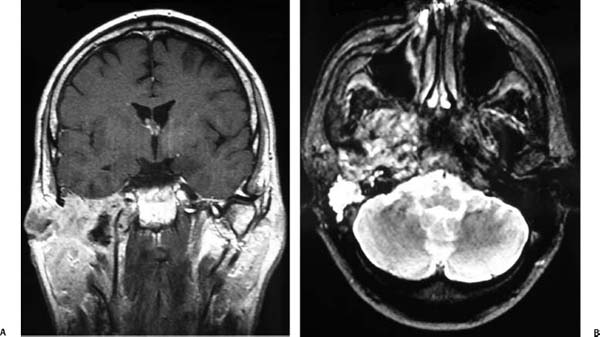
Figure 26–2 (A,B) Significant infratemporal fossa invasion is reflected by loss of soft tissue planes on magnetic resonance imaging (MRI) scan in both coronal and axial planes.
| State | Description/Definition | |
|---|---|---|
| T1 | Tumor limited to external auditory canal without bony erosion or evidence of soft tissue extension | |
| T2 | Tumor with limited external auditory canal bony erosion (not full thickness) or radiographic finding consistent with limited (<0.5 cm) soft tissue involvement | |
| T3 | Tumor eroding the osseous external auditory canal (full thickness) with limited (<0.5 cm) soft tissue involvement or tumor involving the middle ear and/or mastoid or patients presenting with facial paralysis | |
| T4 | Tumor eroding cochlea, petrous apex, medial wall of the middle ear, carotid canal, jugular foramen, or dura, or with extensive (>0.5 cm) soft tissue involvement | |
| N status | Involvement of lymph nodes is a poor prognostic finding and automatically places patient in an advanced stage [either stage III (T1N1) or stage IV (T2-T4N1)] | |
| M status | Distant metastasis indicates a poor prognosis and immediately places patient in stage IV | |
| Grade | Description/Definition | |
|---|---|---|
| I | Tumor in a single site, 1 cm or smaller | |
| II | Tumor in a single site, larger than 1 cm | |
| III | Transannular tumor extension | |
| IV | Mastoid or petrous air-cell invasion | |
| V | Periauricular or contiguous extension (extratemporal/dural invasion) | |
| VI | Neck adenopathy, distant anatomic site, or infratemporal fossa extension | |
 Pathology of Malignant Temporal Bone Tumors
Pathology of Malignant Temporal Bone Tumors
Squamous cell carcinoma accounts for about 85% of malignancies of the EAC and petrous bone, although basal cell carcinoma (BCC) accounts for the majority of lesions on the pinna.17–20 Other primary tumors of the temporal bone include glandular tumors, rhabdomyosarcoma, regionally invasive cancers, and metastatic disease, altogether accounting for the other 15% of tumors found in this region.21–23 Table 26–4 lists benign, aggressive benign, and malignant tumors of the temporal bone, and Table 26–5 lists malignant tumors of metastatic origin found to invade the temporal bone.
Squamous cell carcinoma most frequently appears within the cartilaginous portion of the EAC. Presenting patients are in the fifth to sixth decade and often have a history of chronic aural drainage, pain, and hearing loss. Misdiagnosis as suppurative otitis media or otitis externa accounts for these patients initially being treated with multiple courses of topical and systemic antibiotics without symptom resolution prior to biopsy being performed. As tumor extension occurs, chronic otalgia and cranial nerve damage (sensorineural hearing loss, facial weakness) become evident. Chewing and swallowing may become involved with tumor extension into the glenoid fossa and infratemporal fossa. Although significant local growth of these tumors may be evident at diagnosis, regional lymphatic metastasis is infrequent.
Although no etiologic factors have been found to explain squamous cell carcinoma of the EAC, predisposing conditions that have been examined include radiotherapy to the area, chronic otitis media, chronic otitis externa, cholesteatoma, and lymphoproliferative disorders. A select group of these patients have a common history of radium exposure. Squamous cell carcinoma is the second most common tumor of the auricle and is often related to sun exposure and local trauma.
| Benign | Aggressive Benign | Malignant | ||
|---|---|---|---|---|
| Meningioma, low grade | Chondroblastoma | Squamous cell | ||
| Schwannoma | Plasmacytoma | Basal cell | ||
| Paraganglioma | Hemangiopericytoma | Ceruminous gland tumor | ||
| Osteoma | Hemangioendothelioma | Rhabdomyosarcoma | ||
| Adenoma | Meningioma, high grade | Melanoma | ||
| Chordoma | Adenoidcystic | |||
| Lipoma | Chondrosarcoma | |||



