Malignant External Otitis
Marlene L. Durand
Malignant otitis externa (MOE) is an invasive bacterial infection of the external auditory canal and skull base. It involves the soft tissues adjacent to the skull base and often progresses to osteomyelitis of the skull base. It occurs primarily in elderly patients with diabetes mellitus and is nearly always due to Pseudomonas aeruginosa. Patients typically present with weeks to months of unilateral ear pain and drainage. Cranial neuropathies may be present; a facial nerve palsy is the most common. Patients are usually afebrile and appear nontoxic. Physical examination may be normal except for the finding of granulation tissue in the mid-external auditory canal. Computed tomography (CT) or magnetic resonance imaging (MRI) may demonstrate bony erosion of the skull base. Cultures of purulent drainage and of the granulation tissue in the ear canal should be taken prior to starting antibiotics. Treatment consists of prolonged (at least 6 weeks) systemic antibiotic therapy; surgical debridement is almost never necessary.
The disease was first described by Meltzer and Kelemen in 1959 (1). In 1968, however, Chandler was the first to name it “malignant otitis externa” when he described 13 patients with the infection, seven of whom died (2). Since then, the disease has also been labeled “necrotizing,” “progressive,” and “invasive” otitis externa (3, 4, 5), although “malignant” remains the most commonly used adjective.
PATHOGENESIS
Pseudomonas is not a normal colonizer of the ear canal in either diabetic or nondiabetic patients (6). It is a waterloving organism, however, and can be cultured from sinks and faucets, as well as lake and tap water. It is not clear why this organism is the predominant cause of otitis externa and MOE, although its predilection for warm, moist environments may be a partial explanation.
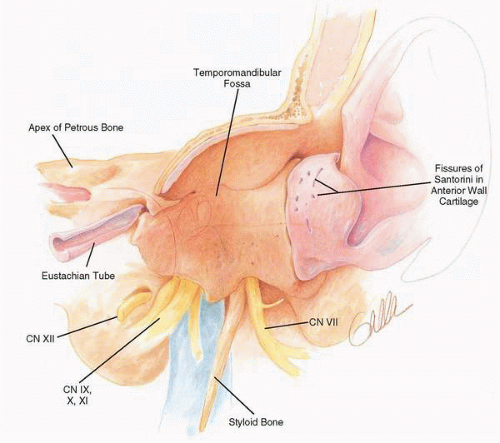
Pseudomonas bacteria in the ear canal are thought to invade through the fissures of Santorini into deeper soft tissues, temporal bone, and then skull base (Fig. 20.1). The facial nerve becomes involved as the infection spreads through the stylomastoid foramen. Cranial nerves (CN) IX, X, and XI may be affected if the infection spreads to the jugular foramen and CN XII as the infection extends to the hypoglossal canal. Infection of the petrous apex may involve CN VI and less often CN V. Extension into the temporomandibular joint may cause a destructive osteomyelitis (7).
Most patients with MOE are diabetic, but hyperglycemia per se is probably not a factor in pathogenesis of MOE (8). Rather, the microangiopathy caused by diabetes most likely leads to hypoperfusion in the skin of the temporal bone and increased local susceptibility to infection (5). A histopathologic study of two patients who died from MOE revealed thickening of periodic acid-Schiff-positive material in the subendothelial basement membrane of the capillaries in skin overlying the temporal bones (5). Most patients with MOE are over age 60, and blood vessel changes occur with aging as well.
RISK FACTORS
Diabetes mellitus is the major risk factor for MOE; in most series, diabetic patients account for more than 90% of cases (5,8). Unlike diabetic patients with mucormycosis, ketoacidosis in patients presenting with MOE is very rare and diabetes is often mild. Combining data on 35 diabetic patients in three recent series of MOE studies where specific diabetic status was reported, 20% were diet controlled, 40% used oral hypoglycemics, and only 40% were insulin dependent (9, 10, 11).
Irrigation of the external ear canal to remove cerumen may be a risk factor for MOE. Rubin and colleagues reported that nearly two thirds of their patients with MOE had a history of aural irrigation with tap water within a few days prior to the onset of symptoms (12), and others have also noted this association (13,14).
Older age is also a risk factor for MOE, and the average age of patients in several series was 67 or older (8). Malignant otitis externa is rare in children, and those who develop the disease usually do not have diabetes but are immunocompromised (e.g., malignancy, chemotherapy) (15,16).
Nondiabetic adults may also develop MOE, and many such patients are immunocompromised. Although nondiabetics generally account for fewer than 10% of patients, two groups from Israel have reported that 22% (5 of 23) (9) and 30% (9 of 30) (17) of their MOE patients had no risk factors other than age (all older than 65 years).
Nondiabetic adults may also develop MOE, and many such patients are immunocompromised. Although nondiabetics generally account for fewer than 10% of patients, two groups from Israel have reported that 22% (5 of 23) (9) and 30% (9 of 30) (17) of their MOE patients had no risk factors other than age (all older than 65 years).
Nondiabetic patients with acquired immunodeficiency syndrome (AIDS) may develop MOE, although few such patients have been reported. Aspergillus was the pathogen in two AIDS patients with MOE, Pseudomonas in four others (18).
CLINICAL PRESENTATION
Most patients with MOE have chronic otorrhea and otalgia. Duration of symptoms prior to diagnosis is usually weeks to months, even in recent series (10). Patients may develop otorrhea prior to the onset of pain. The amount of drainage is variable. When ear pain develops, it initially may be mild, gradually increasing over several weeks to a deep, aching, persistent pain. It is often worse at night, awakening the patient from sleep (19). Patients may complain of headache, especially temporal and parietal on the affected side. Temporomandibular joint pain and tenderness may occur, and pain may be so severe that patients avoid chewing (8). One third of patients complain of hearing loss (5). Patients usually have no systemic symptoms of infection, such as fever, chills, or night sweats.
Facial nerve palsy was found on presentation in approximately one third of patients in older series (5) and generally developed after at least 2 months of symptoms (20). Rarely facial palsy appears as early as 1 week after onset of illness. Other cranial neuropathies develop after the appearance of
facial palsy and have been a poor prognostic sign (5). Cranial nerves IX, X, XI, and XII are more often involved than V and VI. Only one patient has been described with documented cranial nerve II involvement (21). This patient developed unilateral blindness from optic nerve invasion by Pseudomonas after a 2-year course of refractory MOE involving multiple cranial nerves (VI, VII, IX, X, XII). Cranial nerve III palsy had developed in the affected eye 2 weeks earlier. It should be emphasized, however, that cranial neuropathies are usually late findings in MOE. In a recent series of 23 patients diagnosed soon (1 to 6 weeks) after onset of symptoms, no patient presented with cranial neuropathies (22).
facial palsy and have been a poor prognostic sign (5). Cranial nerves IX, X, XI, and XII are more often involved than V and VI. Only one patient has been described with documented cranial nerve II involvement (21). This patient developed unilateral blindness from optic nerve invasion by Pseudomonas after a 2-year course of refractory MOE involving multiple cranial nerves (VI, VII, IX, X, XII). Cranial nerve III palsy had developed in the affected eye 2 weeks earlier. It should be emphasized, however, that cranial neuropathies are usually late findings in MOE. In a recent series of 23 patients diagnosed soon (1 to 6 weeks) after onset of symptoms, no patient presented with cranial neuropathies (22).
The classic finding on physical examination is granulation tissue in the inferior portion of the ear canal, at the bony cartilaginous junction. The canal is often edematous and erythematous. A purulent discharge is nearly always present. The tympanic membrane is often obscured by granulation tissue, but when visible it is often intact (5). There may be periauricular tenderness and pain with movement of the pinna. Tenderness is often present in the lateral aspect of the infratemporal fossa and may be elicited by digital pressure between the mandible and mastoid tip. Hearing loss may be evident in the affected ear. Facial palsy and other cranial neuropathies may be present, as noted earlier. The remainder of the physical examination is usually unremarkable.
LABORATORY FINDINGS
Routine chemistry studies are normal aside from an elevated glucose level in diabetic patients. The white blood cell count is usually normal or minimally elevated. The cardinal laboratory abnormality in MOE is the erythrocyte sedimentation rate (ESR), which is elevated in nearly every patient. It is often markedly elevated (more than 50 mm/hour) and is one of the few nonrheumatologic conditions that cause elevation greater than 100. One group reported that the ESR was elevated in all 25 of their MOE patients, with mean value of 87 mm/hour (8). The ESR decreases over several weeks with appropriate therapy. Relapse of infection after apparently successful therapy is often heralded by renewed ESR elevation.
BACTERIOLOGY
P. aeruginosa, an aerobic gram-negative bacillus, is the cause of nearly all cases of MOE. However, cultures of purulent drainage and granulation tissue should be obtained prior to starting systemic antibiotics in all patients for two reasons. First, it is important to determine antibiotic susceptibility of the Pseudomonas strain prior to starting prolonged therapy, and second, rare cases of MOE may be due to other organisms. If cultures are only obtained after starting systemic antibiotics, a culture that doesn’t grow Pseudomonas may be discounted as falsely negative.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree