(1)
St. Johns, FL, USA
(2)
Helen Keller Foundation for Research and Education, International Society of Ocular Trauma, Birmingham, AL, USA
(3)
Consultant and Vitreoretinal Surgeon, Milos Eye Hospital, Belgrade, Serbia
(4)
Consultant and Vitreoretinal Surgeon, Zagórskiego Eye Hospital, Cracow, Poland
50.1 General Considerations
The question whether to surgically intervene for a macular condition should be decided based neither on the appearance of the posterior pole nor on the VA level.1 Appearance can be deceiving in both directions: what looks like a horrible anatomical situation may still permit good vision; conversely, even a seemingly minor abnormality may cause severe visual loss.
Pearl
In macular diseases where traction plays a part, metamorphopsia is usually more important for the patient’s quality of life than the VA; it is therefore imperative that the ophthalmologist not focus on the VA alone when determining the severity of the condition. This also helps to avoid the sadly common habit of using an arbitrary cutoff VA value to indicate or deny surgery (see Chap. 5).
50.1.1 VMTS
The condition is characterized by an anomalous PVD with strong focal residual adherences to the central retina. The central vitreous may prolapse through an opening in the posterior vitreous cortex and adhere to the foveal region. OCT is a great tool in showing the condition preoperatively and the results of surgery (see Fig. 50.1).2 The posterior cortical vitreous has a sheet-like appearance, which can be traced all the way to the vitreous base. The problem is therefore not confined to the posterior pole; the risk of causing a retinal tear is increased throughout the fundus.
Fig. 50.1
OCT imaging of an with VMTS. (a) Preoperative image showing severe traction on the fovea. The retina is elevated and shows cystoid changes. The split in the posterior cortical vitreous is clearly seen (on the right of the image, a vitreoschisis cavity has formed). (b) The image 1 month postoperatively shows a much improved retinal contour; the functional improvement, however, is primarily determined by the duration of the pathology. Do the operation late and the vision will barely improve
In VMTS intravitreal ocriplasmin (enzymatic vitreolysis) has a decent chance of success, especially if the area of vitreomacular adhesion is less than 1,500 μ.3
50.1.2 Cellophane Maculopathy
Defined here as “surface-wrinkling maculopathy,” it may be a standalone pathology or the initial step in the formation of a macular pucker. No scar tissue is visible but the retinal surface (ILM) is wrinkled (see Fig. 50.2), and the patient may experience metamorphopsia.
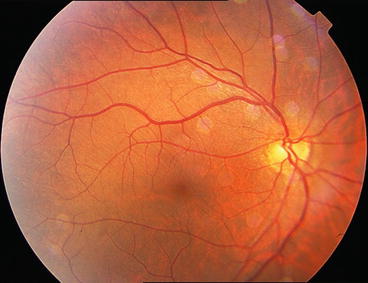
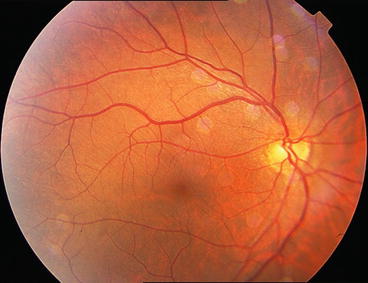
Fig. 50.2
Cellophane maculopathy, preoperative view. Very fine folding of the ILM is visible, especially in the superotemporal area. The folds are not full thickness as EMP-induced folds would be
50.1.3 Macular Pucker
In this condition a true scar forms over the macular surface, which is why many surgeons call it a “mini PVR.” The scar contracts and causes anatomical (edema, retinal folds, hemorrhages, ectopia, corkscrew-like configuration of blood vessels etc.; see Fig. 50.3) and functional (drop in VA, metamorphopsia) abnormalities. The membranes are made mostly of collagen with relatively few cells. They may be secondary to a disease4 or treatment5 but in most cases they are idiopathic.


Fig. 50.3
EMP causing severe changes in the macular anatomy. This a rather centrally located scar, which is understandably responsible for a loss in VA. The metamorphopsia it also causes is explained by the traction the contracting scar exerts on the retina, leading to full-thickness folds, hemorrhages, and distorted vessels
Some ophthalmologists started giving patients with EMP intraocular anti-VEGF injections (see Chap. 43). This medication indeed helps temporarily if the edema is the main culprit in the reduction of the VA. However, recurrence of the fluid is inevitable, and the retinal changes that manifest themselves as metamorphopsia for the patient will not be addressed by any type of medication. The only chance for a definite cure is surgery.6
50.1.4 Macular Hole
VR as well as tangential (surface) traction causes the retraction of the retina from the epicenter; it is often accompanied by an EMP.7
50.2 Surgical Technique8
50.2.1 VMTS
Start the vitrectomy in front of the posterior pole and create a small pocket just above the macula.
The fovea is already under severe traction: start cutting as soon as you start aspirating.9
Inject a minimal amount of TA so that the vitreomacular interface is clearly delineated.
Severe the connection between the posterior vitreous and the retina.
It may be necessary to use scissors if the posterior cortical vitreous has formed a strong, distinct sheet. There is greater control if the cutting is done with scissors. Use of the probe is limited anyway because it is impossible to “sink its teeth into the membrane” as no edge is available (see Fig. 38.2b, right hand side).
Once the macula is freed from all vitreous adhesions, continue with a careful PVD.
As mentioned above (Sect. 50.1.1), strong adhesion between the membrane-like posterior hyaloid cortex and the retina can exist anywhere. Be slow with the PVD and do not try to carry it too far anterior; even then, the adhesion between retina and the cortical vitreous is similar to two sheets of paper glued together. The strength of this adhesion is shown by the appearance of small hemorrhages as you try to detach the hyaloid, forcing you to choose from two options: continue with the PVD and risk an intraoperative retinal tear formation, or leave the adhesion behind and risk that tears occur postoperatively.10 The dilemma is similar to that described under Sect. 32.3.1.4, except that in the case of a VMTS retinectomy is not an option any surgeon would prefer choosing.
Be mindful that if the condition has been present for a long time, the central retina may a have convex, rather than concave, configuration.11 This is important to keep in mind both for the creation of the PVD and the peeling of the ILM.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


