Lens Care and Patient Education
Edward S. Bennett
Heidi Wagner
The ability to care for and handle rigid gas-permeable (GP) contact lenses properly depends on several factors. First, the patient must be provided with several methods of insertion and removal, and proficiency in these methods must be demonstrated before leaving the office. Second, the patient must be aware of the function of each solution in the recommended care regimen, the importance of performing each function properly and regularly, and the basis for which other solutions are not compatible with the particular material. Third, several methods should be provided to both educate the patient and reinforce the education. The patient must know the “do’s and don’ts” of the newest GP lenses; in other words, the patient must recognize the limitations of the lenses and the problems that can occur through noncompliance. The purpose of this chapter is to provide an overview of the ways in which these important factors can be satisfied, thereby enhancing the probability of patient success.
▪ CARE REGIMEN
Wetting and Soaking
The majority of solutions used for wetting and soaking GP lenses combine several functions into one solution. These solutions have four major functions1:
To temporarily enhance the lens surface wettability.
To maintain the lens in a hydrated state similar to that achieved on the eye.
To disinfect the lens.
To act as a mechanical buffer between the lens and cornea.
The specific formulation of the ingredients in these solutions, especially the preservatives and wetting agents, is very important.
Preservatives
Preservatives are capable of either killing microorganisms (bactericidal agents) or inhibiting their growth (bacteriostatic agents).2 They are the active ingredients in these solutions (and all other GP care solutions) that should perform the following functions3:
Provide the necessary degree of disinfection.
Preclude toxic reactions.
Avoid adverse effects on lens surface wettability and parameters.
Enhance compatibility with the tear film.
There are numerous preservatives currently in common use, all differing in their mode of action and effectiveness. The most common preservatives include benzalkonium chloride (BAK), chlorhexidine, thimerosal, ethylenediamine tetraacetate (EDTA), polyaminopropyl biguanide (PAPB), polyquarternium-1 (polyquad), and benzyl alcohol (Tables 6.1 and 6.2).
TABLE 6.1 STORAGE AND DISINFECTION SOLUTIONS | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
Benzalkonium Chloride:
Benzalkonium chloride is a quaternary ammonium compound that is effective against a wide spectrum of bacteria and fungi and normally is used at a concentration of 0.004%. It was first introduced as a preservative in the late 1940s and is currently used in the majority of ophthalmic preparations. The effectiveness of BAK is enhanced when it is used in combination with EDTA, allowing a lower concentration than otherwise necessary.4 It is not used as a preservative with soft lens solutions because the soft polymer will bind the preservative and actually concentrate it, thereby allowing it potentially to reach toxic levels and cause ocular injury.5
Chlorhexidine:
Chlorhexidine is bactericidal in action and traditionally has been used in a concentration of 0.0005% in soft lens chemical disinfection solutions. However, unlike soft lenses, the binding capacity of chlorhexidine to GP lenses appears to be limited because of the wettability of GP lenses and chlorhexidine’s large molecular structure.6 Although chlorhexidine has been reported to have an excellent spectrum of antimicrobial activity, it has limited effectiveness against yeast and fungi; therefore, it often has been combined with EDTA for greater effectiveness. In addition, chlorhexidine has been found to be relatively ineffective against Serratia marcescens.7
Thimerosal:
Thimerosal is a bactericidal organic mercurial compound that at one time was a commonly used soft lens solution preservative. However, some patients are sensitive to organic mercurial compounds and experience a burning sensation and associated clinical signs of redness and superficial punctate keratitis.8,9 In addition, it is slow-acting in nature and, in low concentrations, may be ineffective against Pseudomonas.2,10 Although thimerosal has been found to be compatible with GP lenses, exhibiting only rare sensitivity reactions, for optimal antimicrobial effectiveness it should be used in combination with another preservative such as chlorhexidine.11 It has largely been eliminated from contact lens care systems.
Ethylenediamine Tetraacetate:
EDTA is a chelating agent and not a true preservative. However, it is commonly used in combination with BAK and other preservatives in GP contact lens solutions because of its synergistic ability to enhance the bacterial action of pure preservatives against Pseudomonas.12
TABLE 6.2 COMBINATION SOLUTIONS | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Polyaminopropyl Biguanide:
PAPB has been used as a preservative in soft disinfection regimens because of its low sensitivity rate. It has supplemented chlorhexidine as a preservative in one of the GP care systems because it exhibits greater antimicrobial effectiveness, notably against Serratia marcescens.7 However, in the concentration used in GP lens solutions, which is 30 to 50 times the concentration used in soft lens solutions, the potential for toxicity reactions has been documented.13,14 However, when reduced in concentration by one-third, it has demonstrated excellent antimicrobial activity in comparison with other systems.15 It has also demonstrated effectiveness against Acanthamoeba.16
Polyquaternium-1:
Polyquaternium-1 is a large cationic (+) polymer that also is similar in molecular structure to chlorhexidine. The quaternary ammonium group has a lower cationic (+) charge than polyhexamethylene biguanide and, as a result, is used at higher concentrations.17 It is less likely to produce toxic or allergic reactions than previously developed preservatives such as benzalkonium chloride and thimerosal.17
Benzyl Alcohol:
Benzyl alcohol originally was considered for use as a solvent for contact lens materials; however, it was also found to have good disinfection capabilities. Pure benzyl alcohol possesses certain physicochemical characteristics that are regarded as ideal for an ophthalmic preservative, including low molecular weight, bipolarity, and water solubility.19 Benzyl alcohol exhibits negligible binding to the surface of GP lenses, especially fluoro-silicone/acrylate (F-S/A) lens materials.18 In addition to its properties as a disinfectant, benzyl alcohol is effective in lipid removal.19
All commonly used preservatives in GP lens solutions appear to be safe and exhibit far fewer sensitivity reactions than soft lens disinfecting solutions. Certainly, it is possible for an occasional patient to exhibit a sensitivity reaction to any one of the aforementioned preservatives. This sensitivity is manifested, as with any allergic reaction, in the form of itching, burning, and redness. If this reaction occurs, it is often eliminated by switching to a care regimen using a different preservative.
Wetting Agents
Wetting/soaking solutions typically contain either polyvinyl alcohol or a methylcellulose derivative as a wetting agent.
Polyvinyl alcohol has several properties that make it a beneficial additive to GP lens solutions.2 It is water soluble and is relatively nonviscous and nontoxic to ocular tissues. It has good viscosity-building properties and exhibits good spreading and wettability on the eye and lens surfaces.20,21 Also, unlike methylcellulose, polyvinyl alcohol does not retard regeneration of corneal epithelium.22 Methylcellulose derivatives have been used successfully as wetting agents in more viscous GP solutions.
Cleaning
Several types of cleaners are available for use by GP lens wearers, including nonabrasive surfactants, abrasive surfactants, and surfactant soaking solutions, enzymes, and laboratory cleaners.
Nonabrasive Surfactants
GP cleaners and traditional hard lens cleaners may contain nonabrasive surfactant (detergent) cleaning agents to remove contaminants (e.g., mucoproteins, lipids, and debris) from the lens surface. The use of digital pressure or friction during the cleaning process is important in removing deposits from rigid lenses. Optimum Extra Strength Cleaner (Lobob Laboratories, Inc.) is an example of a nonabrasive surfactant lens cleaner.
Abrasive Surfactants
Abrasive particulate matter has been used in cleaners as an effective adjunct in removing adherent mucoproteinaceous deposits from the lens that may be resistant to use of the surfactant alone. The daily use of abrasive cleaning regimens has been demonstrated to be more effective than the use of nonabrasive cleaners.23 However, two problems have been described with abrasive cleaners. First, small surface scratches have been observed under high magnification.24 Second, inducing minus lens power while reducing center thickness can result.25,26,27 These problems have been minimized by the introduction of small-particle abrasive cleaners; however, abrasive lens cleaners may be contraindicated for lens materials with hyper-oxygen permeability (Dk) as well as for lens materials that have been plasma treated (discussed below). Examples include Boston Cleaner and Boston Advance Cleaner (Bausch & Lomb) and Opti-Free Daily Cleaner (Alcon Laboratories, Inc.).
Surfactant Soaking Solutions
GP lens care systems have traditionally embraced two-bottle regimens composed of separate cleaning and soaking solutions. One-bottle GP systems, combining these procedures, are a more recent innovation. These solutions use surfactant soaking, intended to dissolve deposits during the overnight soaking cycle; therefore, little digital pressure is necessary and warpage is less likely.28 Optimum Soaking Solution (Lobob Laboratories, Inc.) contains nonabrasive surfactants; it is used for both cleaning and disinfection. It should be rinsed before insertion to remove the benzyl alcohol and facilitate the mechanical removal of lens debris. Boston Simplus (Bausch & Lomb) and Unique pH (Alcon Laboratories, Inc.) are examples of multipurpose lens care products that do not require rinsing before insertion.
The lens care system should be prescribed for the needs of the patient. For example, Boston Original was formulated specifically for silicone/acrylate lens materials that are predisposed to protein deposition. Boston Advance Comfort Care was designed for fluoro-silicone/acrylate lens materials that are more likely to attract lipids. Multipurpose lens care systems may be most appropriate for patients who do not tend to deposit lenses or who are not compliant with twobottle lens care regimens. Patients who exhibit sensitivity to one formulation may be better served by a system using a different preservative.
Enzymes
The use of a weekly enzymatic cleaning regimen for GP lens wearers has been proven to be a beneficial adjunct to surfactant cleaning in protein removal from the lens surface.29 In addition, enzyme use has not been reported to cause any adverse effects for GP lens wearers.30
More recently developed protein removal products are in liquid, rather than tablet, form and may be used with the manufacturers’ accompanying storage solution. Boston One-Step Liquid Enzymatic Cleaner (Bausch & Lomb) is added to the storage solution weekly, whereas SupraClens (Alcon Laboratories, Inc.) is added to the storage solution daily. Both products should be rinsed before insertion. Boston One-Step is composed of subtilisin; SupraClens is a pancreatin derivative. Both products are designed to promote patient compliance and meet the patient’s desire for convenience.31,32
Laboratory Cleaners and Solvents
The use of laboratory-approved, extra-strength cleaners such as the Boston Lens Laboratory Cleaner (Polymer Technology Corporation) or Fluoro-Solve (Paragon Vision Sciences) can be beneficial. The Boston Lens Laboratory Cleaner, a solution consisting of several surfactants, can be beneficial for in-office cleaning of lenses that either exhibit poor initial wettability or have acquired a heavy film over time. However, surface debris that is more tenacious and difficult to remove, such as pitch or wax, can be removed only with Fluoro-Solve, which is a mild solvent.
MiraFlow (Ciba Vision), not approved for routine GP use, can be an excellent restorer of lens surface wetting. Since prolonged and repeated exposure to MiraFlow may result in permanent damage because of parameter changes,33 brittleness, and cracking caused by isopropyl alcohol,34 it should be used for no more than 30 seconds and then thoroughly rinsed off. Menicon PROGENT Intensive Protein remover is a further example of lens care products intended for professional in-office use. Available GP lens cleaners are listed in Table 6.3.
MiraFlow (Ciba Vision), not approved for routine GP use, can be an excellent restorer of lens surface wetting. Since prolonged and repeated exposure to MiraFlow may result in permanent damage because of parameter changes,33 brittleness, and cracking caused by isopropyl alcohol,34 it should be used for no more than 30 seconds and then thoroughly rinsed off. Menicon PROGENT Intensive Protein remover is a further example of lens care products intended for professional in-office use. Available GP lens cleaners are listed in Table 6.3.
TABLE 6.3 DAILY CLEANERS | ||||||||
|---|---|---|---|---|---|---|---|---|
|
Plasma Treatment
Plasma treatment for GP lenses removes residue from the manufacturing process and imparts an ultra-clean lens surface. This can enhance lens wettability and patient comfort and vision, particularly upon initial dispensing and early lens wear. Certain lens materials (Menicon Z) are routinely manufactured with plasma treatment, whereas other materials (Boston and Paragon) utilize plasma treatment at the discretion of the laboratory or practitioner.35
Rewetting and Relubricating
A solution that is used to rewet a GP lens surface while it is still on the eye should perform the following functions36:
Rewet the lens surface.
Stabilize the tear film.
Rinse away trapped debris.
Break up loosely attached deposits.
Ideally, this solution should clean the lenses of any debris while rewetting them for an extended period. Because the key to rewetting a GP lens is contact time, polyvinyl alcohol (PVA) often is added to increase the length of contact time. Some solutions contain hydroxyethylcellulose, methylcellulose, or other cellulose derivatives to aid surface wetting by increasing viscosity. Several rewetting solutions also contain a mild, nonionic detergent to loosen and solubilize mucus and debris and keep it from adhering tenaciously to the lens surface.36 Available rewetting/relubricating drops formulated specifically for GP lenses are listed in Table 6.4.
TABLE 6.4 WETTING AND LUBRICATION SOLUTIONS | ||||||
|---|---|---|---|---|---|---|
|
▪ DISPENSING VISIT
Procedures
Knowledge about the available care regimens and their respective functions, applications, and benefits becomes especially important at the dispensing visit. Before dispensing new lenses to a patient, it may be beneficial to apply fluorescein dye to the tear film to rule out any baseline staining with the biomicroscope. Once GP lenses have been inserted, an adaptation period is necessary before performing any test procedures. When the patient’s awareness has decreased and he or she is able to gaze in the straight-ahead position with minimal difficulty (a variable period, typically 10 to 45 minutes), visual acuity and lens evaluation can be performed. The use of a topical anesthetic immediately before initial lens application may result in the ability to assess both vision and the lens-to-cornea fitting relationship much more readily.
Visual Acuity
The patient’s vision should be assessed. Biomicroscopy should then be performed to evaluate lens position and surface wettability. If both good lens centration and surface wettability are present, an overrefraction can be performed to determine the necessary additional correction.
Overrefraction
If the visual acuity is equal to the expected value, typically a spherical over-refraction only is indicated. If a reduction of one line or greater is present, a spherocylindrical over-refraction should be performed. Just as the diagnostic fitting is imperative, both for obtaining a proper fit and for enhancing patient motivation (by the knowledge that contact lenses can be tolerated), so too is the dispensing visit important in continuing this momentum toward eventual patient success by the ability to see, handle, and care for the new GP lenses.
If an uncorrected cylinder that is not residual in nature is causing reduced visual acuity, overkeratometry should be performed to determine if the lens is flexing. If the keratometry readings are not spherical, flexure is present. This induced flexure can be minimized by selecting a flatter base curve radius (e.g., 0.50 D minimum) or increasing center thickness by a minimum of 0.02 mm.37
Slit-Lamp Biomicroscopy
The use of a biomicroscope is essential for evaluating lens centration, lag, fluorescein pattern, and surface wettability (although a Burton lamp would be a valuable adjunct for assessing fluorescein pattern). The lens-to-cornea fitting relationship initially should be evaluated using a wide beam with low-intensity white light and low magnification to scan the lens surface. In addition, the lens can be evaluated for regions of poor wettability or hazing. If the patient experiences variable visual acuity in combination with poor initial wettability, this problem can be minimized by presoaking the lenses for at least 24 hours to precondition the surface before insertion.
If poor wettability is present after presoaking the lenses, an in-office cleaner can be used or approved laboratory solvents should eliminate the problem. Polishing the front surface of the lens also may be beneficial; however, this should be performed after the lens is initially cleaned with an in-office cleaner and only if the lens has not been plasma treated.
Comprehensive evaluation of the fluorescein pattern is also important. Is the pattern similar to that observed at the diagnostic fitting visit? The use of high illumination, low magnification, and a moderate-to-wide beam width with cobalt filter should be beneficial when observation is by biomicroscope. If there is difficulty in observing the pattern, a Wratten no. 12 or similar filter can be used, especially if the lens material contains an ultraviolet inhibitor. In addition, if lower magnification is necessary to evaluate the pattern accurately, or to view both eyes simultaneously, a Burton lamp can be used.
Patient Education
Handling
The key to teaching patients to handle GP lenses successfully is reassurance. No matter how frustrating it is to the person performing the instruction, that feeling of frustration must not be conveyed to the patient. The instructions must be provided slowly and one at a time. Performing group instruction is distracting and denies the patient the necessary one-on-one personal instruction. The patient should not have the perception that the eye care provider or assistants have lost confidence in the patient’s ability to learn how to handle the lenses properly; otherwise, feelings of failure and surrender may result, possibly leading to the attitude that contact lenses will never be worn again. Conversely, if the patient feels confident about handling the lenses, a perception of satisfaction and success is often present. A minimum of three successful insertions and removals is recommended, although the number depends on how confident the patient feels. If it takes two or three visits (closely spaced to maximize memory of techniques and to minimize further anxiety) for the patient to master lens handling, it is often worth the effort. This is more often a problem with presbyopic patients, who not only are experiencing blurred vision at near, but also may have lived 40 or more years without having a foreign body placed on their eye, thereby increasing anxiety.
Patients should be instructed to insert and remove the lenses over a cloth or paper towel spread on a table (not over a sink drain). In addition, patients should be asked and reminded to avoid oily substances such as hand creams, lotions, or cosmetics, and their hands should be washed and rinsed thoroughly prior to handling the lenses. It is important for both practitioner and staff members to set a good example by washing hands before handling lenses in the office and requiring patients to do likewise.
Insertion by the Patient:
Insertion of lenses by the patient is a three-step procedure.
Positioning.
The patient should be encouraged to use an adjustable mirror when inserting the lenses. This will help to ensure that the lens is positioned properly on the finger and to view the position of the lens; the latter is especially important because patients may consistently bring the lens in contact with the upper or lower lid.
Lid Retraction:
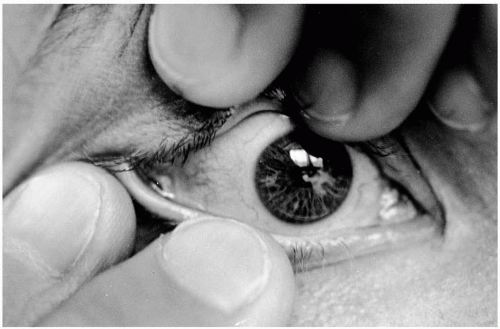
For the right eye, the lens should be placed on the right index finger. The middle finger of the left hand should be placed over the upper lashes to lift up the upper lid. The middle finger of the right hand should be placed directly over the lower lashes to depress the lower lid (Fig. 6.1). The ability to retract the lashes successfully is essential.
Placement:
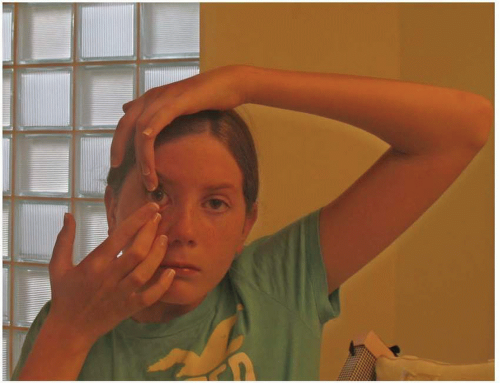
The patient should be looking straight ahead (Fig. 6.2), typically at a mirror on a table or counter. Often, the new rigid lens patient will experience difficulty maintaining proper fixation as the lens approaches the eye; therefore, it is important to assure the patient that the lens will not damage the eye. Finally, once the lens has made contact with the eye, the patient should be instructed first to release the finger holding the lens, then the lower lid, and finally the upper lid. This procedure then can be performed in reverse for the other eye (i.e., use the index finger of the left hand for holding the lens, the middle finger of the right hand for holding the upper lid, and the middle finger of the left hand for holding the lower lid).
Insertion by the Practitioner or Assistant:
The procedure is similar if performed by an office member. If the lens is to be placed on the right eye, the lens will be placed on the index finger of the right hand, with the left middle finger holding the upper lid and the right middle finger holding the lower lid (Fig. 6.3). Because the patient may become especially apprehensive with someone else inserting the lens, it is very important to apply pressure underneath the lashes to ensure that they will not move during this process. In this case, the patient can be instructed to view a distant target, for example, a letter on the acuity chart.
Removal by the Patient:
There are at least three methods of removing a GP lens. Which method is used depends on such factors as lid tension, lens design, and personal preference.
The easiest method is to use the index finger of the same hand as the eye from which the lens is to be removed to eject the lens. The finger is placed at the junction of the lateral edge of the lids (Fig. 6.4). With the eye opened wide, the lids are pulled laterally; at the same time, the patient blinks and the lens should be ejected. This procedure can be performed with both the middle and index fingers of the same hand to enhance the possibility of lens ejection. The other hand can be positioned underneath the eye to catch the lens if it fails to adhere to the lower eyelashes. For patients who experience difficulty with the first method because of such factors as loose lid tension, low edge lift, and large overall lens diameter, a more forceful method to remove the lens is to use both hands. The middle and index fingers of the same hand are positioned over the lower lid; the middle and index fingers of the opposite hand hold up the upper lid. As with the first method, the lids are pulled laterally and, while the patient blinks, the lens is ejected (Fig. 6.5A-C). As with all methods of removal, the most important factor is allowing the lid margins to eject the lens. Figure 6.6 shows that if the lids are not retracted properly (i.e., if the finger is not placed over the lashes), the lid can evert and, therefore, apply very little pressure toward ejecting the lens.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree