Chapter 39 Lateral Neck Dissection
Indications
The controversy in the management of patients with differentiated thyroid cancer has shifted in recent years from the extent of surgery in the thyroid (i.e., thyroid lobectomy versus total thyroidectomy) to the initial management of the regional lymph nodes and, more specifically, to the management of the lymph nodes in the central compartment of the neck (see Chapters 37, Central Neck Dissection: Indications, and 38, Central Neck Dissection: Technique). Even though consensus guidelines are now widely available, this area continues to be debated because prospective randomized studies do not exist and are not likely to be conducted because of the prolonged period of follow-up needed to obtain valid results in patients with differentiated thyroid cancers. Furthermore, the impact of lymph node metastases on survival is still being elucidated. Also, the utility of adjuvant treatment with radioactive iodine in low-risk patients is not clearly delineated. Thus, in this chapter, we address the current controversies in the management of the neck in patients with differentiated thyroid cancer and describe the best evidence available in the literature that supports the different points of view.
Lymphatic Drainage of the Thyroid Gland
The lymphatics of the thyroid gland are divided into three groups (Figure 39-1; see also Chapter 38, Central Neck Dissection: Technique, Figure 38-1). The lymphatics emerging from the inferior-medial aspect of the thyroid lobes follow the course of the inferior thyroid veins and drain to the primary echelon nodes in the pretracheal, paratracheal (level VI), and lower jugular regions (level IV). They drain secondarily into the nodes of the anterior-superior mediastinum (level VII) and rarely into lower mediastinal nodes. The lymphatics emerging from the lateral aspect of the gland follow the middle thyroid vein and drain into the jugular lymph nodes (levels II, III, and IV). The lymphatics from the superior aspect of the gland and the isthmus drain into the prelaryngeal (Delphian) and jugular lymph nodes, particularly to the midjugular nodes (level III).
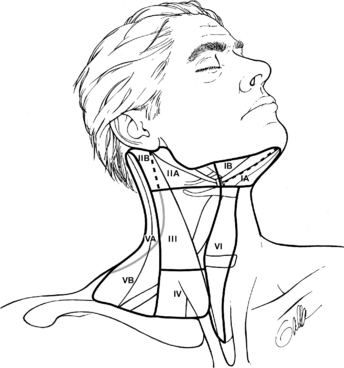
Figure 39-1 Lymphatic drainage regions of the neck.
(From Janfaza P, et al, editors: Surgical anatomy of the head and neck, Philadelphia, 2001, Lippincott Williams & Wilkins.)
This seemingly orderly lymphatic drainage would lead one to think that the pattern of lymphatic spread of carcinomas could be predicted based on the location of the primary tumor within the thyroid. Surprisingly this question was not systematically addressed until recently, when Mirallie et al.,1 studying retrospectively 119 patients with papillary carcinoma of the thyroid who were treated with total thyroidectomy and bilateral modified radical neck dissection, did not find a correlation between the site of the lymph node metastases in the neck and the localization of the primary tumor within the thyroid. However, these authors found that lymph node metastases were significantly less frequent for tumors originating in the lower pole of the thyroid lobes than for tumors of other localizations. It is also interesting that only one of their patients with a tumor in the lower third of the thyroid lobe had metastases in the subdigastric nodes; this patient had paratracheal and midjugular lymph node metastases as well. This observation suggests that level II nodes may not be at high risk of containing metastases in patients whose tumor originates in the lower pole of the thyroid lobe. Clearly there is variability and a lack of predictability in the exact distribution of nodal metastasis for thyroid cancer.
The Patterns of Lymph Node Metastases
Lymph node metastases from thyroid carcinoma tend to occur first in the paratracheal nodes regardless of the location of the primary within the thyroid gland.2,3 A sentinel lymph node from the thyroid can be detected in the paratracheal region in 88% of the patients.4 Although it is safe to consider levels VI (i.e., central neck nodes) and VII (i.e., upper mediastinal) lymph nodes as the primary echelon of drainage for all thyroid cancers, skip metastases to the nodes of the lateral compartment of the neck can occur in as many as 18% of the patients.5 Regarding the jugular chain of lymph nodes, as noted previously, no correlation seems to exist between the site of the primary lesion within the thyroid gland and the location of the lymph node metastases.2
Metastases in the jugular chain of lymph nodes involve most commonly level IV jugular lymph nodes (52%) followed in frequency by levels III, V, and II (45%, 33%, and 30%, respectively).6 Involvement of lymph nodes in the submandibular triangle (level I) is uncommon, occurring mainly with advanced disease and when nodes at other levels of the neck, particularly at level II, are involved.7,8
Contralateral lymph node metastases occur in as many as 24% of the patients, particularly in those patients with large tumors, that involve the isthmus, or with recurrent tumors.2,9 For primary tumors localized to one lobe of the thyroid, the risk of contralateral metastases is low especially for small tumors. In a recent study, only 1 of 57 patients with unilateral thyroid carcinoma less than 1 cm in diameter had metastases to the contralateral paratracheal lymph nodes.10 Intrathyroid spread to the contralateral side, as suggested by Attie,11 is not commonly observed.
In a recent study, Mirallie et al.1 mapped the lymph node groups most frequently involved in papillary carcinoma of the thyroid, in order to determine which nodes could be sampled to guide the decision to perform a neck dissection and to define the extent of the neck dissection. They studied retrospectively 119 patients with papillary carcinoma of the thyroid treated by total thyroidectomy and bilateral modified radical dissection. As expected, 51% of the patients had metastases in the nodes of the central compartment of the neck (level VI), and 47% had involvement of lateral compartment nodes (levels II, III, and IV or a combination). Interestingly, however, of the patients who had histologically proved lymph node metastases overall, 20% had no metastases in the paratracheal nodes, 37% had no metastases in the midjugular nodes, and 49% had no metastases in the supraclavicular lymph nodes. Furthermore, 13% of patients with normal midjugular and paratracheal nodes and 14% with normal supraclavicular and paratracheal nodes had metastases in other lymph nodes in the neck. Others have previously reported an absence of metastases in the paratracheal nodes in 9% to 10% of patients with otherwise pathologically positive neck nodes.12,13 These observations indicate that the presence or absence of metastases in the paratracheal, midjugular, or supraclavicular nodes does not accurately predict the presence or absence of metastases in other lymph nodes of the neck and brings into question the reliability of “sampling” these nodes in deciding when to perform a neck dissection.
Risk Factors for Lymph Node Metastases
Histologic Subtype
Papillary carcinoma is associated with the highest propensity for lymph node metastases. The overall incidence averages 60% but ranges between 30% and 90%.2,5,14–21 The incidence is even higher in children, in whom it averages 80%.6,22–24 A palpable lymph node metastasis is the first clinical manifestation of a thyroid carcinoma in 13% to 30% of all patients25–27 and in 20% of patients with a papillary microcarcinoma of the thyroid.15 The incidence of subclinical lymph node from papillary carcinoma ranges between 44% and 82%.8,16,28–30 The follicular variant of papillary carcinoma is associated with a lower risk of lymph node metastases than the pure papillary variant; in one series, the reported incidence of lymph node metastases was 22% and 57%, respectively (see Chapters 18, Papillary Thyroid Cancer, and 19, Papillary Thyroid Microcarcinoma).31 Follicular carcinoma has a propensity for hematogenous spread and a lower risk (12% to 14%) of lymph node metastases (see Chapter 20, Follicular Thyroid Cancer).32–35 It has been reported that Hurthle cell carcinoma, a subtype of follicular carcinoma, was associated with lymph node metastases in as many as 50% of the cases36; however, recent reports suggest that the rates of nodal metastases are similar to those associated with pure follicular carcinomas (see Chapter 22, Hurthle Cell Tumors of the Thyroid)20,21,37
The tall-cell variant (TCV) of papillary thyroid carcinoma is considered a more aggressive variant of papillary carcinoma, with a poor prognosis. Interestingly, however, using the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) database, Morris et al. did a match-pair analysis of 278 patients with tall cell variant and 2522 with classical papillary carcinoma. They found that the frequency of lymph node metastases was similar for both histologic types (39.6% and 36.5%).38
Tumor Size
In a retrospective study of 335 patients with papillary microcarcinoma who underwent total thyroidectomy or lobectomy with elective central lymph node dissection, Lee et al. found that tumor size (>5 mm), male sex, age (<45), and extrathyroidal extension were predictive factors for lymph node metastases.39 Other reports also describe a direct correlation between tumor size and the risk of nodal metastases.40,41
Tumor Invasion Characteristics
Tumors that exhibit extrathyroidal extension, vascular invasion, or have no capsule around them are prone for lymph node metastases. Male sex may be another factor that is correlated with aggressive tumor invasion. In two separate studies when male patients had tumors that exhibited both extrathyroidal extension and vascular invasion, their risk of nodal metastases was much higher (87%) than in patients without these risk factors (37%).29,39
Biologic Marker
At the present time, no biologic markers have been validated sufficiently to be used routinely as a means of predicting, preoperatively, the presence of lymph node metastases in patients with differentiated thyroid carcinoma. However, the BRAF gene mutation is the most intriguing marker as a potential predictor of the presence of lymph node metastases and of prognosis in patients with papillary thyroid cancer. Several studies have established a strong association between the presence of BRAF mutation and a higher rate of lymph node metastasis, as well as other clinicopathologic characteristics of papillary thyroid carcinomas, including extrathyroidal extension, advanced disease stage, and persistence and recurrence of tumor.42,43 Xing et al. investigated the utility of preoperative testing for the BRAF mutation on fine-needle aspiration biopsy specimens in predicting the extent of the tumor and subsequent clinical outcomes. In comparison with the wild-type allele, the presence of BRAF mutation was a better predictor of lymph node metastasis (38% versus 18%; p = 0.002), extrathyroidal extension (23% versus 11%; p = 0.039), and thyroid capsular invasion (29% versus 16%; p = 0.045). It should be noted that in this study, central compartment dissection was performed “mainly” for grossly enlarged lymph nodes. Consequently, the extent of the association of BRAF mutation with lymph node metastasis was probably underestimated. These observations suggest that preoperative knowledge of BRAF mutation status may be useful in selecting patients that may benefit from elective central compartment dissection (see Chapters 37, Central Neck Dissection: Indications, and 38, Central Neck Dissection: Technique).44 Rodolico et al. observed recently that patients with papillary thyroid carcinoma of 1 cm in diameter or less, in whom the tumor cells metastatic to the lymph nodes harbor the BRAFV600 mutation and exhibit down-regulation of protein p27Kip1, had larger metastatic deposits, more involved lymph nodes, and more frequent extracapsular extension than patients without these mutations. However, they found no difference in regard to the neck compartment involved (central versus lateral).45 The association of BRAF mutations and other genetic events appears to be a better predictor of a poor outcome.46
Expression of suppressor gene p53 appears to correlate with the “aggressiveness” of papillary carcinoma.47,48 Morita et al. recently found a significant correlation between the overexpression of p53 protein and large tumor size, the presence of lymph node metastasis, and the mean number of lymph node metastases.49 Papillary carcinomas harboring the RAS mutation almost always have the follicular variant histology; this mutation also correlates with more frequent encapsulation and lower rate of lymph node metastases.50,51
Correlation between RET/PTC rearrangement and prognosis in human papillary carcinomas remains unclear. Some evidence suggests that the RET/PTC1 rearrangement type is associated with more favorable behavior.52
The Prognostic Significance of Lymph Node Metastases
The impact of lymph node metastases on the prognosis of patients with differentiated thyroid cancer is now better understood. In the past, some studies had suggested that lymph node metastases are not associated with a decreased survival in patients with papillary thyroid carcinoma.5,14,24,27,41,53–59 Some studies even suggested a survival benefit in patients with nodal metastases.27,32,60 However, in some of these studies the results were not adjusted according to the age of the patients. Furthermore, in most of these studies the length of follow-up may have been inadequate. Harness et al.56 emphasized the need for prolonged follow-up on patients with differentiated thyroid cancer to get accurate survival statistics. Mazzaferri and Jhiang61 studied 1355 patients with papillary and follicular cancer followed for 10 to 30 years. They found that survival was significantly decreased in patients with lymph node metastases. Some of the deaths from cancer in their series occurred 20 to 30 years after treatment, emphasizing again the importance of a prolonged follow-up period. More recently, Podnos et al.62 reported a study of the SEER database. In a cohort of 9904 patients with papillary thyroid carcinoma, lymph node metastases, age > 45 years, distant metastasis, and large tumor size were significant predictors of poor outcome on multivariate analysis. Survival at 14 years was 79% for patients with lymph node metastases and 82% for patients without them (p < 0.05). In a more recent study of the SEER database, Zaydfudim et al.63 concluded that cervical lymph node metastases are independently associated with decreased survival, but only in patients with follicular cancer and in patients with papillary cancer older than 45 years. Other studies have shown that the rate of regional recurrence is higher in patients with lymph node metastases, especially in those patients with metastases in multiple lymph nodes or extracapsular extension of tumor.64
The Management of the N0 Neck
The Lateral Compartment of the Neck
Elective dissection of the lateral compartment of the neck is not indicated in patients with differentiated thyroid cancer because there seems to be no survival benefit with such practice.65–67 It should be noted, however, that some surgeons, especially in Japan, recommend elective treatment to the lateral compartment of the neck (levels II to V) for every patient with papillary carcinoma of the thyroid or for high-risk patients only.5,6,30,68–70
The Central Compartment of the Neck
The role of elective dissection of the lymph nodes in the central compartment of the neck is the main controversy in the surgical management of differentiated carcinoma of the thyroid today (see Chapters 37, Central Neck Dissection: Indications, and 38, Central Neck Dissection: Technique).71 The most recent guidelines published by the American Thyroid Association72 state that prophylactic central-compartment neck dissection (ipsilateral or bilateral) may be performed in patients with papillary thyroid carcinoma with clinically uninvolved central neck lymph nodes, especially for advanced primary tumors (T3 or T4). In terms of supporting evidence, this recommendation is based on “expert opinion” and is qualified by the statement that it “should be interpreted in the light of available surgical expertise,” acknowledging that the rate of complications associated with this operation can be higher when the surgeon is inexperienced or does the operation only sporadically. The European Thyroid Cancer Taskforce consensus in 2006 was that “There is no evidence that it [i.e., central compartment dissection] improves recurrence or mortality rates, but it permits an accurate staging of the disease that may guide subsequent treatment and follow-up.”73
These recommendations are noncommittal because of the lack of prospective, randomized data that show a beneficial effect of central compartment dissection on recurrence or disease-specific survival in patients with differentiated thyroid carcinoma. However, a number of retrospective studies and case series suggest a beneficial effect. What is considered by some to be the best available evidence in support of elective central compartment dissections is the study by Tisell et al.,74 which has been described as a prospective study. The study is, in fact, a retrospective analysis of what appears to have been a standardized clinical practice. The authors reviewed a series of 195 consecutive patients operated on for papillary thyroid cancer at Sahlgrenska University Hospital in Göteborg from 1970 through 1989. Surgeons in the endocrine surgery unit operated on all patients, and their strategy was to perform a total or near total thyroidectomy and a “careful central neck dissection” between the internal jugular veins from the level of the hyoid bone down to the innominate vessels. Only 12 patients (6%) were treated with radioiodine postoperatively, either because of distant metastases (4 patients) or for ablation of a thyroid remnant (8 patients). The median follow up was 13 years, and it ranged between 0.2 and 26 years. Eight patients died of thyroid cancer (4%); 5 of these patients had distant metastases at the time of initial diagnosis (stage IV), and the other 3 (1.6%) had stage III disease. The mortality rate of 1.6% observed in patients without distant metastases is remarkable. The authors went on to compare their results with those of two other Scandinavian studies published recently, one from Finland75 and one from Norway.76 Central compartment dissection was not routinely performed in the patients included in those studies. The authors indicate that the comparison is appropriate because the living conditions and health care systems are similar in the three Scandinavian countries. The mortality rate of 1.6% compares favorably with the 11.1% and 8.4% rates observed in the studies from Finland and Norway, respectively. The authors conclude that their results strongly suggest that careful microdissection of the thyroid and the central lymph nodes can improve survival in patients with papillary thyroid cancer. However, the appropriateness of the studies selected for comparison can be called into question because the cohorts studied were not comparable in terms of tumor stage and postoperative treatment. More importantly, in one of the comparison studies, no information is provided about management of the lymph nodes and in the other the prevailing practice was a “berry picking” procedure.
In addition to this study, two recent systematic reviews of the literature indicate that four retrospective studies and at least seven case series also suggest that elective dissection of the central compartment may decrease recurrence and improve disease-specific survival in patients with papillary thyroid carcinoma.77,78 However, the controversy in this area remains because similar, retrospective, observational studies have not found such beneficial effect.79
1. Metastases in the lymph nodes of the central compartment of the neck cannot be identified reliably by preoperative ultrasonography (US) or by visual inspection of the nodes intraoperatively. Evaluation of the paratracheal nodes by ultrasonography is hampered by the presence of the thyroid gland. Several studies have shown that US identifies about half of the lymph nodes identified through elective dissection of the central compartment.80,81 It has also been shown that fewer than 50% of lymph nodes in the central compartment that have pathologically proved metastases are correctly judged by the surgeon during the operation.82
2. Elective dissection of the nodes in the central compartment can improve accuracy in staging and decreases postoperative thyroglobulin levels. Sywak et al. reviewed retrospectively 447 patients with papillary thyroid carcinoma and clinically negative nodes using thyroglobulin measurements during follow-up as a marker of persistent disease.83 Fifty-six patients underwent total thyroidectomy plus ipsilateral central compartment dissection, and 391 patients had total thyroidectomy alone. Both groups had equivalent tumor sizes and MACIS scores, and both groups were treated with radioactive iodine, with the mean dose being similar in the two groups. Postablation serum levels of thyroglobulin were lower in the group undergoing central compartment dissection (p = 0.02), and more patients in this group had undetectable thyroglobulin levels (p < 0.001). More recently, Bonnet et al.84 studied 115 patients with small papillary thyroid carcinomas who had negative preoperative neck ultrasound examinations (T1N0) and were treated with total thyroidectomy and bilateral central compartment (level VI) dissection. The authors reported that elective lymph node dissection modified the indication for radioiodine ablation in 30% of the patients. Furthermore, 1 year after treatment, 97% of the patients had undetectable levels of serum thyroglobulin during thyroid-stimulating hormone (TSH) suppression or with recombinant human TSH (rhTSH) stimulation.
3. Removal of the nodes in the central compartment in high-risk patients, who are likely to harbor metastases that would eventually grow, prevents subsequent surgery in a previously operated, scarred area, which may jeopardize the recurrent laryngeal nerve.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


