, Yasuya Nomura2 and Yasuya Nomura3
(1)
The Society for Promotion of International Oto-Rhino-Laryngology, Tokyo, Japan
(2)
The University of Tokyo, Tokyo, Japan
(3)
Showa University, Tokyo, Japan
Abstract
Laser can be used as a tool for inner ear surgery, particularly for the treatment of intractable vertigo. We found that argon laser selectively destroyed the maculae of the otolithic organs without injuring the wall of the membranous labyrinth, except for the dark cell area. The area of the maculae of the otolithic organs can be seen through the oval window after stapedectomy. The utricular macula is seen as a white plaque high in the vestibule. The recommended lasing site is the center of the plaque, or near its base, because nerve fibers and blood vessels enter the macula through the base. As for the human saccular macula, the saccular wall in the elderly contains many lipofuscin granules in its endothelial cell layer. Therefore, when lasing the saccular macula, sieve-like small perforations result in the saccular wall. These perforations may greatly influence the function of the cochlea.
Heat produced by laser irradiation of the semicircular canal can constrict the semicircular duct. This procedure does not require opening the canal for irradiation. Blue-lining the semicircular canal near the semicircular duct is essential. Because the duct adheres to the periosteum at the outer circumference of the canal, the blue line in this area is the best site to irradiate. This procedure is useful when attempting to immobilize the endolymph, such as for patients with intractable benign paroxysmal positional vertigo.
Laser surgery will eventually replace vestibular neurectomy. Its surgical field is within the scope of conventional ear surgery.
Keywords
Argon laserInner earSaccular maculaSemicircular canalSemicircular ductSurgeryUtricular maculaVertigo7.1 Introduction
Applications of laser as a treatment modality for inner ear disease have a long history. As early as 1965, Stahle and Högberg [1] irradiated the semicircular canals of pigeons using a Q-switched pulsed ruby laser and found a marked fibrotic reaction within the irradiated canal. The pigeons showed signs of labyrinthine irritation immediately after the procedure. Since then, the inner ear has been the subject of research aimed at developing laser surgery techniques [2–4].
In 1991, Anthony [5] reported lasing a pigment-marked blue-lined area of the posterior semicircular canal in two patients with benign paroxysmal positional vertigo (BPPV), and called this occlusion of the semicircular canal “partitioning.” The lasing attempted to immobilize the endolymph of the posterior semicircular canal. Later, Anthony [6] thought that BPPV could be resolved by eliminating the otoliths from the utricle. Accordingly, the target organs for laser treatment have extended from the semicircular canals to the otolithic organ.
Among the various kinds of lasers, argon laser has been selected chiefly because it passes through the membranous vestibular labyrinth safely and selectively damages the sensory epithelium.
In this series of studies, the following two argon laser systems were used:
1.
Coherent Medical Group Laser apparatus was incorporated in a Zeiss OMP1 operating microscope, spot size 100 μm
2.
HGM Medical Laser System, Inc. ME-648, hand probe type, spot size 200 μm
Argon laser is a visible wavelength laser that has a range from 488 to 514.5 nm. The intensity of the argon laser in water falls to 1/10 its original surface value at a depth of 920 cm (penetration depth).
7.2 Animal Experiments
7.2.1 The Cochlea
7.2.1.1 Laser Irradiation of/Through the Round Window Membrane
Namba and Nomura [7] irradiated the round window membrane of guinea pigs (Takei strain) with an argon laser after pentobarbital anesthesia. The probe had an outer diameter of 600 μm, in which a glass fiber 200 μm in diameter was encased. One watt of power was applied for 0.5 s. The tip of the probe was approximated to the round window membrane about 1 mm from the target.
The irradiated round window membrane showed no microscopic changes. No burned spot or perforation was observed after application of the argon laser (Fig. 7.1). However, various changes were found within the cochlea. When the organ of Corti was irradiated, an area 300 μm in diameter completely disappeared, with formation of three slits in the basilar membrane. The direction of the slits was the same, parallel to the fibers of the basilar membrane. It seemed that the slits occurred secondary to micro-explosion of the organ of Corti. The basilar membrane itself seemed to permit passage of the argon laser beam (Fig. 7.2).
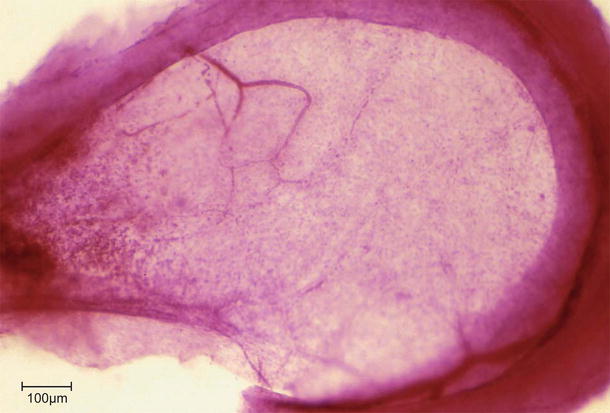
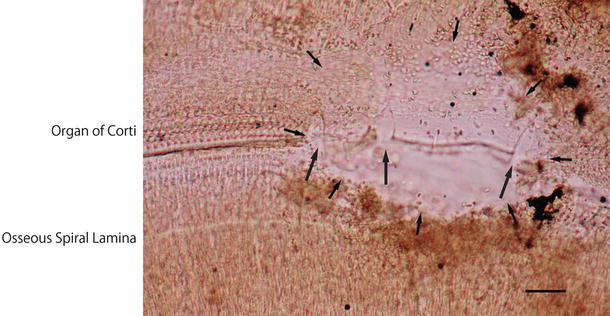
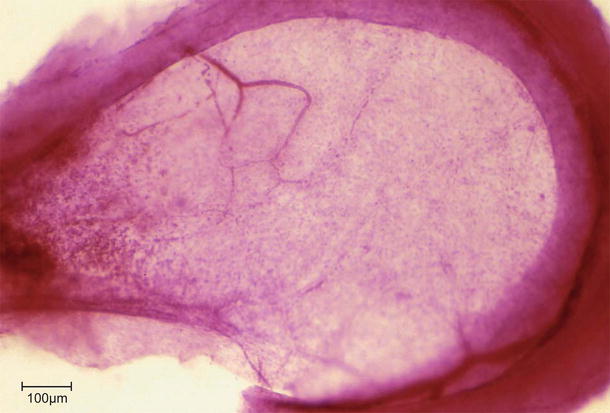
Fig. 7.1
The intact round window membrane after argon laser irradiation. Power 1.0 W × 0.5 s × 3 times. Beam diameter was 200 μm. Guinea pig, Kernechtrot staining, scale: 100 μm
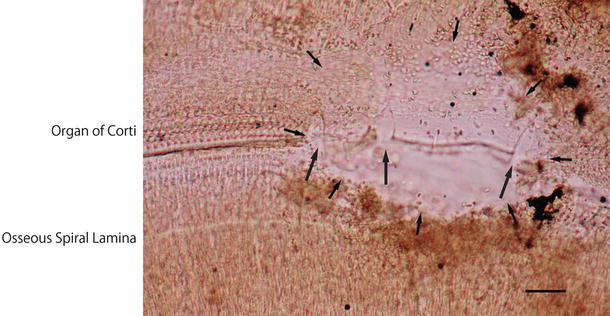
Fig. 7.2
Destruction of the organ of Corti immediately after irradiation [7]. Power 1.0 W × 0.5 s. An area 300 μm in diameter disappeared (arrows). Three splits are found in the basilar membrane (large arrows). Scale: 50 μm
When the osseous spiral lamina of the basal turn was lased, the irradiated area was destroyed and the associated venule vaporized and coagulated, resulting in congestion of its periphery (Fig. 7.3). In another specimen, partial loss of the lower shelf of the osseous spiral lamina and loss of nerve fibers were seen on cross section. The upper shelf of the osseous spiral lamina was partly fractured and elevated. The limbus spiralis, tectorial membrane, and organ of Corti had degenerated (Fig. 7.4). Cyst formation in the stria vascularis was observed 2 days after irradiation. Because anatomy prevents direct access to the stria vascularis through the round window membrane, cyst formation might be a secondary effect. Though the secondary spiral lamina appeared intact, the adjacent lower spiral ligament was widely destroyed (Fig. 7.5) [8]. The basilar membrane showed a break. Claudius’ cells near the break were lifted and attached to Reissner’s membrane. The round window membrane remained intact (Fig. 7.6).
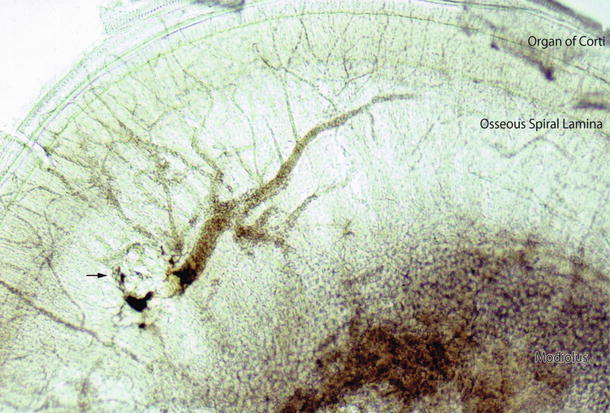
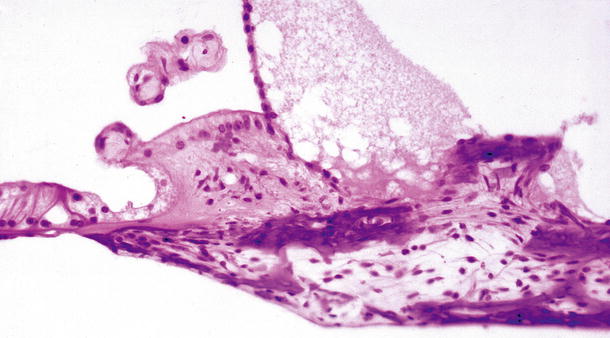
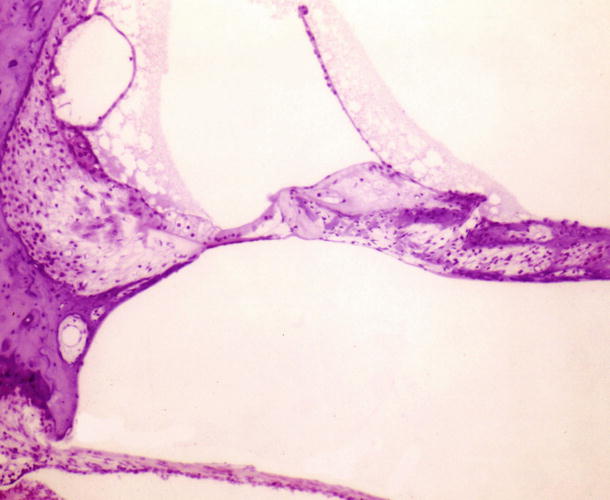
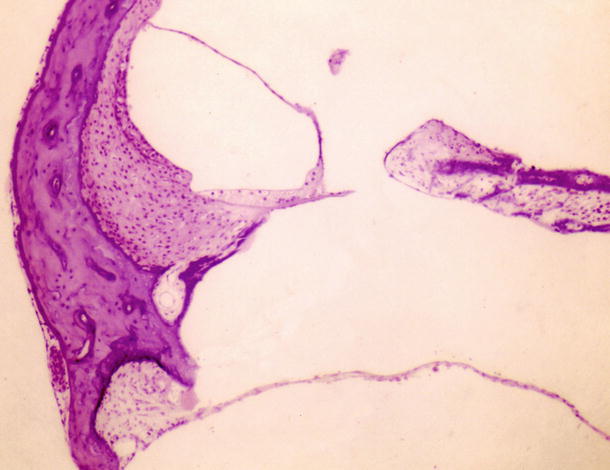
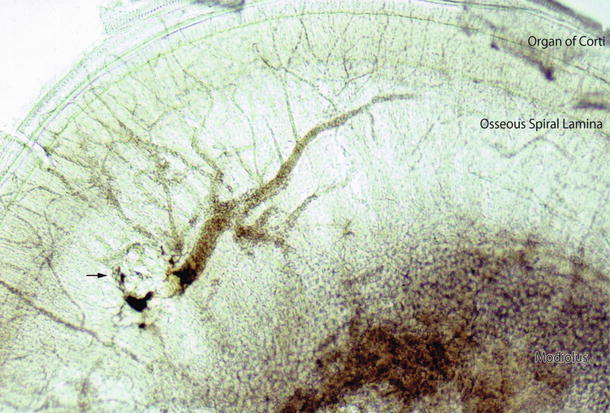
Fig. 7.3
Irradiation of the osseous spiral lamina through the round window membrane. The arrow indicates circular damage to the osseous spiral lamina. The venule running near the center of the explosion was involved, resulting in destruction and coagulation of the vessel. Its periphery is congested. Immediately after irradiation. The same animal whose intact round window membrane is shown in Fig. 7.1. Surface preparation, Nomarski microscope
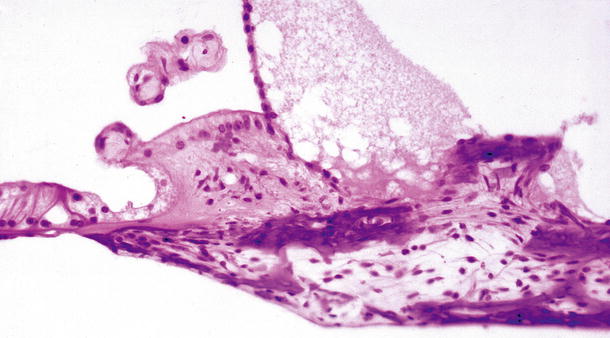
Fig. 7.4
Laser irradiation of the osseous spiral lamina through the round window membrane. There is loss of dendrites of the cochlear neurons in the osseous spiral lamina. A defect in the lower shelf and fracture of the upper shelf of the spiral lamina are seen. Partial loss of the interdental cells and degeneration of the tectorial membrane are evident. The organ of Corti and the internal sulcus cells have degenerated. Two days after irradiation (1 W × 0.5 s) (original ×16) [7]
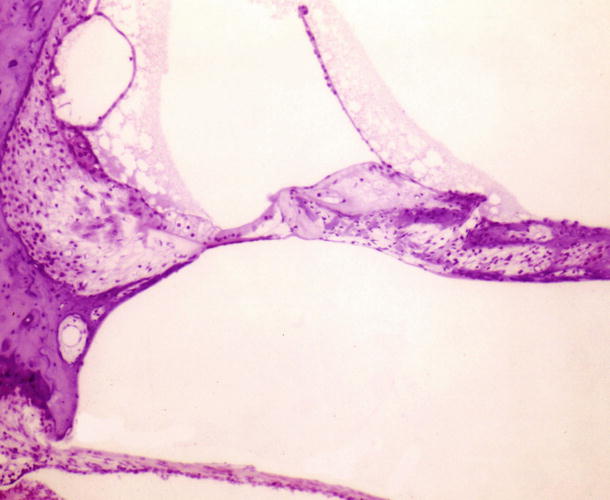
Fig. 7.5
Laser irradiation of the cochlea through the round window membrane. Laser beams hit the basilar membrane and the osseous spiral lamina, resulting in marked damage. A cyst has formed in the stria vascularis. The secondary spiral lamina appears intact but the adjacent lower spiral lamina is destroyed. Two days after irradiation (1 W × 0.5 s × 5 times) (original ×6.5) [8]
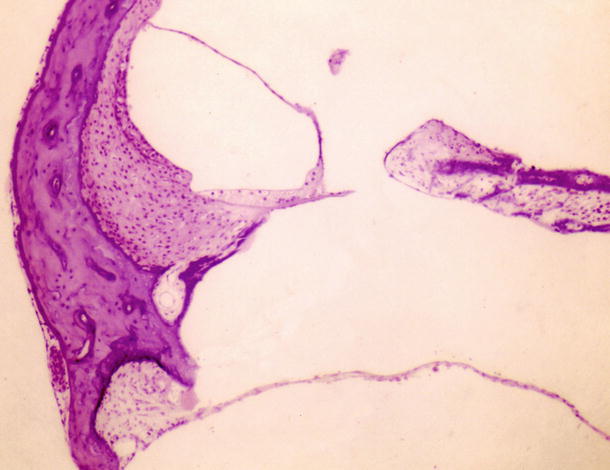
Fig. 7.6
Laser irradiation of the cochlea through the round window membrane. Laser beams hit the basilar membrane and the osseous spiral lamina, resulting in communication between the scalae tympani and vestibuli. Claudius’ cells close the scala media together with Reissner’s membrane (original ×6.5) [8]
7.2.1.2 Laser Irradiation of the Otic Capsule
The purpose of argon laser application to the bony wall of the cochlea is to produce localized loss or atrophy of the stria vascularis. In another study, the tip of the probe (diameter 200 μm) was advanced toward the otic capsule of the third cochlear turn, about 1 mm from the bony surface. The target was the stria vascularis [8].
The stria vascularis with spiral ligament was removed immediately after laser irradiation (800 mW × 0.5 s) of the otic capsule of the third turn. Alkaline phosphatase staining was performed to confirm the effect of lasing on the strial capillary network. A circular coagulated area was found in the stria vascularis within which the strial capillaries showed no enzymatic activity (Fig. 7.7).
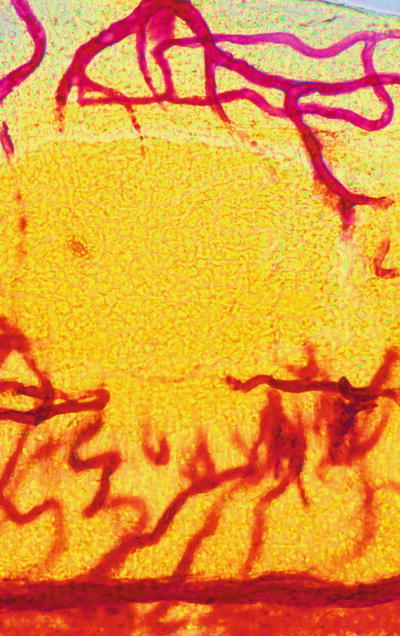
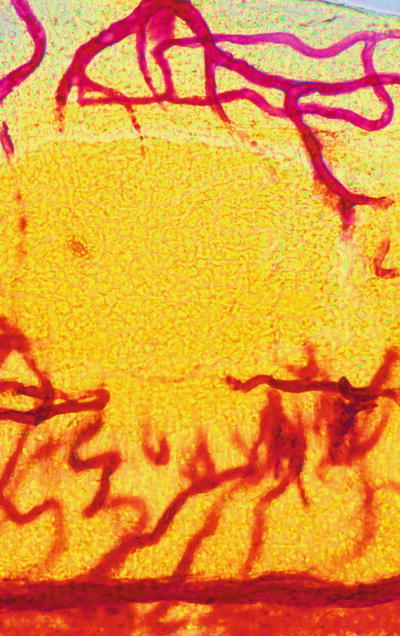
Fig. 7.7
Laser irradiation of the stria vascularis through the otic capsule of the third turn. The strial capillary in the coagulated area (about 300 μm in diameter) shows no alkaline phosphatase activity (0.8 W × 0.5 s). Guinea pig, alkaline phosphatase staining [8]
A similar experiment was conducted using reduced laser power of 300 mW applied to the otic capsule [7]. This produced a charred area with an adjacent vaporized area in the capsule. The irradiated area showed a slight bulge covered by intact periosteum (Fig. 7.8). Strands connecting the remaining living tissues passed through the charred and lucent area. The strands may have been capillary remnants. Reissner’s membrane appeared to have extended to cover the defect of the stria vascularis and spiral ligament. It is not clear whether the altered marginal cells of the stria vascularis participated in this process (Fig. 7.8). In another specimen, altered marginal cells remained and connected to Reissner’s membrane. Several days later, cellular debris had cleared from the perilymphatic space, as well as from the scala media (Fig. 7.9).
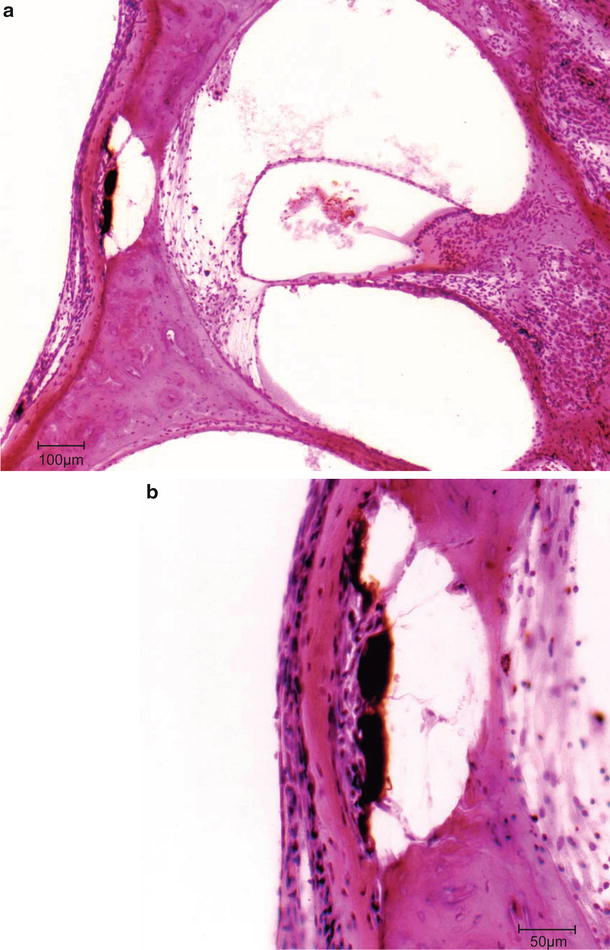

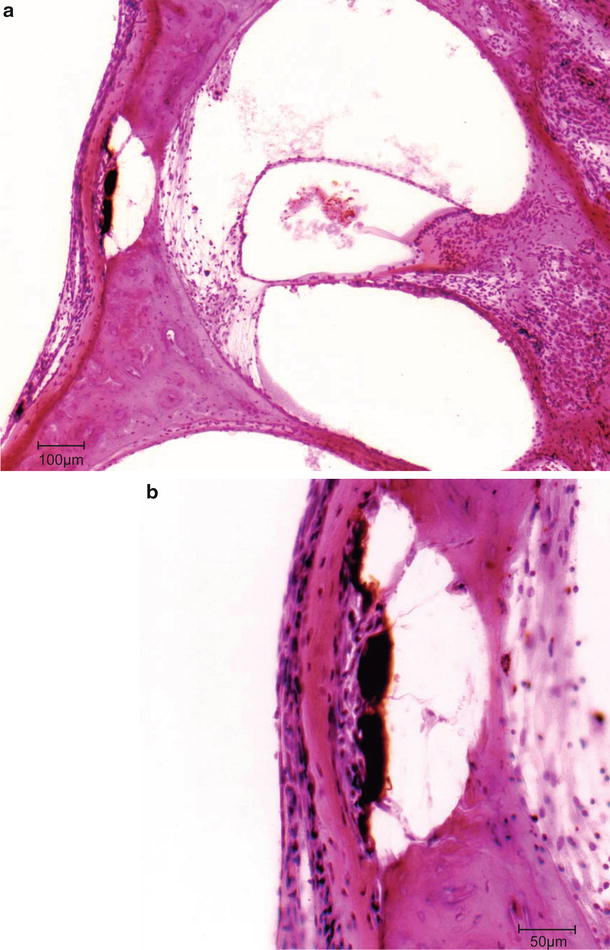
Fig. 7.8
Changes of the otic capsule and inside the cochlea [7]. (a) A carbonized area is present beneath the normal periosteum, which shows a bulge. Adjacent to the carbonized area is a vaporized region. The spiral ligament is defective and the stria vascularis is absent. The organ of Corti has been completely destroyed and has detached from the basilar membrane. Fifteen days after irradiation of the otic capsule adjacent to stria vascularis. The scala media is smaller but its boundary is preserved. Scale: 100 μm (original ×6.5). (b) Higher magnification of the section of (a). The power applied was 300 mW × 0.5 s. The second turn of the cochlea of a guinea pig, 15 days after irradiation (original ×16), scale: 50 μm

Fig. 7.9
More advanced stage. Irradiation of the otic capsule. In addition to loss of the stria vascularis, loss of the spiral ligament extends toward its lower portion. Dendrite loss in the osseous spiral lamina is more marked than that observed in Fig. 7.8. Twenty-six days after irradiation of 300 mW × 0.5 s (original ×16) [7]
Thirty-five days after laser irradiation (90 mW × 0.5 s), the stria vascularis was completely absent but the configuration of the scala media was preserved. The upper half of the spiral ligament was almost completely missing. The inner and outer hair cells had degenerated. Hensen’s cells appeared preserved. No cellular debris remained in the scala media (Fig. 7.10).
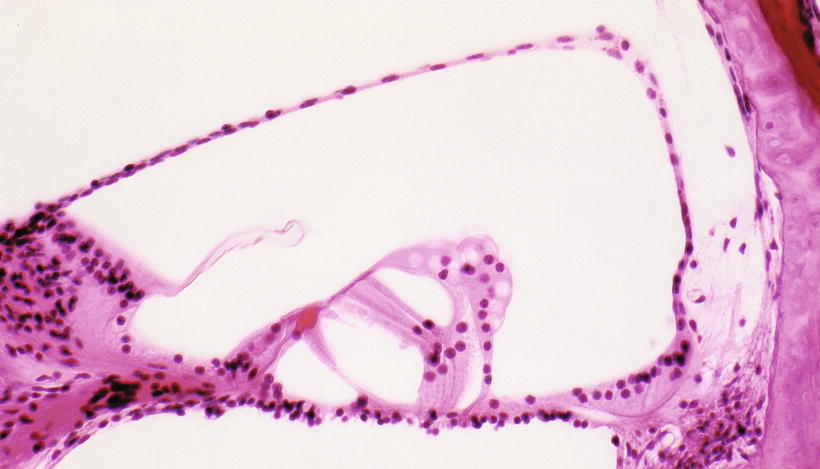
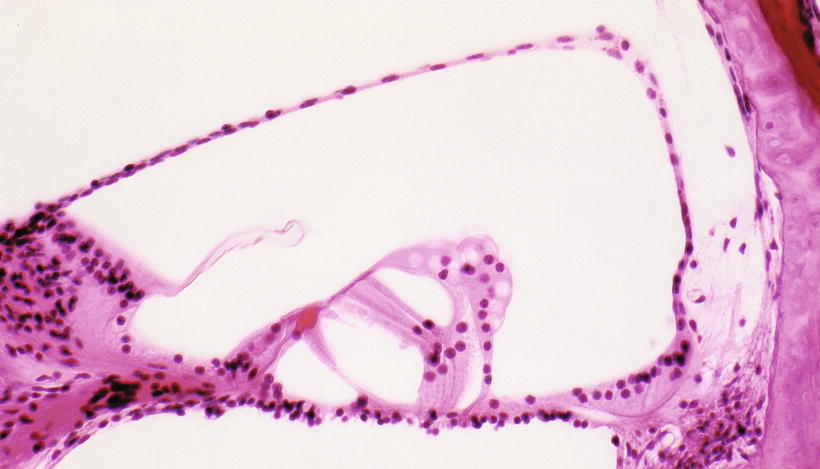
Fig. 7.10
Complete loss of the stria vascularis and near loss of the spiral ligament. The outer hair cells are elongated with shrunken nuclei. Reissner’s membrane extends to cover the lost stria vascularis and spiral ligament. The endolymphatic compartment is preserved. Hensen’s cells are fairly well preserved. 35 days after irradiation of the otic capsule (90 mW × 0.5 s). Guinea pig (original ×16) [7]
The otic capsule did not show any changes after laser irradiation (50 mW × 0.5 s). However, the spiral ligament was atrophic and acellular behind the stria vascularis, which persisted as a single layer of altered marginal cells. The outer hair cells were atrophic and some lacked nuclei. The outer hair cells and the phalanx of Deiters’ cells appeared to have fused. Hensen’s cell appeared unchanged 30 days after laser application (Fig. 7.11).


Fig. 7.11
Free floating, disintegrated strial cells in the scala media (large arrow). There is fusion of the anuclear atrophic hair cells with the phalanx of Deiters’ cells (small arrow). The stria vascularis and spiral ligament are atrophic. Thirty days after argon laser irradiation of the otic capsule (50 mW × 0.5 s). Third turn of the cochlea, guinea pig (original ×16) [7]
The average thickness of the otic capsule of the third turn was 102 μm (mean of 12 animals) and the capsule did not show morphologic changes. This suggests that the laser beam passed through the bony wall and led to destruction of the spiral ligament and disappearance of the stria vascularis. However, the primary goal of inducing localized strial atrophy was unsuccessful. The laser power needed to be reduced to preserve an intact organ of Corti.
Using the photochemical reaction between the systemic injection of Rose Bengal and controlled green light irradiation of the cochlea, Ocho et al. [9] produced a localized degeneration of the stria vascularis with preservation of the outer hair cells. The photochemical reaction produced a reactive oxygen species, resulting in damage to the endothelium. This damage triggered platelet adhesion and aggregation at the site of endothelial injury, producing thrombi and affecting microcirculation in the lateral wall of the cochlea at the site of irradiation. The direction of irradiation was tangential to the target in the cochlear wall. The outer hair cells survived for 24 h after irradiation, then disappeared with loss of the stria vascularis [9, 10].
7.2.2 The Otolithic Organs
7.2.2.1 Laser Irradiation of the Utricular Macula
The utricular macula is located on the floor of the utricle and its area can be seen through the oval window as a white plaque in the upper portion of the vestibule.
An argon laser passes through the utricular wall without damaging it, except in the dark cell area. Melanin in the dark cell area is susceptible to the beam, resulting in perforation [11]. Irradiation of the macular area is safe, because the connective tissue layer beneath the sensory epithelium is relatively thick and almost no pigments or pigment cells exist there.
When irradiating the utricular macula of guinea pigs, stapedectomy should be performed carefully to allow replacement of the stapes in the oval window after irradiation.
A single irradiation with an argon laser (1–1.5 W for 0.5–1 s) is enough to erase the entire sensory area, including the otoliths, sensory epithelium, nerve fibers, and capillary networks. The beam is directed toward the center of the white plaque (Fig. 7.12) [11].
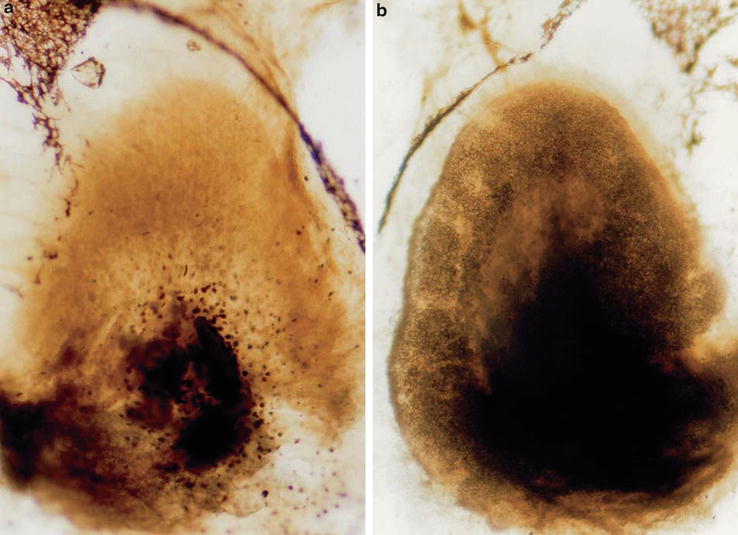
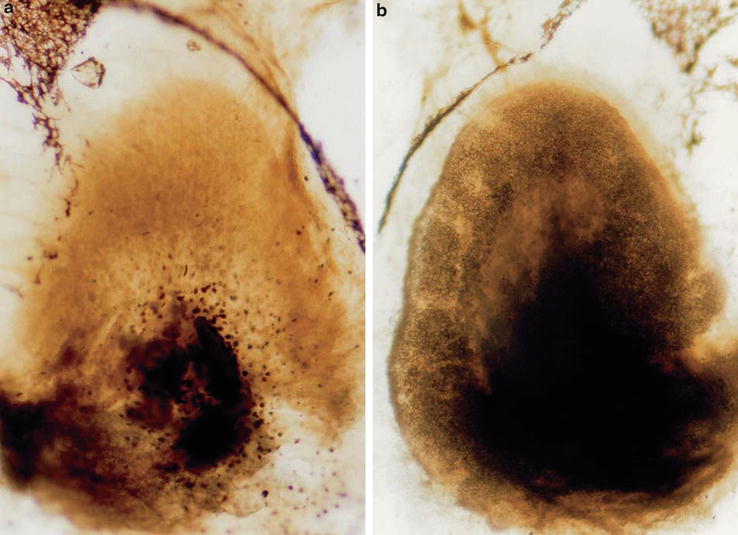
Fig. 7.12
Irradiation of the utricular macula [13]. (a) Complete loss of nerve fibers, sensory epithelium, and otoliths. Nineteen days after a single irradiation of 1.5 W × 0.5 s. (b) Control: The otoliths and dark-stained nerve fibers can be seen. Guinea pig, osmic acid staining, whole mount staining (original ×6.5)
Histological changes seen in the utricular macula differ depending on the power and duration of irradiation, and the interval between irradiation and sacrifice. The sensory cells and supporting cells are most vulnerable to irradiation.
Histological Changes 10 Weeks After Argon Laser Irradiation of the Utricular Macula (1 W x 1 s)
Complete loss of the macula was observed with preservation of the utricular wall, saccular wall, and membrana limitans. The utricle showed a mild hydrops (Fig. 7.13) [12]. The nerve fibers underneath the sensory epithelium were also missing. The crista of the lateral semicircular canal remained intact (Fig. 7.14) [11]. Caloric testing response had returned to normal.
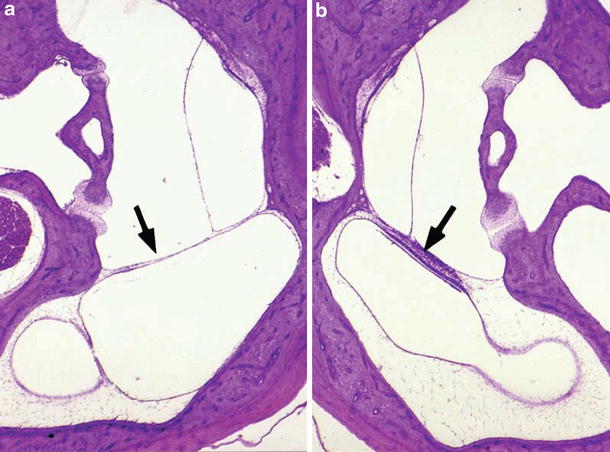
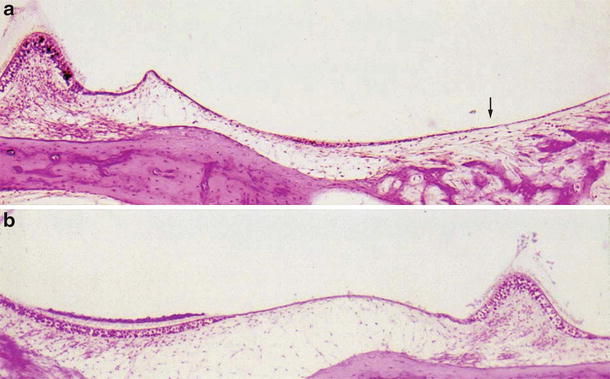
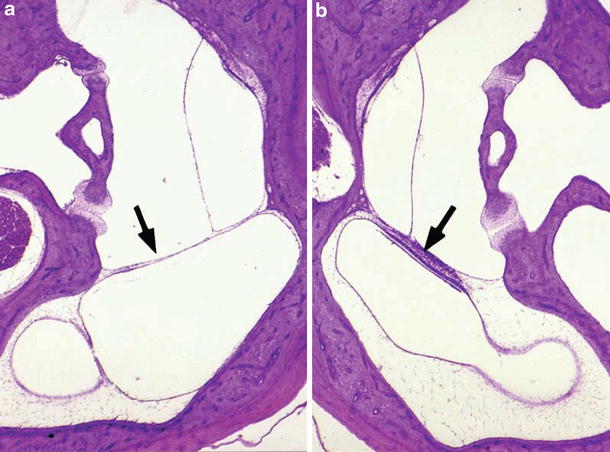
Fig. 7.13
Irradiation of the utricular macula 10 weeks after irradiation [12]. (a) After stapedectomy, the utricular macula was irradiated by argon laser (1 W × 1 s). The stapes was replaced in the oval window after irradiation. The utricular macula has completely disappeared (arrow). Mild hydrops is seen in the utricle and semicircular duct. (b) Control: A cross section of normal utricular macula (arrow) is observed. Guinea pig, HE staining (original ×2.5)
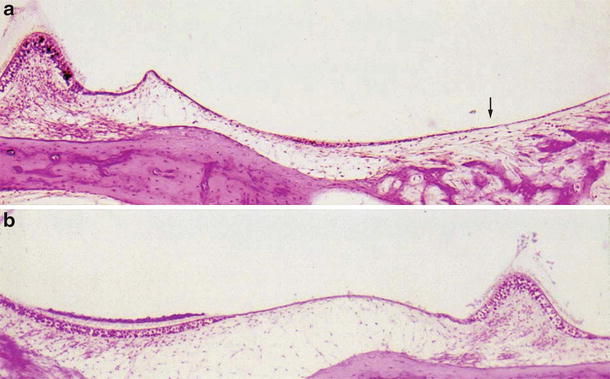
Fig. 7.14
Irradiation of the utricular macula [11]. (a) The utricular macula with nerve fibers is completely missing 10 weeks after irradiation (1 W × 0.5 s) (arrow). The subepithelial connective tissue is thin compared with the normal side. The crista ampullaris of the lateral canal lies on the same plane as the utricle. (b) Control: The utricular macula shows normal structure: otolithic membrane, sensory epithelium, and nerve fibers. Guinea pig (original ×6.5)
Immediately after irradiation, the supporting cells were partly missing and partly remained on the basement membrane as destroyed cells with pyknotic nuclei. The sensory cells were destroyed and elevated. The top surface of the sensory epithelium appeared undulated. There were clear spaces between the sensory cells and the basement membrane and/or remnants of the supporting cells. The basement membrane did not show any clear rupture under light microscopy (Fig. 7.15) [13]. Capillaries beneath the basement membrane were intact. When viewed with electron microscopy, nerve fibers in the subepithelial connective tissue layer showed marked distortion of their myelin sheaths with loss of neurofilaments.
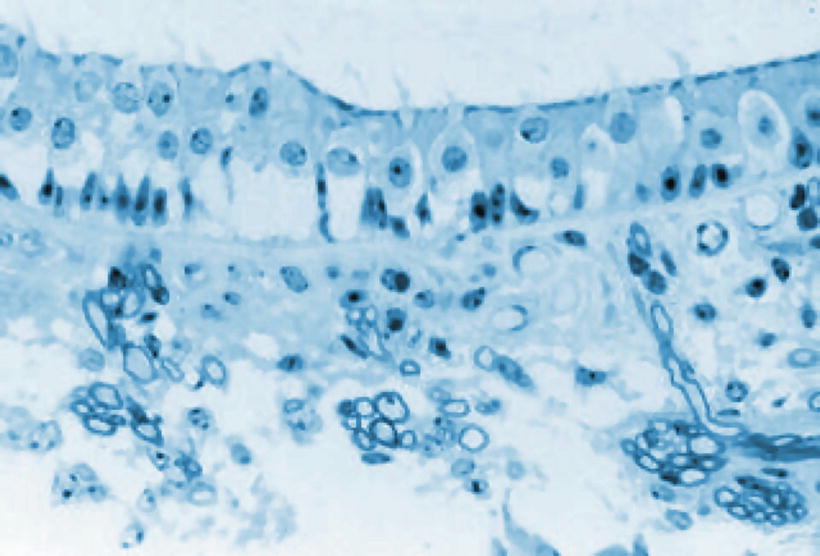
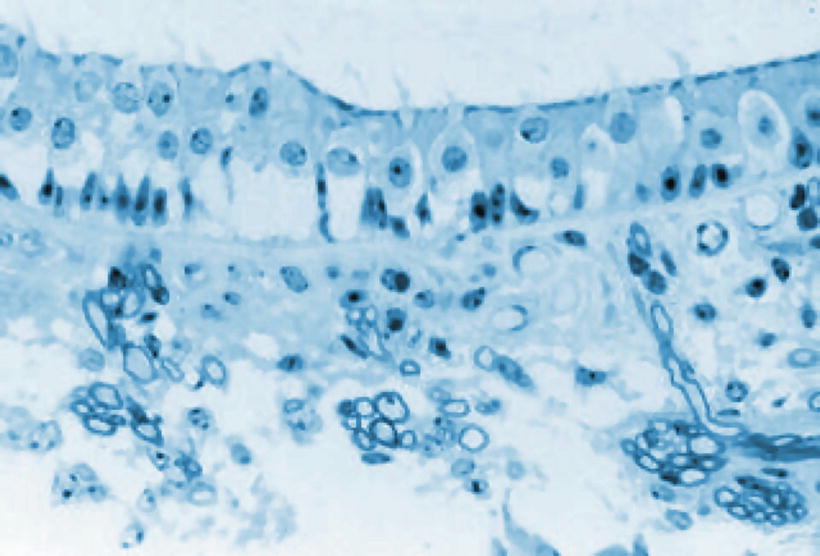
Fig. 7.15




The utricular macula immediately after irradiation. Sensory cells are destroyed and detached. There is marked loss of supporting cells. A lucent area is present between the basement membrane and the sensory cells. Myelinated nerve fibers in the subepithelial connective tissue show degenerated myelin sheaths and rare neurofilaments under an electron microscope. Guinea pig, toluidine blue staining (original ×40) [13]
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


