10
Laboratory Tests of Vestibular and Balance Functioning
Judith A. White
Laboratory vestibular testing includes a battery of quantitative tests that can be selected to provide assessment of the oculomotor system, caloric responses, positional and positioning nystagmus, vestibulo-ocular reflex (VOR) gain, phase and symmetry, vestibular-visual interaction, and postural control. Each test in the appropriately chosen test battery will add independent information to the assessment.
 Clinical Utility of Vestibular Testing
Clinical Utility of Vestibular Testing
First it is important to consider which clinical questions laboratory vestibular testing can answer. Vestibular testing can identify a vestibular deficit and provide information to localize the lesion. This is appropriate when the diagnosis remains uncertain after the history and office physical examination of the dizzy patient (see Chapter 14) are completed. Laboratory vestibular testing is not a substitute for an accurate, thorough history. It should not replace the basic office physical examination of the dizzy patient, including spontaneous, gaze, positional, and positioning testing; head thrust and head shake testing; and office oculomotor assessment, including pursuit and saccade. For example, it would not be necessary to obtain laboratory vestibular testing when simple posterior semicircular canal benign paroxysmal positional vertigo is noted on office Dix-Hallpike testing.
Vestibular assessment can also be used to follow vestibular deficits over time. This is because the testing not only identifies a vestibular deficit, such as a caloric weakness in one ear, but also provides valuable information regarding the degree of compensation present to that deficit. Compensation is a central process that recalibrates the vestibular system after an acute unilateral vestibular loss. During the initial period following an acute unilateral vestibular loss, there may be spontaneous nystagmus beating away from the affected ear, positional and positioning nystagmus similarly beating away from the affected side, and a weakness of VOR gain when the patient rotates to the side of loss. Postural control may be abnormal when visual and proprioceptive cues are minimized.
After vestibular compensation to an acute unilateral vestibular loss, the vestibular assessment pattern changes. The caloric loss may remain, but spontaneous, positional, and gaze-evoked nystagmus disappear. Rotary chair VOR gain normalizes, and VOR asymmetry resolves. Postural control normalizes. The only persistent signs of a long-standing compensated vestibular loss may be VOR phase elevations and the caloric asymmetry. This information is useful in assessing response to vestibular rehabilitation. Following successful vestibular rehabilitation, the resolution of VOR asymmetry can be followed objectively using rotary chair testing (see Chapter 32). Similarly, the significance of an isolated caloric asymmetry identified during caloric testing can be determined by looking for associated indicators of an uncompensated versus compensated unilateral loss.
Vestibular testing is an important consideration prior to ablative vestibular procedures or surgery. Ensuring normal function on the unaffected side avoids inadvertently ablating the only functioning vestibular system. Preoperative vestibular testing may also help predict the course of recovery after procedures such as vestibular nerve section, intratympanic gentamicin, or acoustic neuroma resection. A robust response in the affected ear would predict significant vertigo after surgical ablation, similar to a bout of vestibular neuritis. A weak response suggests that some degree of chronic loss and compensation may have previously occurred, and predicts a more rapid recovery.
In summary, vestibular testing can identify and help localize vestibular lesions, and assess the degree of compensation present to these lesions. It is appropriate after a history and office physical examination leave the diagnosis in question, when initial treatment does not result in expected benefit, and prior to vestibular ablative surgical procedures.
 Limitations of Vestibular Testing
Limitations of Vestibular Testing
Vestibular testing has several limitations. It does not measure disability from vestibular deficits. Patients with similar test results may have widely varying functional capacity. Factors such as the demands of the workplace and environment, response to illness, concurrent medical problems, and psychosocial resources affect the degree of disability a patient may experience from a vestibular deficit.
An additional limitation of standard vestibular testing is that it does not assess the vertical canals or otolith function. Head-shake testing, the Halmagyi-Curthoys head thrust, caloric testing, and rotary-chair testing all assess the lateral (horizontal) canal and by extension the superior division of the vestibular nerve. Head-thrust testing in vertical canal planes can be performed, but may be uncomfortable for the patient because twisting of the neck is required at a high velocity and should only be performed by someone familiar with the technique. Most clinical vestibular laboratories limit assessment of the vertical canals to Dix-Hallpike positioning.
 Indications and Patient Preparation for Vestibular Testing
Indications and Patient Preparation for Vestibular Testing
Vestibular testing begins with patient preparation. Typically, patients referred for testing have suffered from some type of dizziness or vertigo, and the prospect that testing will reproduce this symptom is daunting. Patient cooperation with test instructions, including concentration, is vital in obtaining accurate data. Psychological factors strongly affect test performance, and patients who are too anxious, preoccupied, or fatigued cannot perform the required tasks. Patients are prepared for the test with simple, clear instructions, and advised to get a good night’s rest before the test. Reassurance, encouragement, and support during testing are very helpful. Patients are required to refrain from antihistamines, alcohol, sedatives, and benzodiazepines 24 to 48 hours prior to testing (exceptions for benzodiazepines are sometimes made for chronic low-dose use when discontinuation presents significant problems, but this compromises test accuracy). Other medications may also affect test sensitivity (notably antiepileptics, which should not be discontinued), and interpretation should note all medications taken and include their possible effects on the test results.
Vestibular test data quality is human operator dependent. The patient’s frequent eye blinks, eye closure, poor concentration, and less than optimal performance may make vestibular test data useless, or inaccurately suggest oculomotor deficits, failure of fixation suppression, or other “central” findings. Computerized interpretation systems cannot replace the role of the experienced human operator in obtaining optimal, cooperative performance from patients, which yields valid and reliable data.
As computerized interpretation systems become faster, more accurate, and more sensitive, our tendency may be to only examine the computer screen graphics, or the printed results. However, each of the clinical interpretation systems in common usage analyzes eye movements in the x-y (horizontal and vertical) plane. These systems are sensitive to horizontal and vertical eye movements, whether sensed by skin electrodes or infrared video image analysis. Torsional eye movements are not accurately analyzed by commonly used computerized systems because torsion of the pupil is not accurately sensed in either a horizontal or vertical plane. We find it very useful to record the nystagmus seen during positional and positioning testing and replay and review it during interpretation. Various recording methods seem to work well, including VCR, DVD, and hard drive digital recording. The most important teaching point in our vestibular laboratory is to look at the eye movement during positional and positioning testing, not the computer graphics.
The order of testing is planned to allow the patient to perform easier tests first. Computerized dynamic posturography may be performed first. Oculomotor and rotary chair testing is usually performed prior to positional and positioning testing. Caloric testing, usually the most unpleasant of the tests because it provokes brief vertigo, is performed last.
 Types of Vestibular Testing
Types of Vestibular Testing
Oculomotor Testing
Oculomotor testing consists of pursuit, saccade, spontaneous, gaze-evoked, and optokinetic nystagmus. The reader is directed to Leigh and Zee1 for an excellent reference on the neurology of eye movements. Eye movements are assessed first in the vestibular test battery, to identify abnormalities and also to ensure that nystagmus can be recorded accurately during later vestibular stimulation. The presence of strabismus and poor vision should be noted and considered in test interpretation.
Calibration is performed by having the patient look at fixed points 1 m away, including center, left (27 cm), and right (27 cm). These lateral points correspond to approximately 15 degrees of eccentric gaze. Calibration is important for computerized interpretation systems because inaccurate calibration will affect measurement of the amplitude and direction of nystagmus throughout testing. Calibration errors are the most common reason caloric responses appear “reversed.”
Nystagmus refers to rhythmic repetitive eye movements. The term is derived from the Greek expression used to describe the involuntary head nodding seen during napping while sitting up. Nystagmus may be visual or central in origin, and is commonly seen in individuals with congenital blindness. Vestibular nystagmus is specifically characterized by a slow and fast phase. The eyes deviate slowly to one direction and jerk rapidly back (fast phase). By convention, the direction of the nystagmus is named for the direction of the fast phase. The strength of the nystagmus is calculated by measuring the degrees that the eye moves in 1 second during the slow phase.
Vestibular test interpretation is greatly facilitated for beginners by recognizing the conventions used in strip recording. A line tracing of nystagmus will usually have time along the horizontal axis and eye deviation along the vertical axis. Looking at the strip recording from left to right shows the eye movement as time progressed in the testing (similar to electrocardiogram strips). An upward deflection of the line on the horizontal recording strip corresponds to a rightward eye movement (UP-RIGHT), and a downward deflection corresponds to a leftward eye movement. The vertical strip (if used) is easier to interpret because upward eye movement is also an upward deflection of the line, and a downward eye movement is a downward deflection of the line.
Nystagmus can be recorded by several methods. Visual inspection in room light is the least sensitive. Patients who can see objects visually fixate on them, and this reduces vestibular nystagmus by at least 50%. Electro-oculography (EOG) uses surface skin electrodes around the eye to record changes in the strength of the field generated by the corneo-retinal potential, and nystagmus is recorded in the dark or with eyes closed. EOG resolution is 1 degree and recording bandwidth is narrow (35 Hz), but electrical and muscle interference decreases sensitivity. Infrared video-oculography (IR-VOG) uses infrared recording cameras placed in goggles in front of the eyes, which must be kept open for the examination. Most clinical vestibular image analysis systems use the differing infrared reflectance of the sclera versus the iris to analyze eye movement. Resolution is high (0.1 degree) but bandwidth is limited by present recording speed technology and currently exceeds 100 Hz. This limitation does not usually affect the accuracy of clinical vestibular testing, but more advanced infrared systems are available at a considerably higher cost for research applications. The most complex technique, using magnetic search coils placed on the sclera, has very high resolution (0.02 degrees), high recording speed, and the advantage of torsional nystagmus recording. However, magnetic search coils are expensive and uncomfortable, with recording times limited to 30 minutes.
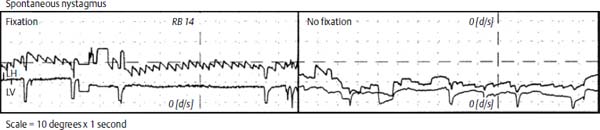
Figure 10–1 Rightward nystagmus (seen during fixation testing only)—a central finding.
Spontaneous nystagmus is recorded with the patient sitting comfortably, and is recorded with and without visual fixation. Usually a small light located inside the infrared goggle is illuminated for fixation testing. The most common pattern of vestibular nystagmus is a persistent horizontal unidirectional nystagmus that diminishes at least 50% with fixation. It may be stronger when patients direct their gaze in the direction of the fast phase (Alexander’s law). It is usually seen in the acute period following a unilateral vestibular loss, and the fast phase beats away from the affected ear.
Spontaneous nystagmus that does not have these important characteristics (unidirectional, horizontal, diminishes with fixation, and worsens with gaze in the direction of the fast phase) should be considered potentially central. This includes vertical nystagmus (upbeat or downbeat), direction-changing nystagmus, irregular or disconjugate nystagmus, or nystagmus that worsens with fixation. Alcohol and anticonvulsants may cause atypical nystagmus.
A rightward spontaneous nystagmus is seen in Fig. 10–1. The fast phase of the nystagmus beats rightward (upward on a horizontal channel strip recording). The nystagmus is recorded only during fixation and disappears without fixation. This is a central finding because the nystagmus is worse with fixation. Another central spontaneous nystagmus is shown in Fig. 10–2. It beats leftward with fixation and rightward without fixation. This nystagmus is direction-changing.
Nystagmus is tested next in eccentric gaze. Fifteen to 30 degrees of eccentric gaze is sufficient; more may provoke a physiologic end-gaze nystagmus seen in many normal patients. Rightward, leftward, upward, and downward gaze are assessed. Unidirectional horizontal nystagmus may sometimes be seen when gazing away from the side of an acute vestibular loss, and other features of acute uncompensated vestibular loss are evident when this occurs (such as caloric weakness and VOR asymmetry). However, most other types of gaze-evoked nystagmus, such as direction-changing nystagmus, are considered a sign of central pathology. Anticonvulsants and alcohol may cause gaze-evoked nystagmus. Fig. 10–3 shows a central gaze-evoked rightward nystagmus in right gaze (worse with fixation in this example, which is another central sign). Gaze-evoked nystagmus may be so severe that it interferes with the patient’s ability to visually follow a moving object. Fig. 10–4 shows right gaze-evoked nystagmus interfering with smooth pursuit tracking.
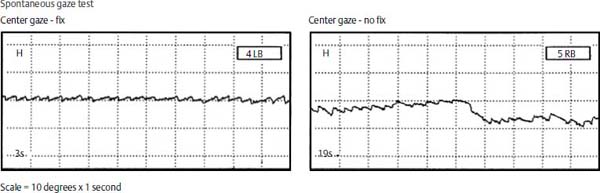
Figure 10–2 Direction-changing nystagmus that beats leftward in center gaze with fixation and rightward in center gaze without fixation—a central finding.
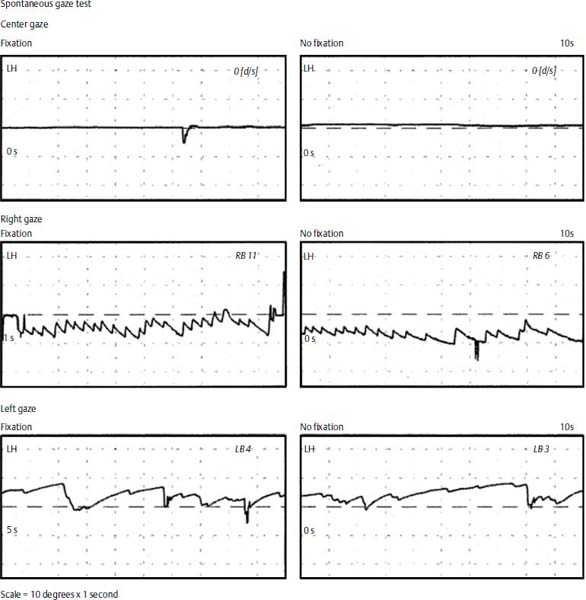
Figure 10–3 Gaze-evoked nystagmus.
Saccades are extremely high acceleration (30,000 deg/sec2) eye movements with a 200-ms latency and a 50- to 100-ms duration. They are used to volitionally redirect sight, or reflexively gaze toward a startling stimulus. Saccades are so fast that vision is obscured during the eye movement. Three features of saccades are usually assessed in vestibular testing: latency (delay between the presentation of the stimulus and beginning of the saccade, usually approximately 200 ms); accuracy; and peak velocity (norms vary with ocular displacement and are displayed on a special graph, ranging from 50 to 700 degrees/s). Saccades that are hypometric undershoot and fail to reach the target. Hypometria must be severe and reproducible to be considered abnormal. Hypermetric saccades overshoot the target, and are more significant even if slightly abnormal.
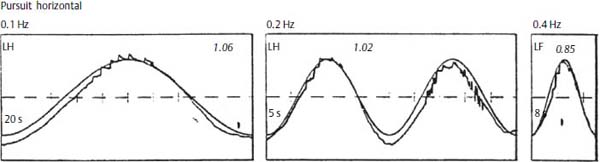
Figure 10–4 Gaze-evoked nystagmus affecting right smooth pursuit.
Saccades are frequently noted to have bilateral mildly prolonged latency and mild hypometria in older, less alert, or poorly compliant patients. Drugs may affect saccades symmetrically (both leftward and rightward). Care should be taken not to attribute a central pathology in those situations. However, any asymmetric saccade abnormality is considered significant. Internuclear ophthalmoplegia (INO) is a central disorder that causes slowed or absent adduction (inward movement toward the nose) of the affected eye during conjugate eye movements, such as saccades or pursuit. It may be seen in both eyes in bilateral INO. It is seen in lesions of the median longitudinal fasciculus such as multiple sclerosis.
Pursuit eye movements allow clear viewing of objects moving slowly in the visual environment by allowing the eye to focus the image on the fovea. The match of eye speed to target speed is termed “gain.” Pursuit performance is highly affected by age, alertness, attention, and cooperation.
Asymmetric pursuit is considered significant for a central or visual disorder, as is gain that is markedly decreased, with a substitution of saccades for normal smooth pursuit. This gives the appearance of “stair steps” on the eye movement tracing (Fig. 10–5) rather than normal smooth pursuit tracings (Fig. 10–6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


