Acute fulminant invasive fungal sinusitis in an immunocompromised host and bacterial rhinosinusitis with intracranial or orbital extension are challenging to manage and constitute true otolaryngic emergencies. In the absence of rapid diagnosis and treatment, these diseases can be fatal. In this article, the complications of bacterial rhinosinusitis are divided into three categories: local, orbital, and intracranial. They vary in their characteristics and severity according to their location, duration, and specific symptoms. This article reviews the pathophysiology, clinical presentation, diagnosis, and treatment options of acute invasive fungal sinusitis rhinosinusitis, the most common subtype in the United States.
Invasive fungal sinusitis
Invasive fungal sinusitis is one of the most challenging forms of sinonasal pathology to manage, most commonly presenting in immunocompromised individuals. Diagnosis of invasive fungal sinusitis requires histopathologic evidence of fungi invading nasal tissue: hyphal forms within the sinus mucosa, submucosa, blood vessels, or bone . Invasive fungal sinusitis has been subclassified into three distinct forms: acute fulminant invasive fungal sinusitis (AFIFS), chronic invasive fungal sinusitis, and granulomatous invasive fungal sinusitis . The focus of this article is on the acute fulminant form of invasive rhinosinusitis, the most common subtype in the United States. Failure to diagnose and treat this entity promptly usually results in rapid progression and death.
AFIFS results from the rapid spread of fungi from the nasal and sinus mucosa by way of vascular invasion into the orbit, vessels, and parenchyma of the brain. The time course of less than 4 weeks’ duration separates acute from chronic disease . Patients typically have ailments associated with impaired neutrophil function (hematologic malignancies, aplastic anemia, hemochromatosis, insulin-dependent diabetes, AIDS, organ transplantation) or are undergoing iatrogenic immunosuppression with systemic steroids or chemotherapeutic agents . Although rare, cases of AFIFS in otherwise healthy individuals have been documented in the literature .
Diagnosis
Several studies have investigated the signs and symptoms of AFIFS to determine the subset of patients who require a more aggressive diagnostic investigation. In the immunocompromised patient population, the presence of fever of unknown origin after 48 hours of appropriate broad-spectrum intravenous antibiotic or the presence of localizing sinonasal symptoms should prompt imaging studies and nasal endoscopy . The physical findings in AFIFS can be subtle, but the most consistent finding is an alteration in the appearance of the nasal mucosa. Mucosal discoloration can be variable, and may be gray, green, white, or black. Discoloration, granulation, and ulceration typically replace the normal pale-pink mucosa. White discoloration indicates tissue ischemia secondary to angiocentric invasion, whereas black discoloration is a late finding of tissue necrosis. In a series by Gillespie and colleagues , mucosal abnormalities were seen most commonly on the middle turbinate, followed by the septum, palate, and inferior turbinate. Anesthetic regions of the face or oral cavity are features of early invasive process and may precede the development of objective changes in the mucosa. Decreased nasal mucosal bleeding or sensation should also be noted because they may be signs of fungal invasion.
Intraoperative nasal endoscopic examination may be the most informative test for possible fungal involvement in pediatric patients who have severe neutropenia (absolute neutrophil count 600 cells/μL or fewer), persistent fevers, or localizing sinus symptoms. Park and colleagues discovered that bedside endoscopic findings did not correlate with intraoperative endoscopy because of a large amount of debris in the nasal cavity that was not removed during bedside examinations and the relative noncompliance of the pediatric patients. Examination under general anesthesia was recommended for nasal endoscopic examination and directed biopsies of suspicious lesions, the middle and inferior turbinate.
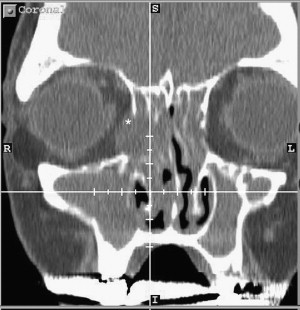
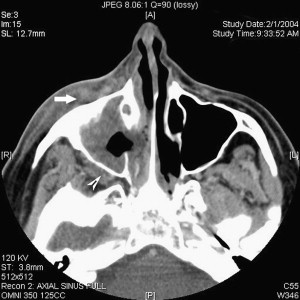
CT of paranasal sinuses is usually obtained during the workup of immunocompromised patients who have fever or sinonasal symptoms, usually before evaluation by an otolaryngologist. Fine-cut (2-mm) slices in the axial and coronal planes should be obtained in high-risk patients. Intravenous contrast is used if intracranial or intraorbital extension is suspected, but it is not necessary for most initial evaluations. Severe unilateral thickening of the nasal cavity mucosa has been shown to be the most consistent finding on CT, suggestive of underlying invasive fungal sinusitis . It has also been suggested that infiltration of the periantral fat planes ( Fig. 1 ) may represent the earliest imaging evidence of AFIFS . Although the diagnosis of AFIFS cannot be made on the basis of imaging, CT scans are helpful in defining individual variations in sinus architecture and possible periorbital and intracranial spread. MRI is superior to CT in delineating the intracranial extent of the disease and it may have a role in evaluating patients who demonstrate signs of intracranial invasion: mental status changes, orbital apex syndrome, seizure, or stroke.
Diagnosis of AFIFS incorporates clinical suspicion with culture and microscopic examination of the specimens. Because prompt diagnosis is essential, the potassium hydroxide–calcofluor white method can be used immediately on culture aspirate material. This highly sensitive technique uses potassium hydroxide to dissolve human material, and an optic brightener (calcofluor white) that binds to the cell wall of the hyphae. Fungal cell walls, including septations, fluoresce when viewed using a fluorescence microscope . The fungal cultures may take days to weeks to grow but may be needed for antifungal susceptibility testing. Proper speciation also provides important clinical data, because certain species, such as Pseudallescheria boydii , do not respond to amphotericin. Histopathologic evaluation of the suspected tissue, however, is typically the most critical to making the diagnosis. Permanent section with the Gomori-methenamine-silver stain uses deposition of silver onto the fungal cell wall, and, because it can detect even a single cell, it undoubtedly is the most sensitive of the commonly used histologic stains. No histologic specimen should be considered to be negative for fungus unless a silver stain has been performed . Fungal disease is determined to be invasive if it meets the following criteria: (1) hyphal forms within the submucosa, with or without angiocentric invasion and (2) tissue necrosis with minimal host inflammatory cell infiltration . Frozen section allows for a timely diagnosis, and, if positive, appropriate antifungal therapy and extended surgical resection can be initiated without delay. Neither frozen section nor special stains will definitely distinguish among fungal species, but this distinction can generally be made on permanent histopathologic sections. Mucormycosis fungal elements are broad, ribbon-like, irregular, and rarely septated, whereas the Aspergillus sp demonstrate more narrow hyphae with regular septations and 45° branching . Aspergillus sp can be angioinvasive, but it is not the obliterative invasion seen with mucormycosis .
Treatment and prognosis
The treatment of AFIFS requires reversal of the underlying predisposing condition, surgical debridement, and appropriate systemic antifungal therapy. Treatment of diabetic ketoacidosis or correction of neutropenia can be initiated concurrently with systemic antifungals. In transplant patients, or those who have hematologic malignancies, white blood cell transfusions and administration of granulocyte colony–stimulating factor to increase an absolute neutrophil count to above 1000/mm 3 have been shown to improve survival .
Medical antifungal therapy for most patients who have AFIFS consists of systemic amphotericin B at intravenous doses of 0.25 to 1.0 mg/kg/d to a total dose of 2 to 4 g over six to eight weeks. The use of amphotericin B is limited in some patients secondary to renal toxicity, and they may be candidates for liposomal amphotericin B at a concentration of 3 to 5 mg/kg/d. Liposomal amphotericin, secondary to high cost, is reserved for a clinically proven fungal infection in an immunocompromised host with an elevated serum creatinine (>2.5 mg/dL) or progression of fungal disease while on maximum dosage of standard amphotericin. Voriconazole, approved by the Food and Drug Administration in 2002, is more effective than amphotericin B for invasive aspergillus .
Antifungals alone are not sufficient in the treatment of invasive fungal sinusitis. Early aggressive endoscopic sinonasal debridement should be performed on all patients who have biopsy-proven disease or on any patient suspected of having fungal invasion. Radical resections (radical maxillectomy, craniofacial resection, and orbital exenteration) to remove disease outside the sinonasal cavity rarely achieve negative margins or improve long-term survival . Endoscopic sinus debridement slows the progression of the disease, reduces the fungal load, and provides a specimen for culture and histopathologic diagnosis . Debridement of the involved sinuses or structures is extended until clear bleeding margins are exposed. Hemorrhage in thrombocytopenic patients can be reduced if the platelet count is greater than 60 × 10 9 /L. A second-look procedure should be scheduled within 48 to 72 hours if residual disease in the sinonasal cavity is suspected. Follow-up consists of weekly rigid nasal endoscopy until reversal of neutropenia, and should be once a month for 6 months thereafter .
Although earlier studies have cited the mortality for AFIFS to be as high as 50% to 80%, more recent series have demonstrated a mortality rate of less than 20% . However, a mortality rate approaching 100% has been demonstrated in patients who have symptomatic intracranial involvement . Thus, patients who have orbital apex involvement or intracranial spread are less likely to respond to radical surgery, and should be appropriately counseled when a radical surgical procedure is considered . Identification of the fungal organism can also be an important predictor of survival. The overall mortality of patients infected with Mucor (29%) is higher than in those infected with aspergillus (11%), regardless of the patient’s underlying condition . The survival rates in those with invasive mucormycosis reflect the variance in the ability to reverse the underlying predisposing cause . Neutropenic patients who respond to granulocyte colony–stimulating factor are more likely to become disease survivors; this subset of patients is more likely to have disease limited to the sinonasal cavity, which is also more amenable to limited resection . In a large retrospective review by Parikh , the overall mortality rate directly as a result of invasive fungal sinusitis was found to be 18%. When examining each specific disease subgroup, the mortality rate from invasive fungal sinusitis among diabetic patients (40%) was significantly higher than in patients who had hematologic malignancy (11%), chronic steroid users (33%), and solid organ transplant patients (0%). This disparity can be due to a greater incidence of Mucor over Aspergillus affecting diabetics and a delay in diagnosis resulting in more advanced disease at presentation in this subgroup of patients .
Complications of rhinosinusitis
Rhinosinusitis has become one of the most common chronic illnesses in the United States, affecting one in eight persons . Complications of rhinosinusitis range from relatively benign to potentially fatal and are divided into three categories: local, orbital, and intracranial.
Local complications
Mucocele
Paranasal sinus mucoceles are chronic, cystic lesions that are lined with pseudostratified or low-columnar epithelium containing occasional goblet cells. These are slowly concentrically expanding lesions, frequently requiring more than 10 years to become symptomatic. Although the exact pathophysiologic mechanisms are still uncertain, mucoceles are generally classified as primary or secondary . Primary mucoceles (also called mucus retention cysts) develop secondary to blockage of the duct of a minor salivary gland within the lining of the paranasal sinus, primarily in the maxillary sinus, and are not discussed further here.
A secondary mucocele results from obstruction of a sinus ostium caused by the obstructive complications of chronic rhinosinusitis, polyposis, trauma, surgery, or tumor. The sinuses most commonly involved (in decreasing order of frequency) are the frontal sinus, ethmoid sinuses, maxillary sinus, and sphenoid sinus . Headache and diminished vision constitute the most common presenting symptoms of sphenoid sinus mucocele . The most common clinically significant mucocele originates in the frontal sinus where sinusitis in a chronic state can predispose to slow formation of a mucocele over the course of many years .
Diagnosis
Frontal headache and proptosis are the most common presenting complaints of patients who have frontal mucocele, with displacement of the globe in a downward and outward direction. Deep nasal or periorbital pain may occur. In contrast to acute or chronic sinusitis, nasal obstruction and rhinorrhea are unusual findings . Although the diagnosis may be suggested by the clinical presentation, past medical history, or physical examination, radiographic imaging is necessary for accurate analysis of the regional anatomy and the extent of the lesion. On CT scan, mucoceles appear as hypodense, nonenhancing masses that fill and expand the sinus cavity. The typical mucocele contents have low density and do not enhance. As the mucus becomes more inspissated, the density may increase. On MRI, the signal intensity of the mucocele varies with its protein content and the degree of hydration ( Fig. 2 ). After injection of gadolinium contrast, on T1-weighted image with fat suppression, the mucocele shows no enhancement, with some enhancement of the mucosa along the margin of the mucocele. This finding can help rule out solid tumors, which show significant enhancement .
Treatment
Traditional management of mucoceles emphasized the need for complete removal of the lining to achieve a cure, usually involving an open surgical approach. More recently, transnasal endoscopic techniques have essentially replaced the earlier methodology for most mucoceles. Endoscopic marsupialization of mucoceles, rather than complete removal, as a treatment concept, relies on the ability of the sinus mucosa to return to a normal or near-normal condition .
Frontal sinus mucoceles differ from similar lesions of other sinuses in that the frontal outflow tract is usually narrower and less accessible for conventional intranasal surgery. The osteoplastic flap with fat obliteration has been the gold standard against which other frontal sinus procedures have been compared. More recently, endoscopic drainage and marsupialization techniques have largely replaced the osteoplastic flap for the management of frontal mucoceles, with recurrence rates at, or close to, 0% . Har-el treated 66 frontal and frontoethmoidal mucoceles endoscopically and reported a recurrence rate of 0.9%. For frontal sinus mucoceles, a minimum Draf II procedure was performed and most large mucoceles were managed with a Draf III, also termed the endoscopic modified Lothrop procedure (EMLP). A retrospective study evaluated the efficacy of EMLP for complicated frontal mucoceles treated over a 4-year period (1998–2002). Twenty-one patients underwent the EMLP and, at a median follow-up of 16 months, all patients had a patent mucocele opening and had improvement in symptoms and signs. Although excellent results have been confirmed, given the nature of mucoceles, long-term results (5–10 year follow-ups) are needed before endoscopic drainage of these lesions can be validated completely. Furthermore, although mucoceles of paranasal sinuses are increasingly treated by endoscopic surgery, external approaches with or without obliteration of the sinus occasionally remain useful as tools in the treatment of this disease.
Osteomyelitis and Pott’s puffy tumor
The frontal sinus is the most common sinus involved with osteomyelitis; osteomyelitis of other sinuses is rare . Pott’s puffy tumor (PPT), first described by Sir Percivall Pott in 1775, is a subperiosteal abscess (SPA) of the frontal bone that appears as a localized swelling of the overlying region of the forehead associated with frontal osteomyelitis . PPT can result from acute and chronic frontal sinusitis and has become an uncommon entity since the introduction of antibiotics. Although the association of epidural purulent collections with PPT is well recognized, other intracranial abnormalities, such as subdural empyema and intracerebral abscess, have also been described.
The sinus mucosa, marrow cavity, and frontal bone share common venous drainage through the valveless diploic veins. The spread of infection from the frontal sinuses into the frontal bone causes inflammation in the diploic system, with local suppuration, that propagates to the Haversian system of the inner and outer tables of the skull and causes localized demineralization and necrosis. This process then leads to perforation of the anterior table of the frontal sinus, resulting in the subperiosteal pus collection and formation of granulation tissue known as PPT. The involvement of the venous structures explains the development of epidural abscess in cases where the posterior wall of the frontal sinus is intact, or the presence of subdural empyema without epidural abscess or dural violation .
The most common causative organisms are Staphylococcus aureus , nonenterococcal streptococcus , and oral anaerobes. Cultures from patients who have PTT often reveal polymicrobial involvement. When intracranial complications occur, anaerobes such as Fusobacterium , Bacteroides , and anaerobic Streptococci are the predominant pathogens . It has been suggested that the reason why these organisms are common in frontal sinusitis, although uncommon in diseases affecting other sinuses, is the relatively lower oxygen concentration in the frontal sinus .
Diagnosis
The presenting symptoms of osteomyelitis and PPT include headache, photophobia, swelling of the forehead, purulent and nonpurulent rhinorrhea, and fever. Fluctuant and tender erythematous swelling of the scalp at the midforehead is a typical sign . In complicated cases with intracranial abscesses, headache is almost always present, in addition to signs of increased intracranial pressure (nausea, vomiting, lethargy) and focal neurologic deficits .
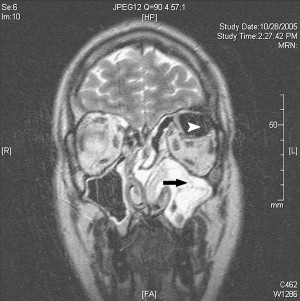
CT ( Fig. 3 ) is the diagnostic modality of choice for PPT, but MRI is the gold standard for the diagnosis of any intracranial complication. On CT with contrast, SPA will be visualized as a hypodense collection of fluid external to the frontal bone with an enhancing rim that represents the thickened, displaced periosteum; this finding corresponds to the clinically palpable PPT .

Treatment
Surgical intervention is the treatment of choice for PPT. Treatment should include intravenous administration of broad-spectrum antibiotics followed by evacuation of the SPA and removal of the osteomyelitic bone up to the margins of normal bone. Consistent with the literature on osteomyelitis in long bones, antibiotic therapy for a minimum of 6 weeks is recommended. Anticonvulsants are used in patients who have intradural infection .
Frontal sinusitis can be addressed through endoscopic frontal sinusotomy and through external approaches such as frontal trephination. Functional endoscopic sinus surgery has been advocated for the treatment of acute complicated sinusitis , and endoscopic frontal sinusotomy has the advantage of avoiding facial scars, preserving the bony superstructure of the frontal sinus infundibulum, and preserving a greater amount of mucosa than an external approach . However, the risk of major complications varies between 1% and 2% and may increase when the surgery is performed on acutely inflamed sinuses, when the increased vascularity and consequent hemorrhage may obscure the operative field . Frontal trephination is a relatively simple and effective procedure, and it can be a mainstay of treatment for complicated sinusitis requiring immediate surgical treatment. Mortimore and Wormald found that 80% of patients who had complicated sinusitis undergoing frontal sinus trephine, irrigations, and drainage of purulence did not require further surgery. If definitive surgery is still required after the frontal sinus trephine, it can be performed at a later date under more advantageous conditions.
Orbital complications
The spread of infection from the paranasal sinuses to the orbit represents the most common site of extension of rhinosinusitis. Ethmoid sinusitis can extend through the thin lamina papyracea or through congenital, surgical, or traumatic dehiscences in the medial or superior walls. The infections may also spread into the orbit through the anterior and posterior ethmoid neurovascular foramina and the valveless veins (communicating between the nose, paranasal sinuses, pterygoid plexus, and the orbit). Although frontal sinusitis alone rarely causes orbital complications, communication from the frontal sinus to the orbit may occur in three sites of dehiscence in the frontal bone: behind the trochlear fossa, behind the supraorbital notch, and at the junction of the middle and outer thirds of the sinus floor . Sinusitis-related orbital infection is the most common cause of unilateral proptosis in children and the third leading cause in adults, behind Graves’ orbitopathy and pseudotumor . Children appear to be more prone to orbital complications, probably secondary to the high incidence of acute rhinosinusitis in the pediatric population. Based on the anatomy and the presumed pathogenesis of orbital infections, Chandler classified the orbital complications into five groups, as shown in Table 1 .
| I. Inflammatory edema (preseptal) | Lid edema, no limitation in ocular movement or visual change |
| II. Orbital cellulitis (postseptal) | Diffuse orbital infection and inflammation without abscess formation |
| III. Subperiosteal abscess | Collection of pus between medial periosteum and lamina papyracea, impaired extraocular movement |
| IV. Orbital abscess | Discrete pus collection in orbital tissues, proptosis and chemosis with ophthalmoplegia and decreased vision |
| V. Cavernous sinus thrombosis | Bilateral eye findings and worsening of all other previously described eye findings |
Orbital complications are most commonly the result of Streptococcus sp, anaerobic micro-organisms, Staphylococcus sp, and other organisms associated with sinusitis, including gram-negative bacilli. Although a broad range of Streptococcus is implicated in rhinosinusitis and its complications, recent series have specifically identified Streptococcus milleri as an isolate in orbital and intracranial complications .
Inflammatory edema
Preseptal cellulitis describes infection limited to the skin and subcutaneous tissues of the eyelid anterior to the orbital septum. It is the most common and least severe complication, and is responsible for approximately 70% of all orbital complications of sinusitis . Preseptal cellulitis is more common than orbital cellulitis, especially in children, and results from impeded venous and lymphatic drainage from the obstructed sinus.
Diagnosis
Examination of a patient who has preseptal cellulitis will reveal eyelid swelling, erythema, and tenderness. Visual acuity, pupillary reaction, extraocular motility, and intraocular pressure are normal. CT is usually unnecessary in patients who have preseptal infections, but, if done, would reveal a diffuse increase in density and thickening of the lid and conjunctiva . CT is mandatory when intracranial complications are suspected or when signs or symptoms of postseptal inflammation (findings of proptosis, gaze restriction, or changes in visual acuity) progress in 24 to 48 hours despite therapy .
Treatment
The management of preseptal cellulitis should include broad-spectrum oral antibiotics, head elevation, warm packs, and management of the underlying cause. Although intravenous antibiotics were standard care for preseptal cellulitis in children before the introduction of the Haemophilus influenzae type B (Hib) vaccination in 1985, oral broad-spectrum antibiotics are now often appropriate for mild cases and when good follow-up is ensured . Controversy still remains as to whether these patients should be admitted for intravenous antibiotics and close examination, especially children under 3 years of age. A nasal decongestant, either topical or oral, mucolytics, and saline irrigations may help promote sinus drainage.
Orbital cellulitis
Orbital cellulitis defines an infectious process that occurs within the orbit proper, behind the orbital septum, and within the bony walls of the orbit. The orbital contents show diffuse edema with inflammatory cells and fluid, without distinct abscess formation. The swelling of orbital contents occurs when an increase in sinus venous pressure is transmitted to the orbital vasculature, resulting in transudation and leakage through the vessel walls .
Diagnosis
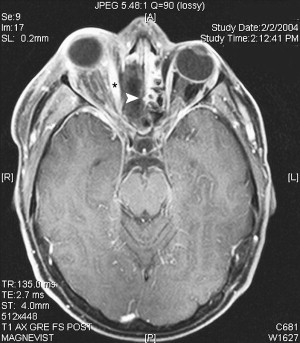
Clinically, the patient has eyelid edema, mild proptosis, and chemosis. Orbital pain is present in 85% of patients . In severe cases, motility may be limited; however, visual acuity is not impaired. When orbital cellulitis is suspected, ophthalmologic consultation should be obtained to assess visual acuity, pupillary reaction, confrontation visual fields, color vision, extraocular motility, proptosis, globe displacement, resistance to globe retropulsion, intraocular pressure, and optic nerve appearance . Orbital imaging should be obtained in all patients suspected of having orbital cellulitis. Axial and coronal views of the orbits and sinuses with contrast should be obtained in soft tissue and bone windows. CT with contrast ( Fig. 4 ) will show some enhancement of edematous orbital fatty reticulum and adjacent tissues. The involvement is maximal in the extraconal fat directly adjacent to the most severely affected sinus. Although proptosis is usually present, suggestive of more diffuse involvement, intraconal fat may be radiographically normal. Other findings include eyelid swelling, which is uniformly present, and enlargement and contrast enhancement of the adjacent rectus muscle, which is present in some cases .
Treatment
After initial evaluation by an ophthalmologist, orbital cellulitis patient should have daily assessments of visual acuity and color vision, pupillary reaction, and extraocular motility. Early treatment should include intravenous antibiotics and imaging to determine which orbital and associated sites are involved. Antibiotic failure is indicated by progression of vision loss, persistent fever after 36 hours of antibiotic treatment, clinical deterioration after 48 hours of antibiotics, or failure to improve within 72 hours of antibiotic treatment . Surgical drainage is recommended when one of five circumstances is present :
- •
CT evidence of abscess formation
- •
Visual acuity of 20/60 (or worse) on initial evaluation
- •
Severe orbital complications (eg, blindness or an afferent pupillary reflex) on initial evaluation
- •
Progression of orbital signs and symptoms despite therapy
- •
Lack of improvement within 48 hours despite medical therapy
Subperiosteal abscess
SPA is most commonly located in the superomedial or inferomedial orbit in conjunction with ethmoid sinusitis. The abscess develops when infection breaks through the lamina papyracea or travels through the anterior or posterior ethmoidal foramina. The subperiosteal fluid collection can expand rapidly and may lead to blindness by compromising optic nerve function through several possible mechanisms: direct optic nerve compression, elevation of intraorbital pressure, or proptosis causing a stretch optic neuropathy . Even with aggressive medical and surgical intervention, about 15% to 30% of patients who have SPA develop various visual sequelae .
Diagnosis
As in orbital cellulitis, ophthalmologic evaluation is essential. Clinically, SPA is suspected when a patient who has orbital cellulitis develops worsening proptosis and gaze restriction. The ability to distinguish colors may be used as a guide of disease progression because increasing intraorbital pressure causes loss of red/green perception before deterioration of visual acuity .
On CT images, axial views optimally demonstrate the displacement of the medial rectus muscle and the abscess within the orbit, whereas coronal cuts ( Fig. 5 ) are useful to delineate orbital and sinus anatomy. With contrast-enhanced CT, the SPA is seen as a contrast-enhancing mass in the extraconal space. The ring-enhanced lesion or air-fluid level is pathognomonic for an SPA. Marked proptosis is seen, occasionally with a conic deformity of the posterior aspect of the globe. Osteomyelitis of the orbital wall can be seen in advanced cases. Extension of the inflammatory process into the intraconal space appears on CT as an ill-defined infiltration of the orbital fat with obliteration of optic nerve and extraocular muscles . Depending on the size of the abscess, the adjacent rectus muscle is generally displaced inward and enlarged. One recent study used a lateral displacement of the medial rectus muscles of at least 2 mm as a diagnostic criterion for an SPA .