39

Intravitreal Triamcinolone
Francisco Gómez-Ulla  Javier Ferro
Javier Ferro  Maria José Blanco
Maria José Blanco  Maximino Abraldes
Maximino Abraldes
BACKGROUND
Glucocorticosteroids are synthetic analogs of hormones produced by the suprarenal gland. Traditionally these drugs have been used for their anti-inflammatory properties and as immunosuppressants, for their ability to inhibit the activities of different cells types including lymphocytes, macrophages, neutrophiles, basophiles, endothelial vascular cells, and fibroblasts. The inhibitory effect of corticoids on fibroblast proliferation and endothelial vascular cells (1) had been observed in vitro and given rise to numerous possible therapeutic applications. However, these therapies were initially hindered by the inability to obtain sufficiently high doses of intraocular glucocorticoids using traditional topical or systemic administrations (2). In 1970, Machemer et al. (3) were the first to use intravitreal steroids in an animal model with retinal detachment. Intravitreal injections of triamcinolone were administered to obtain sufficient concentrations of intraocular corticoids inside the eye to prevent the development of proliferative vitreoretinopathy (PVR) after surgery. Other experimental models appeared later, evaluating the therapeutic effects of corticoid injections into the vitreous cavity (4, 5).
Corticosteroids are known to reduce inflammation and tissue edema. Clinical studies suggest that intravitreal injections of steroids after the vehicle is removed may be an appropriate treatment for intraocular neovascular or edematous diseases (6–9). Steroids have been found to be potent inhibitors of vascular endothelial growth factor (VEGF) and may reduce the leakage of fluid from compromised capillaries in patients with maculopathy as well as inhibit neovascularization.
Triamcinolone acetonide (TA) is a corticosteroid with practically no water solubility which prolongs its presence in the vitreous nearly five times as compared to hydrocortisone (10). This increased media life makes it a useful alternative for the treatment of inflammatory ocular pathologies or other proliferative intraocular diseases.
Since the 1970s, many articles have been published evaluating the pharmacological effects of intraocular triamcinolone, as well as determining its safety and therapeutic effectiveness for a wide range of ophthalmologic pathologies (11–16).
In 1977, Perry et al. (17) published an article describing the apparent safety of an accidental intravitreal injection. A similar situation was described in 1993 by Gomez-Ulla et al. (18), when paramethasone acetate was inadvertently injected into the vitreous cavity during a subtenon’s placement of the medication; side effects were not noted. These incidents preceded planned intravitreal corticoid injection. The first intentional intraocular injections of triamcinolone in humans were administered in 1993 and 1994 by Dominguez et al. (19, 20) for the treatment of pathologies like macular edema and choroidal neovascularization and in 1995 by Pendfold et al. (21) to treat 28 patients with exudative or wet age-related macular degeneration.
INTRAVITREAL STEROIDS IN DIABETIC RETINOPATHY
Intravitreal triamcinolone acetonide (IVTA) has been applied with an exponentially increasing frequency for various intraocular neovascular and edematous diseases, including diabetic macular edema (DME), proliferating diabetic retinopathy, and neovascular glaucoma due to proliferative diabetic retinopathy (PDR).
In DME, the edema may almost completely resolve, and visual acuity may increase as much as macular ischemia and the tissue destruction by the diabetic process may allow. For PDR and neovascular glaucoma, investigations have suggested an antiangiogenic effect of IVTA (22). The use of other steroids like intravitreal dexamethasone and slow release device such as sustained release fluocinolone intravitreal implant, are also areas of active research.
IVTA is a promising therapeutic method for DME that fails to respond to conventional laser photocoagulation (23–28).
Different techniques (nonfilter and filter techniques) applied to reduce the solvent agent benzyl alcohol (9.9 mg/ml) from a commercially prepared TA suspension were made (29).
Two different nonfilter techniques were used: sedimentation and centrifugation. Commercially prepared TA suspension was allowed to sediment overnight and 0.9 ml of the supernatant was extracted with a tuberculin syringe. The pellet was resuspended with 0.9 or 0.5 ml of balanced salt solution (BSS). In the other nonfilter technique, the commercial suspension was centrifuged at 3000 × g for 5 minutes; 0.9 ml of the supernatant was extracted with a tuberculin syringe and the pellet resuspended with 1 ml of BSS.
Filtered triamcinolone has been prepared by taking 0.62 ml from the commercial TA ampoule, following the technique described by Jonas (8, 9). The extracted volume was placed in a tuberculin syringe (1 ml) filled with Ringer lactate solution. Two different syringe driven filter units were evaluated: a Millipore filter and a Pall filter. The selected filter was placed on the top of the syringe and most of the contents of the syringe were pressed through the filter, with the triamcinolone crystals remaining in the syringe. The syringe was refilled with Ringer lactate solution and the same procedure was repeated three times. In the end, 0.2 ml of the solution was left in the syringe.
Intravitreal injection of triamcinolone effectively reduces macular thickening due to diffuse DME, at least in the short term. However, in this chronic disease, the need to repeat intravitreal injections every 4 to 6 months will increase the risk of injection-related complications and may not be tolerated by the patients.
The injection technique is as follows. Topical anesthesia is applied to the ocular surface followed by preparation with 5% povidone iodine. A cotton-tipped applicator soaked in povidone iodine is then applied to the injection site, 3.5 mm posterior to the limbus in pseudophakic eyes and 4.0 mm posterior to the limbus in phakic eyes. TA is injected through the inferior pars plana at a dose of 4 mg (0.1 ml). A 30-gauge needle is used. Indirect ophthalmoscopy is used to confirm proper intravitreal localization of the suspension and perfusion of the optic nerve head (30).
The complications of IVTA include secondary ocular hypertension in about 40% of the eyes, medically uncontrollable high intraocular pressure (IOP) leading to antiglaucomatous surgery in about 1% to 2% (31, 32), posterior subcapsular cataract and nuclear cataract leading to cataract surgery in about 15% to 20%, especially in elderly patients within 1 year after injection (22, 33), postoperative infectious endophthalmitis with a rate of about 1:500 or 1:1000 (34–36), noninfectious endophthalmitis (36, 37), and pseudo-endophthalmitis (38), which can recur even after successive injections (39). IVTA can be combined with other intraocular surgeries including cataract surgery (40), particularly in eyes with iris neovascularization due to diabetic retinopathy.
Pars plana vitrectomy (PPV) with or without internal limiting membrane (ILM) peeling has also been advocated for the treatment of diabetic maculopathy (41), the reasons being mainly to relieve anteroposterior vitreomacular traction, tangential traction, as well as to remove interleukin 6 (IL-6), VEGF and other vasopermeable factors from the vitreous, improve microcirculation, and improve oxygenation (42–45). The benefit of ILM peeling is that it ensures that all posterior hyaloidal traction has been removed (46). When laser photocoagulation and TA treatment is not effective for diabetic maculopathy, vitrectomy with the complete removal of the posterior hyaloid face, including possible removal of the ILM, should be considered (47–49). TA greatly improves the visualization of the ILM. TA is used during vitrectomy to visualize the hyaloid. After the posterior hyaloid is surgically separated from the optic nerve head and posterior retina, TA suspension is injected over the posterior pole and an intraocular forceps is used to peel the ILM in a circumferential manner. The peeled area is seen as an area lacking white specks.
Several complications of advanced diabetic retinopathy can be treated surgically. Vitrectomy can clear media opacities, relieve traction on the retina, and make adequate laser treatment of the retina possible. IVTA may be an additional tool in PPV for PDR (50). After a core PPV, a little quantity of TA aqueous suspension (40 mg/ml) is injected into the mid vitreous cavity (51). This suspension is very useful to delaminate and remove the fibrovascular proliferation and to visualize the posterior hyaloid, thus allowing a complete posterior hyaloid separation and removal. After surgery, 0.1 to 0.2 ml of TA is left in the vitreous cavity to help the reabsorption of macular edema and control intraocular inflammation (Figs. 39-1 to 39-3).
Triamcinolone Acetonide Used as an Aid to Visualization of the Vitreous and the Posterior Hyaloid during Pars Plana Vitrectomy
The interaction between the posterior vitreous cortex and the retinal surface plays a key role in the pathogenesis of several ocular diseases. An attached or incompletely separated posterior hyaloid can provide a source of traction in conditions such as macular hole (MH), vitreomacular traction syndrome, and PVR or serve as a scaffold for fibrovascular proliferation in PDR.
Although a complete removal of the vitreous and posterior hyaloid membrane is an important surgical goal when a PPV is used to treat the above mentioned diseases, a layer of posterior vitreous cortex often remains on the retinal surface after an apparent vitreous detachment during surgery. Consequently, in spite of the development of different surgical techniques for creating a surgical PVD using cannulas (silicone tipped or hard) and forceps with active or passive suction, the surgeon cannot be certain that the posterior hyaloid separation and complete vitrectomy have been successful because of the transparency of these structures.
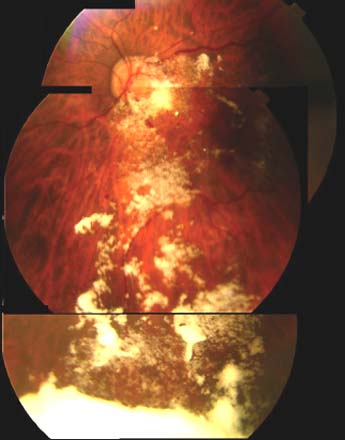
Figure 39-1. Intraocular triamcinolone crystals following vitrectomy for diabetic macular edema.
In 2000, Peyman et al. (52) first described the use of IVTA as an aid to improve the visualization of the posterior hyaloid and thus assist in its separation during PPV. The IVTA-assisted PPV permits the observation of the residual vitreous cortex left on the retina as small islands which can be removed using vitreal forceps. Similarly, the use of IVTA enables the visualization of all the epiretinal membranes (ERMs) by showing a clear contrast with the unstained retina. IVTA suspension particles trapped in the peripheral vitreous also enable a clear visualization of the vitreous base, which permits its complete removal (53).
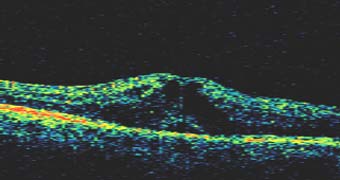
Figure 39-2. The optical coherence tomography scan obtained through the fovea revealed loss of the normal foveal contour, diffuse macular thickening, intraretinal cysts, and fluid accumulation.
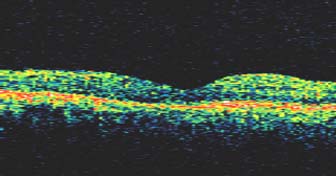
Figure 39-3. Optical coherence tomography done 3 months after vitrectomy and intravitreal triamcinolone acetonide showed a decrease of foveal thickness, complete resolution of intraretinal cysts and a normal macular anatomical architecture.
It is not surprising to suggest that the intraoperative use of intravitreal TA has at least three advantages: the provision of certainty during the surgical maneuver by improving the visualization of the hyaloid, the detection of a very thin hyaloid cortex as well as ERM’s remaining on the retinal surface and the reduction of postoperative inflammation, which is a major cause of postoperative complications, like PVR. We must remember that PVR is the most common cause of rhegmatogenous retinal detachment surgery failure and it is responsible for recurrent retinal detachments in 5% to 10% of eyes. In the surgical repair of rhegmatogenous retinal detachment complicated with PVR, the major goals are the removal of vitreous scaffolding and tractional membranes and the use of IVTA facilitates the visualization and delineation of both.
Different authors have carried out a TA-assisted PPV in several diseases such as DME, PDR, and PVR (52–58) stressing good vitreous visualization, the absence of retinal toxicity, and the possibility of preventing fibrin syndrome and PVR after surgery. Sakamoto et al. used IVTA to improve the visibility of the hyaloid during PPV in 13 eyes with PVR and found favorable anatomic and functional results. By use a laser flare meter, they also found a significantly lower postoperative blood-ocular barrier breakdown in the eyes treated with IVTA-assisted PPV than in those treated without IVTA. Enaida et al. (55) found that the number of reoperations due to preretinal fibrous membrane formation decreased in TA-assisted PPV for all cases and especially in those with PDR, with a significant statistical difference.
Although Hida et al. (59) have suggested that the vehicle of commercially available depot corticosteroid, and not the crystalline itself, could be toxic to intraocular tissue, no relevant postoperative complications in terms of retinal toxicity were observed in these studies. The absence of toxic effects of commercially available IVTA may be explained by the low dose injected and by the fast removal of TA from the vitreous cavity. The same reason could explain why pathologically increased IOP which is one of the most common postoperative complications of intravitreal triamcinolone (31), has not been found.
Triamcinolone Acetonide-Assisted Peeling of the Internal Limiting Membrane
The peeling of the ILM has been recommended as an effective means of reducing tangential traction on the retina surface in many macular diseases, especially in idiopathic MHs (60, 61), cellophane maculopathy or macular pucker, and diabetic retinopathy. Many reports suggest that ILM peeling increases the rate of anatomic closure of the MH and may decrease late reopening (62). However, the removal of the ILM is very complex because of the difficulty in its visualization and consequent risk of incomplete peeling or retinal damage.
Recently, the concept of staining the ILM has been introduced. Indocyanine green (ICG) was first used to enhance visualization and removal of the ILM (63), however, concerns regarding its toxicity persist (64, 65). Trypan blue and TA were subsequently reported to have similar effects (56, 66, 67). While ICG stains all layers of the ILM and alters the cleavage plane between the ILM and the innermost retinal layers, TA does not stain the ILM selectively and does not behave like a stainer. It forms a thin layer with white specks on the surface of the ILM, which not only assists in the initial picking-up of the ILM, but also helps in identifying the margins of the unpeeled ILM, which are sometimes missed during the ILM peeling without an adjuvant.
Although the preservative in TA suspension may cause toxic effects on the retina (59), TA itself may not be toxic because submacular deposition of the substance has reportedly shown no apparent adverse effects (68). In MH surgery one must take special care not to leave any intraocular deposit, because this is thought to be the responsible for the hole closure failure.
TRIAMCINOLONE ACETONIDE-ASSISTED PARS PLANA VITRECTOMY IN HIGH MYOPIA
It is well known that the vitreous gel of patients with high myopia differs from emmetropic subjects. Synchisis and syneresis of the vitreous are common findings in young myopic patients. It is also conceivable that the vitreoretinal adhesion may be weaker in those patients explaining why posterior vitreous detachment (PVD) appears to develop nearly 10 years earlier in high myopia (> −6 diopters) than in emmetropia (69).
Diagnosing PVD in high myopia is more difficult than in nonmyopia. It can be commonly misdiagnosed with large lacuna formation or extensive vitreous liquefaction, because the posterior hyaloid membrane is thin and delicate. The thinness of the posterior cortex can explain the difficulty in assessment preoperatively as well as during surgery. It could also explain the interesting occurrence of a PVD in some previously vitrectomized eyes in which the posterior hyaloid membrane has been left in place with or without a thin sheet of cortical gel. TA (52) is the best tool to assess and map the relationship between the posterior hyaloid and its retinal surface.
In nonmyopic eyes without PVD, the premacular liquefied space usually seems to lose the construction of gel and forms only a thin layer of vitreous cortex that becomes clearly visualized as a white structure after injection of TA. Another liquefied space with a similar appearance is confirmed on the optic disk adjacent to the premacular area (Fig. 39-4). Both liquefied areas are separated by a “wall” of thick vitreous cortex with few TA crystals accumulated at that point, and correspond to previous autopsy findings called bursa premacularis or posterior vitreous pocket, and Martegiani’s space respectively. In highly myopic eyes without PVD however, these structures cannot be individualized after TA injection. We speculate that the main cause for this phenomenon is the lack of thick vitreous surrounding both the prepapillary and the premacular spaces.

Figure 39-4. Normal appearance of the triamcinolone stained vitreous highlighting the premacular bursa and Martegiani’s space in nonmyopic eyes at the time of vitreous surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


