Chapter 64 Intraoperative Neurophysiologic Monitoring
MONITORING FACIAL NERVE
History
Krause1 first described facial nerve monitoring in 1912 using a faradic stimulation during cochlear nerve section for tinnitus. Twitching of the ipsilateral facial muscles during stimulation helped him preserve the facial nerve, and the patient had transient facial weakness postoperatively. In the 1960s, dedicated facial nerve monitoring systems were developed. The Hilger stimulator2 was used principally in the assessment of facial paralysis, but was also used during surgery. Further developments in facial nerve monitoring occurred in the 1970s and 1980s. Delgado and colleagues3 described the use of electromyography (EMG) monitoring in cerebellopontine angle (CPA) surgery. Moller and Jannetta4 combined the specificity of EMG recording with the advantage of acoustic feedback to the surgeon.
Electromyography
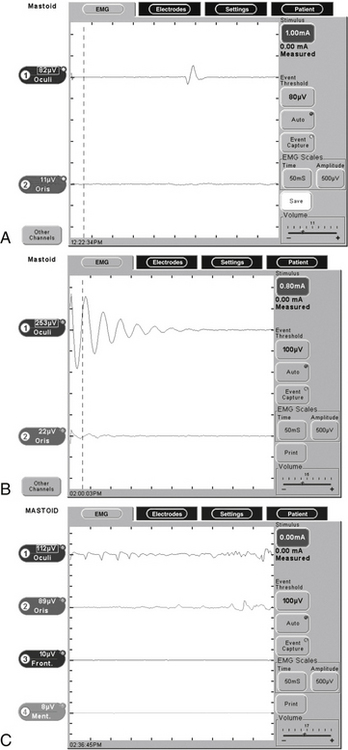
Subdermal needle electrodes are most commonly used for facial nerve monitoring. They have the advantages of ease of use, low impedance, and stability (less likely to be displaced than surface discs or cups). Monitoring more than one muscle provides additional sensitivity and redundancy.5 For two-channel bipolar recording, a typical sensing montage includes a pair of electrodes in the orbicularis oculi approximately 1 cm apart and another pair in the orbicularis oris (Fig. 64-1). The ground electrode is placed in the forehead, and the anode for the monopolar nerve stimulator is inserted at the ipsilateral shoulder. The operating room is a noisy place with abundant electric interference. The connections are checked by tapping the electrodes and observing an audible and oscilloscopic response. This mechanical compound muscle action potential results in a characteristic sound from the monitor. A second check, when available, involves testing the impedance of the inserted electrodes.
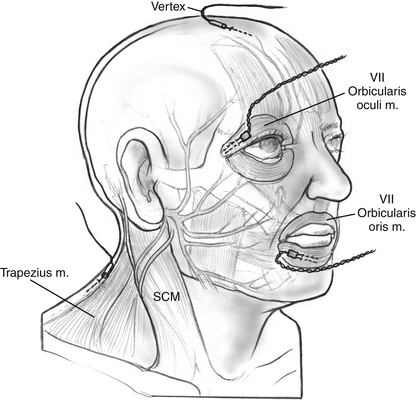
FIGURE 64-1 Electrode placement for facial nerve intraoperative monitoring. SCM, sternocleidomastoid.
Many facial nerve monitoring systems are available commercially, including the Nerve Integrity Monitor (Xomed, Inc., Jacksonville, FL) (Fig. 64-2), Neurosign 100 (Smith & Nephew Richards, Inc., Memphis, TN), Brackmann II (WR Medical Electronics Co., Stillwater, MN), and NEI (Grass Instrument Co., Quincy, MA). All of these devices use EMG. The Silverstein Facial Nerve Monitor (WR Medical Electronics Co.,) is an example of a motion detector device. Some systems, such as the Silverstein Monitor, include the ability to electrify instruments to aid with monitoring.
Stimulation
Pulsed stimulation may be safer and more efficacious.6 The parameters of safe nerve stimulation are 100 to 250 μs pulses with a range of 0.05 to 0.5 mA.5 The upper limit of safe nerve stimulation varies along the course of the nerve, but animal studies have shown myelin and axonal injury using 2 mA stimulus for 3 seconds.7 A 0.5 mA stimulus applied briefly 50 times was found to manifest no functional or histologic evidence of injury in a mouse model.8 Most normal facial nerves should be stimulated with direct contact of the probe using a 100 μs pulse of 0.05 mA. Settings of 0.05 to 0.1 mA are recommended when working close to the nerve. Farther from the nerve, currents of 0.2 to 0.3 mA may be used. Higher settings may be required when the nerve is covered by bone, connective tissue, or granulation tissue. Cerebrospinal fluid or blood may shunt current from a stimulator probe. In these cases, stimulation with a constant voltage may be used.
In an attempt to determine the threshold necessary to detect a surgical dehiscence of the facial nerve electrically, Choung and associates9 prospectively estimated the minimal threshold of electric current needed to change the EMG of facial muscles using the Nerve Integrity Monitor (NIM)-2 in 100 patients. They found that 43% of ears with surgical dehiscence responded to electric stimulation of 0.7 mA or less. The mean threshold of minimal electric stimulation was 0.29 mA for tympanic segments and 0.41 mA for mastoid segments.
Burst Activity
During the course of surgery, many burst potentials may be observed and are usually not associated with significant trauma to the nerve. Bursts are brief discharges in which the stimulus and response are simultaneous (see Fig. 64-2). Burst activity occurring with gentle manipulation suggests a healthy nerve. Very similar responses may be obtained, however, when drilling close to or after complete transection of the nerve. Lack of burst activity during dissection may be associated with minor manipulation of a healthy nerve, significant manipulation of an already injured nerve, or a problem with the monitoring connections and instruments. Electrically stimulating the nerve at this point verifies the integrity of the nerve.
Trains
Episodes of repetitive EMG activity may occur several seconds to minutes after the stimulus, making it difficult to identify the initiating factor or to modify dissection technique. As seen in Figure 64-2, trains are caused by prolonged depolarization of the nerve beyond its threshold for developing an action potential. Subsequent repetitive firing continues until the nerve repolarizes, or can no longer sustain the repetitive activation.5 The most common initiating factor is traction on the nerve. Trains may indicate significant trauma has occurred, although this is not always the case. Changes in temperature around the nerve may also precipitate train activity. When caused by cool irrigating fluid, the spontaneous activity usually subsides with warming. When a train pattern develops after laser application or cautery, however, thermal damage should be suspected. Elevated stimulation thresholds after repetitive nerve activity suggest significant injury. Higher frequency train activity (>50 Hz) with an amplitude greater than 250 μV is associated with a more ominous outcome; in a series of 51 patients, Nakao and coworkers10 found that 86% of patients with train activity having an amplitude greater than 250 μV had severe facial nerve dysfunction. More than 10 seconds of cumulative train time is associated with postoperative facial paresis.11
Anesthetic Issues
It is common practice that when facial nerve monitoring is employed, neuromuscular blocking agents are avoided after induction of anesthesia. In 2003, Kizilay and associates12 examined the effects of different levels of neuromuscular blockade (NMB) on electric stimulation thresholds of the facial nerve during otologic surgery. Minimal facial nerve stimulation causing EMG responses in the facial musculature was measured during recovery from the effects of muscular relaxants and with 25%, 50%, 75%, and 100% levels of NMB. All of the patients had detectable EMG responses of the facial musculature at the 50% and 75% levels of NMB in response to the electric stimulation (mean 0.1 mA) of the facial nerve. No responses were measured in 31% of the patients when the level of peripheral NMB was 100%. The investigators concluded that a regulated 50% level of peripheral NMB provides reliable intraoperative EMG monitoring of the facial musculature in response to electric stimulation and adequate anesthesia, with full immobilization of the patient. Chronic injury resulting from compression from a tumor may make the facial nerve more sensitive to the effects of NMB, however.13
Practical Application in Surgery
Locating the Facial Nerve
Monopolar stimulation is especially useful for mapping the nerve throughout its course.4 Monitoring becomes more important in cases of large tumors.5 A stronger stimulus may need to be used to confirm that the nerve is not in close proximity to an area of tumor to be removed. False-positive responses may be obtained from stimulation of the superior vestibular and cochlear nerves owing to electric current dispersion, especially within the internal auditory canal where the nerves lie in close proximity to one another. Stimulation of the trigeminal nerve may elicit motor activity that can be interpreted as facial nerve stimulation. False-negative responses are usually related to technical errors such as failure to connect the stimulus probe, anesthetic-induced muscle paralysis, or impedance imbalances.
Postoperative Prognosis and Prognosis of Acute Injury
The threshold for stimulation has been shown to correlate with postoperative facial nerve function. When using constant current stimulation with a 50 μs pulse, if the threshold for facial nerve stimulation at the brainstem was 0.1 mA or lower, 90% of patients exhibited House-Brackmann grade I or II function at 1 year after CPA surgery.14 Thresholds of 0.1 to 0.2 mA were associated with grade I or II function in 77% of cases.15 The amount of energy delivered to the nerve using a 50 μs pulse of 0.1 mA is equal in magnitude to a 100 μs pulse of 0.05 mA as delivered by many commercial facial nerve monitors. When testing the nerve at the root entry zone of the brainstem to determine threshold at the conclusion of the procedure, it is important to contact the nerve long enough to confirm the precisely timed pulses of electric stimulation. A single noise could be a mechanically evoked burst, which may give the surgeon a falsely optimistic estimate of nerve function.
In 2005, Grayeli and colleagues16 looked at the short-term facial prognostic value of a four-channel facial EMG device in vestibular schwannoma surgery. In 89 patients, EMG detection was performed in frontal, orbicularis oculi, orbicularis oris, and platysma muscles. Postoperative facial function at 6 months was assessed as House-Brackmann grade I or II in 80%, as grade III or IV in 16%, and as grade V or VI in 4% (n = 80). A proximal threshold between 0.01 and 0.04 mA had a positive predictive value of 94% for good facial function (grade I or II). The proximal threshold was lower in patients with improving or stable facial function compared with patients with a delayed deterioration between days 8 and 30. The maximal EMG response was detected in the frontal muscle or the platysma in 27% of cases and in orbicularis oris and oculi in 73% of cases.
Also in 2005, Neff and coworkers17 sought to evaluate prospectively whether the intraoperative stimulus threshold and response amplitude measurements from facial EMG can predict facial nerve function at 1 year after vestibular schwannoma resection. In 74 consecutive patients, the minimal stimulus intensity and EMG response amplitude were recorded during stimulation applied to the proximal facial nerve after vestibular schwannoma removal. Of the 74 patients, 66 of 74 (89%) had House-Brackmann grade I or II facial nerve function, and 8 of 74 (11%) had House-Brackmann grade III-VI function at 1 year after surgery. With intraoperative minimal stimulus intensity of 0.05 mA or less and response amplitude of 240 μV or greater, the authors were able to predict a House-Brackmann grade I or II outcome in 56 of 66 (85%) patients at 1 year after surgery. With these same electrophysiologic parameters, only 1 of 8 (12%) patients with House-Brackmann grade III-VI also met this standard and gave a false-positive result. Logistic regression analysis of the data showed that a stimulus threshold of 0.05 mA or less and a response amplitude of 240 μV or greater predicted a House-Brackmann grade I or II outcome with a 98% probability. Stimulus threshold or response amplitude alone had a much lower probability of the same result, however.
A similar study by Isaacson and colleagues18 looked at two independent intraoperative monitoring parameters in predicting long-term facial nerve function in 60 patients undergoing resection of vestibular schwannomas. They found that 5 of 60 (8.3%) patients showed significant long-term weakness (i.e., House-Brackmann grade III or worse). Intraoperative monitoring parameters (proximal stimulation threshold, proximal-to-distal response amplitude ratio) were accurate in predicting increased risk of long-term facial nerve dysfunction when used in a logistic regression model. Table 64-1 summarizes a selection of studies using facial nerve monitoring to evaluate postoperative prognosis in acoustic neuroma surgery38–47.
TABLE 64-1 Studies Using Facial Nerve Monitoring to Predict Facial Nerve Function after Acoustic Neuroma Surgery
| Study | N | Result |
|---|---|---|
| Lin et al, 2006 | 38 | With 0.3 mA stimulus, proximal-distal amplitude >50% had PPV 93% for HB grade II or better immediately postoperative |
| Grayeli et al, 200516 | 89 | Stimulation threshold of 0.01-0.04 mA had PPV 94% for HB grade II or better 180 days postoperative using four-channel EMG |
| Neff et al, 200517 | 74 | For <0.05 mA stimulus and response amplitude of >0.240 V, authors could predict 85% of patients with HB grade II or better 1 yr postoperative |
| Isaacson et al, 2003 | 229 | Using proximal-distal amplitude and stimulation threshold, authors developed regression function with sensitivity 89%, specificity 83%, PPV 94% in predicting HB grade III or worse in immediate postoperative period |
| Fenton et al, 2002 | 67 | Using stimulation current and tumor size, authors developed regression function correctly describing 93% of patients at 2 yr follow-up |
| Goldbrunner et al, 2000 | 137 | With proximal-distal amplitude >80%, 98.4% had HB grade I at 6 mo |