Among the several risks encountered in endoscopic sinus surgery, catastrophic orbital bleeding and iatrogenic cerebrospinal fluid leak are the two serious complications surgeons most fear. This article discusses these avoidable complications and provides treatment algorithms for intraoperative maneuvers. A thorough understanding of the anatomy of the paranasal sinuses and their relationships with the anterior skull base, appropriate preoperative planning, and meticulous surgical technique are essential for preventing intraoperative cerebrospinal fluid leaks. Intraoperative orbital hematoma is discussed and a stepwise approach to reduce complications is provided.
Over the past 20 years, endoscopic sinus surgery has been widely used as a safe and effective treatment for disorders of the paranasal sinuses that are refractory to medical therapy. Advances in surgical technique, including powered instrumentation and stereotactic image-guided surgery, have improved the efficiency and safety of this procedure. Despite these advances, complications are still encountered.
Among the most common risks encountered in endoscopic sinus surgery (eg, bleeding, infection, injury to the eye, cerebrospinal fluid [CSF] leak, anosmia, myocardial infarction, cerebrovascular accident, need for revision surgery), approximately 83% to 100% of patients considered cerebrospinal fluid leak or injury to the eye to be the most important risks warranting discussion. Similarly, catastrophic orbital bleeding and iatrogenic CSF leak are the two serious complications surgeons most fear. However, thorough preoperative planning and meticulous surgical technique can help minimize these risks. Moreover, surgeons managing these complications using a stepwise approach can avoid untoward long-term sequellae.
This article discusses these two avoidable complications and provides treatment algorithms for intraoperative maneuvers.
Intraoperative cerebrospinal fluid leaks
Prevention of intraoperative CSF leaks begins with a thorough understanding of the anatomy of the paranasal sinuses, particularly their relationships with the anterior skull base.
Anatomy of the anterior skull base
Surgeons must understand the relationship between the ethmoid sinuses and the anterior skull base. Understanding this relationship begins in the preoperative setting through reviewing CT images of the patient’s anatomy. CT imaging must be performed in the coronal plane in all patients before undergoing endoscopic sinus surgery. If available, thin slice (1.0–3.0 mm) axial images reconstructed in the coronal and sagittal planes provided further elucidation of the skull base anatomy.
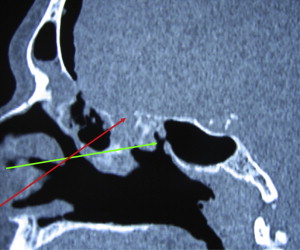
Coronal images provide crucial information on several critical areas that, if overlooked, can lead to intraoperative complications. On coronal images, the height of the maxillary sinus should be compared with the height of the ethmoid sinuses. The ratio of maxillary-to-ethmoid height ( Fig. 1 ) can vary from 1:1 to 2:1 and can be used preoperatively to guide how dissection through the basal lamella will lead to the anterior skull base along the posterior ethmoid sinuses. Meyers has shown how this ratio can lead to inadvertent injury to the anterior skull base during dissection. The ratio can be further examined along the slope of the skull base, which is best viewed in sagittal or parasagittal images. A line extended from the limen nasi to the basal lamella will identify the distance to which the skull base will be encountered. Additionally, the slope of the skull base from frontal recess to planum sphenoidale will correlate these findings. The thickness of the anterior skull base should also be examined thoroughly with both coronal and sagittal CT images. The thickness of the anterior skull base varies and is often asymmetric in individual patients. Knowing the thickness of the anterior skull base is important, because the roof of the ethmoid has been shown to be the place of least resistance during dissection ( Fig. 2 ) . In addition to its anatomy, the skull base itself should be examined for areas of dehiscence, thinness, and thickness, and for soft tissue that might suggest an encephalocele.
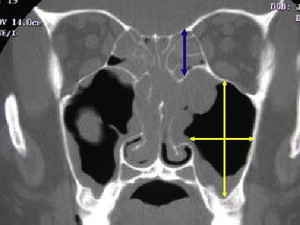
The region of the ethmoid roof and cribriform plate is of critical importance and is best analyzed in the coronal plane. In the midline of the ethmoid bone is the cribriform plate ( lamina cribrosa ), which represents the lowest point of the skull base in the median aspect of the nasal cavity. Multiple perforations of the cribriform plate permit transmission of neural fibers into the nasal cavity that contribute to olfaction. The lateral mass (or labyrinth) of the ethmoid is suspended laterally from the cribriform plate by the fovea ethmoidalis, or ethmoid roof. Interposed between the cribriform plate and the fovea ethmoidalis is the lateral cribriform lamella. The sagittal buttress of the middle turbinate is suspended from the articulation of the cribriform plate and the lateral cribriform lamella. When viewed in the coronal plane, the three bony structures are said to possess a “gull wing in flight” appearance ( Fig. 3 ); however, this structure has significant variations. Keros and colleagues studied the relationship of these bony structures and proposed a classification based on the length of the lateral cribriform lamella. The classification is as follows: Keros type I (1–3 mm deep), Keros type II (4–7 mm deep), and Keros type III (8–16 mm deep). Ali and colleagues showed that type II anatomy is the most commonly encountered and the symmetry of the olfactory fossa varies widely among patients . The classification is useful because patients who have a lower Keros classification are believed to have a lower risk for intracranial injury and those who have a higher Keros classification a higher risk for intracranial injury and postoperative CSF leak.

Intraoperative management of cerebrospinal fluid leaks
Despite review of the preoperative films, use of intraoperative stereotactic image-guided surgery, and meticulous surgical technique, a violation of the anterior skull base can occur. If this untoward event occurs, the authors recommend the algorithm provided in Fig. 4 to manage this complication.
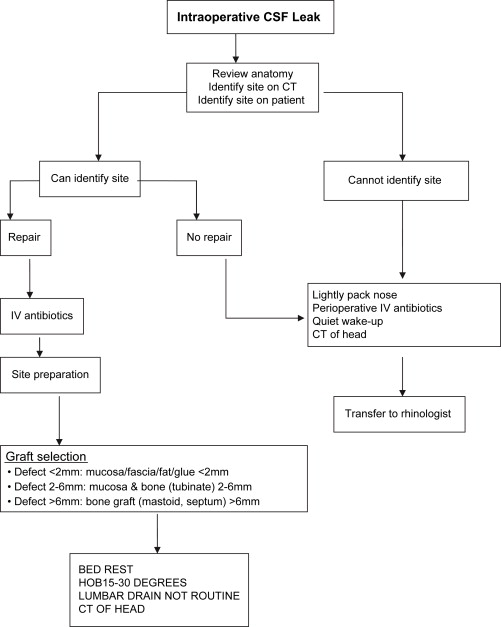
When a leak occurs, the surgeon should stop and review the anatomy. Landmarks (eg, posterior wall of the maxillary sinus, attachments of the middle turbinate, anterior face of the sphenoid sinus, skull base) within the patient should be identified to help reorient the surgeon, and then the preoperative and stereotactic imaging should be used to help localize the probable site of the leak. The most likely sites of injury include the lateral cribriform lamella and cribriform plate; therefore, surgeons should review these areas for dehiscences, asymmetries, thinness/thickness, or any bony abnormalities on the preoperative imaging. Additional attention should be directed to the posterior ethmoid sinuses to determine if reduced posterior ethmoid height (ie, maxillary–ethmoid ratio greater than 1:1) is present that would precipitate inadvertent injury to the skull base. If a particular region is suspected, an attempt should be made to correlate the radiographic site with the region endoscopically.
If the site cannot be completely identified or if the operating surgeon does not feel equipped to repair the defect, then adequate hemostasis should be obtained and the nasal cavity lightly packed to help apply gentle pressure to the defect. The surgeon should be aware that the process of gaining hemostasis can actually cause more complications, and the endoscopic view greatly magnifies any blood loss. They should therefore proceed with caution, especially when using monopolar cautery near the skull base. The upper and lower aerodigestive tract should be aspirated for blood and antiemetics administered to minimize postoperative nausea. All efforts should be made to minimize increases in intracranial pressure, and particular attention should be directed toward minimizing Valsalva maneuvers during arousal from general anesthesia. If safe, a deep extubation can be performed. Avoidance of nasal positive airway pressure is imperative, despite the extubation plan, because of the potential for pneumocephalus. Immediate head CT is warranted to document that no hematoma or pneumocephalus has occurred, which can be life-threatening.
The efficacy of antibiotic prophylaxis for preventing meningitis in patients who have postsurgical CSF leaks has not been studied in a prospective manner; however, several retrospective reviews of traumatic CSF leaks have yielded conflicting information. A meta-analysis by Brodie and colleagues showed no significant differences in the rates of ascending meningitis in patients treated with and without antibiotics in traumatic anterior skull base CSF leaks. Conversely, Bernal-Sprekelsen and colleagues found an incidence of ascending meningitis in 29% of patients treated conservatively (eg, head of bed elevation, bed rest). Although not statistically significant, 40% of patients treated transcranially also developed meningitis. However, in a separate study, these investigators found an incidence of ascending meningitis in 36.5% of patients undergoing endoscopic repair of CSF leaks. During endoscopic sinus surgery, presumably the anterior skull base is penetrated with an instrument (eg, curette, microdebrider), and bacteria or inflamed or infected mucosa is implanted intracranially, which may contribute to infection. Therefore, the authors believe it is prudent to administer perioperative parenteral antibiotics (eg, ceftriaxone) that effectively cross the blood–brain barrier, because an intraoperative CSF leak by definition includes an element of direct trauma to the brain, however minor.
A subarachnoid lumbar drain has been advocated for planned treatment of CSF leaks. However, no prospective studies have examined the use and duration of lumbar drains in patients who have experienced iatrogenic endoscopic sinus surgery injuries. In most instances, the authors believe a lumbar drain is unnecessary for an iatrogenic injury unless the patient has signs of benign intracranial hypertension, empty sella syndrome, or radiographic evidence of dehiscent bone along the skull base that would otherwise suggest elevated intracranial pressures.
Finally, transfer of service to a local rhinologist is recommended for continued care of the patient. Operating surgeons should proceed with closure only after they have identified the site of leak, understand the anatomy, and are prepared to attempt closure, and the patients are stable.
Transnasal endoscopic repair of CSF leaks has been reported to be successful in 90% to 97% of patients during a first attempt. Once the site of the leak is identified and prepared, surgeons should adhere to three goals: (1) safe and successful closure of the leak; (2) maintenance of sinus function; and (3) prevention of postoperative complications. The major sites of anterior skull base injury are reviewed.
Ethmoid/cribriform leaks
The surgical site is prepared by completing a maxillary antrostomy and total ethmoidectomy with wide exposure of the skull base. If exposure of the defect requires the removal of the middle turbinate, then its resection should be complete to prevent postoperative lateralization of the middle turbinate remnant and iatrogenic frontal recess obstruction. If the middle turbinate is removed, it should be preserved for later use as grafting material. If the repair is likely to cause postoperative obstruction of the frontal recess or the sphenoethmoidal recess, a prophylactic frontal sinusotomy or sphenoidotomy should be performed.
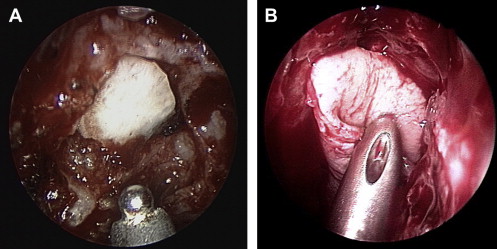
Once the defect is fully delineated, the mucosa surrounding the defect is stripped and potentially fulgurated with bipolar electrocautery 3 to 4 mm beyond the bony defect rim. The authors then size the defect measured using a trimmed ruler. Defects smaller than 2 mm will likely heal with a combination of osteoneogenesis and soft tissue fibrosis; therefore, the authors do not recommend preparing the epidural space or placing a bone graft to avoid increasing the size of the defect. Simple abrasion of the surrounding bone (scraping versus drilling with diamond bur) with placement of an overlay graft (eg, mucosa, temporalis fascia) dressed with a thin layer of fibrin glue sufficiently patches most leaks. Excessive fibrin glue should be avoided to help facilitate remucosalization.
A composite graft is often suited for the repair of defects larger than 2 mm but smaller than 6 mm. In these circumstances, a middle turbinate composite (mucosa/bone) graft is an excellent choice for repair, because the bone of the middle turbinate has similar density to the bone of the cribriform plate and anterior skull base. Resection of the middle turbinate should occur at the skull base to prevent postoperative lateralization of the middle turbinate remnant and iatrogenic stenosis of the frontal recess. Once the turbinate is harvested, it can be filleted and the mucosa stripped from one side. Once the defect is measured, the excess bone of the middle turbinate is removed, taking care to leave behind mucoperiosteum. The appropriately sized middle turbinate bone is then wedged into the defect, allowing the periosteum to be applied to the cleaned skull base and the mucosa facing the nasal cavity.
Defects larger than 6 mm are closed in a multilayered fashion with underlay bone grafting to reconstitute the native skull base anatomy ( Fig. 5 ). Septal bone and mastoid cortex are two choices for bone grafting. The advantages of septal bone include its ease of access intranasally and the osteoneogenic properties of the overlying mucoperichondrium. Care must be taken when harvesting the septal bone, because iatrogenic septal perforations may result; furthermore, portions of the septal bone may be fairly flimsy and fracture easily during placement. In situations of poor septal bone, the authors recommend using mastoid cortex, because sufficient bone is available for contouring, and soft tissue (eg, fascia, muscle) can be obtained for additional layered support. Harvesting mastoid cortex, however, requires a separate incision and site preparation, which may increase intraoperative time. The final defect size should be measured and the mucosa surrounding the defect stripped and potentially fulgurated. The dura is elevated using a round knife, ball-tipped seeker, or other appropriate instrument, and the bone graft is placed in an underlay fashion. Fibrin glue is applied lightly, and a pliable soft tissue graft (eg, fascia, mucosa) is placed as an overlay and secured with a thin coating of fibrin glue.
Sphenoid sinus cerebrospinal leaks
Leaks within the sphenoid sinus may occur during transsphenoidal hypophysectomy or during routine endoscopic sinus surgery. In these instances, fat grafting used as an onlay graft or as biologic packing to reinforce a fascial graft works well to seal midline sphenoid sinus leaks. Additionally, middle turbinate composite grafts work well to close the moderate-sized, midline sphenoid sinus CSF leak. Care must be taken during preparation to not strip the sphenoid sinus mucosa too far laterally, because this will place the optic nerve and carotid artery at a great risk for injury.
Frontal sinus cerebrospinal leaks
CSF leaks involving the frontal sinus require the most skill to repair. These leaks can be separated into those involving the frontal sinus posterior table, frontal recess, or anterior ethmoid adjacent to the outflow tract. The type of repair will depend on the location, extent of preparation, and graft selection. A wide frontal sinusotomy should be performed (if it was not previously) to prevent outflow obstruction of the frontal sinus after a repair. Any supraorbital ethmoid, agger nasi, and frontal recess cells should be widely opened so that postoperative stenosis of the frontal sinus outflow tract is avoided. If the injury or site preparation extends too far superiorly or laterally, the repair may require the assistance of a trephination or an osteoplastic flap for definitive repair. Therefore, this repair may be best left for another time or after transfer to a rhinologist.
Once prepared, the site is repaired using similar principles as described earlier. The main differences involve the use of the 70° endoscope and instrumentation (eg, frontal sinus curette, giraffe forceps) designed for the frontal sinus. A frontal sinus stent composed of thin Silastic sheeting is placed to stabilize the graft and help maintain frontal sinus patency postoperatively. This stent is removed 1 week postoperatively. Woodworth and colleagues treated seven patients who had CSF leaks originating from the frontal sinus and frontal recess using these principles, all of whom were treated successfully during the first attempt and maintained long-term frontal recess patency.
Summary
Preoperative planning and meticulous surgical technique involving the use of state-of-the-art instrumentation can help improve the efficiency and safety of endoscopic sinus surgery. When an intraoperative leak is encountered, surgeons must assess the damage and decide to stop or proceed based on their experience and resources. Proper site preparation, graft selection, and preservation of outflow tracts are essential for success. As with the conservative management algorithm, patients who undergo an intraoperative repair of an iatrogenic CSF leak should receive perioperative intravenous antibiotics (eg, ceftriaxone) and be placed on short-term bed rest. A lumbar drain is not necessary for an iatrogenic leak unless signs of increased intracranial pressure are present. A lumbar drain in this instance with the possible adjuvant administration of acetazolamide, 500 mg twice daily, can help relieve pressure on the repair, because increased CSF pressure often affects postoperative management.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


