10 Intraocular Inflammation
The uveal tract consists of the iris, ciliary body and choroid lying in continuity; inflammation in this tract is known as uveitis. Uveitis can be classified according to the principal site of inflammation as anterior uveitis, intermediate uveitis (a subgroup of which is pars planitis), posterior uveitis or panuveitis. Because the uveal tract is continuous, severe inflammation in one part may be accompanied by signs of overspill inflammation in another. For example, a severe anterior uveitis (iritis) may be accompanied by a cellular infiltrate in the anterior vitreous (some ophthalmologists would term this an iridocyclitis). Conversely, posterior uveitis may be accompanied by signs of inflammation in the anterior chamber; furthermore, diseases included under the umbrella of posterior uveitis often have significant retinal signs.
SIGNS OF UVEITIS
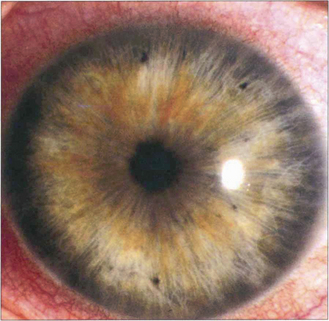
Fig. 10.1 Ciliary injection is seen here in its classical form as a dusky red circumlimbal vasodilatation in the area around the cornea where the ciliary and scleroconjunctival circulations anastomose. Its degree reflects the acuteness and severity of inflammation in the anterior uveal tract. With very severe inflammation the whole of the bulbar conjunctiva can be involved and the appearances may be difficult to distinguish from the diffuse appearance of conjunctival inflammation.
By courtesy of Dr J Krachmer.
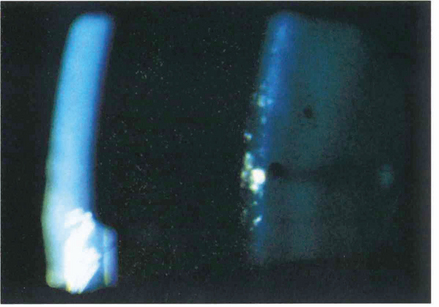
Fig. 10.2 Cells in the anterior chamber are a sign of active inflammation within the eye. The cells are leucocytes that circulate in the convection currents present within the anterior chamber. In the slit-lamp beam they have an appearance similar to that of particles of dust in a sunbeam. They are best seen by a narrow high-intensity beam directed obliquely across the anterior chamber.
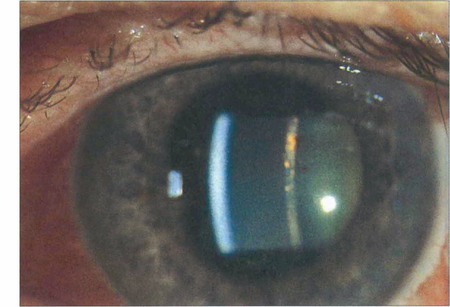
Fig. 10.3 A flare within the aqueous humour is the result of a raised protein concentration from breakdown of the blood–aqueous barrier together with locally synthesized immunoglobulin. It defines the slit-lamp beam within the anterior chamber rather like a car headlight cutting through a foggy night. Cells usually accompany flare but flare often persists for some time after the cells have disappeared indicating persistent vascular damage rather than active inflammation.
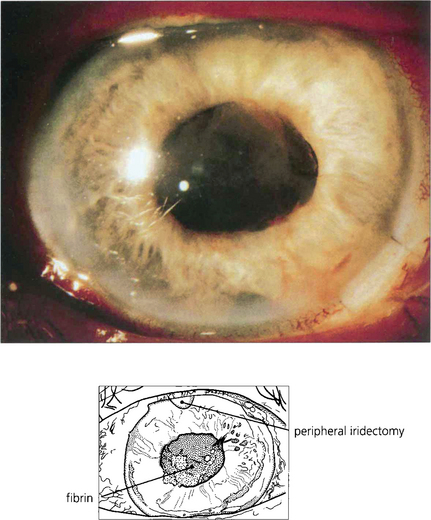
Fig. 10.4 Severe vascular damage, usually seen with really acute inflammation, infection or following surgery will allow even the largest plasma proteins to exude into the aqueous humour. Such exudation is manifested by fibrin, which clots in the anterior chamber to produce the ‘plastic’ uveitis so typical of HLA-B27-associated acute anterior uveitis.
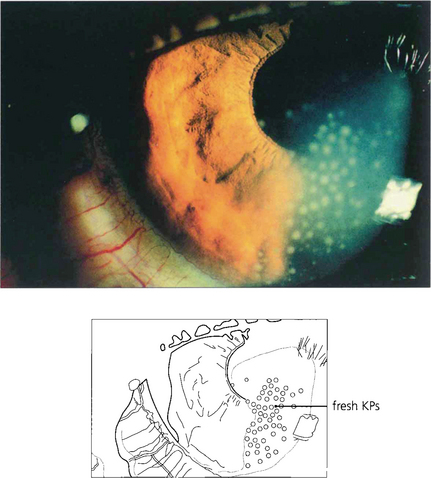
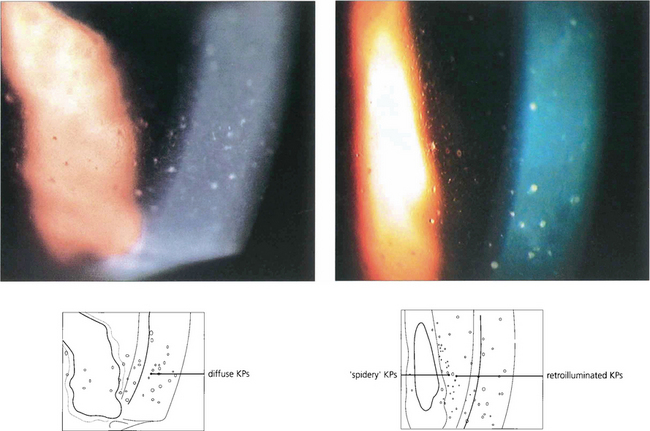
Fig. 10.5 Cells within the anterior chamber circulate through the aqueous humour to agglutinate and become deposited on the corneal endothelium. They are then known as keratic precipitates (KPs) and are one of the classical signs of anterior uveitis. KPs are typically deposited in the inferior quadrant of the cornea, probably because of gravity and convection currents within the aqueous humour. They vary in distribution and number and also in size, colour and shape.

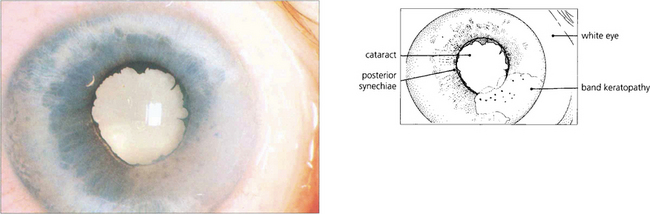
Fig. 10.6 With resolution of the uveitis with treatment or time the KPs will disappear. Chronic KPs tend to become more pigmented, as in this patient. These are typical mutton fat KPs; note the whiteness of the eye.
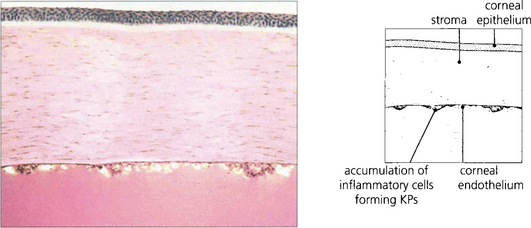
Fig. 10.7 Pathologically KPs consist of a mixture of neutrophils, macrophages and lymphocytes. Neutrophils predominate in newly formed KPs, whereas macrophages and lymphocytes are deposited later.
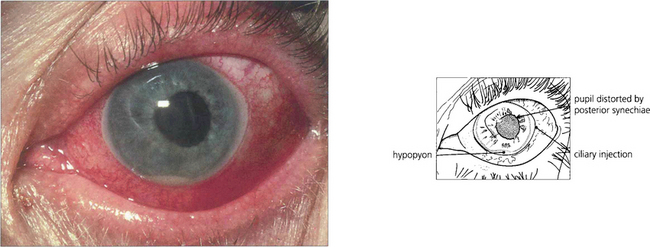
Fig. 10.8 A massive leucocytic response with an acute anterior uveitis can lead to cells precipitating as a hypopyon. This is typical of HLA-B27 positive anterior uveitis but is also seen with other causes of severe anterior uveitis such as Behçet’s disease. Hypopyon may also be the presenting sign of retinoblastoma in children, ocular lymphoma and bacterial or fungal endophthalmitis.
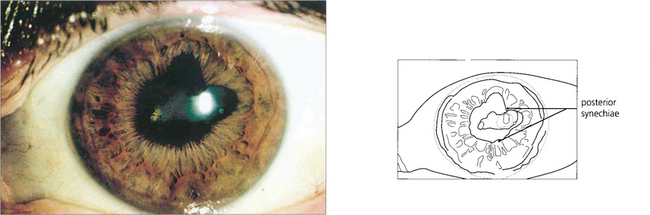
Fig. 10.9 Posterior synechiae are adhesions between the pupillary margin and anterior lens surface; they always reflect a previous anterior uveitis. Pupillary dilatation retracts the iris from contact with the anterior lens capsule and prevents their formation. This is one of the aims of mydriasis in the treatment of uveitis which will sometimes break weak adhesions to leave tell-tale pigment on the lens. Ring adhesions will seclude the pupil and prevent aqueous humour flowing anteriorly, causing iris bombé (see Ch. 8).
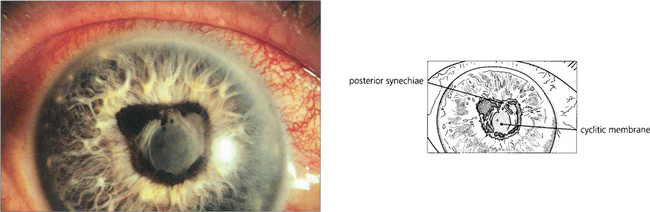
Fig. 10.10 Prolonged and severe inflammation in the anterior chamber produces a cyclitic membrane which can also occlude the pupil.
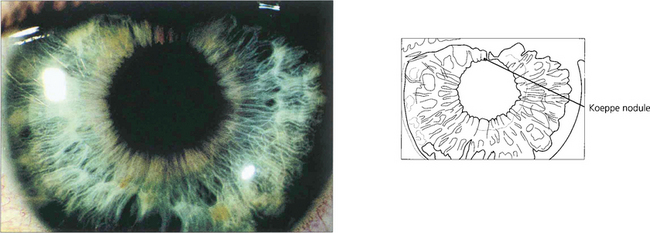
Fig. 10.11 Iris nodules are granulomas. These are known as Busacca nodules when they are in the stroma. At the pupillary margin they are known as Koeppe nodules; posterior synechiae often form at these positions.
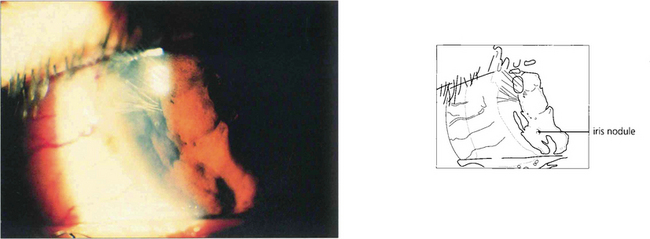
Fig. 10.12 Nodules within the peripheral iris stroma can be seen in this patient with a granulomatous uveitis due to sarcoid.
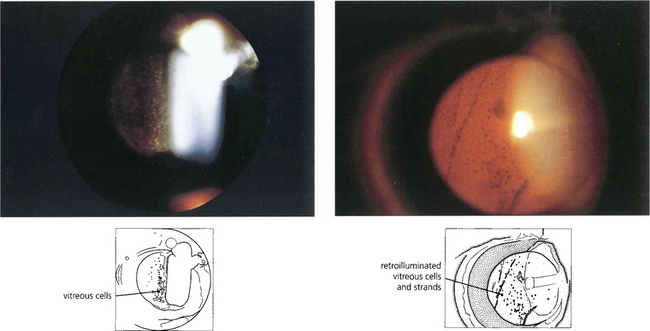
Fig. 10.13 Posterior uveitis produces a cellular vitreous infiltration, analogous to anterior chamber infiltration, but because of the viscosity and structure of the vitreous gel the cells tend to circulate less and persist for longer. Vitreous cells are sometimes distributed more locally, for instance over a focus of chorioretinitis or over the ciliary body. Cells may be distributed as a mass of single cells or accumulate as larger clusters known as ‘snowballs’; they can also be seen as retrohyaloid precipitates on a detached posterior vitreous face. Persistent vitreous inflammation leads to collapse and vitreous detachment with a hazy gel filled with debris.
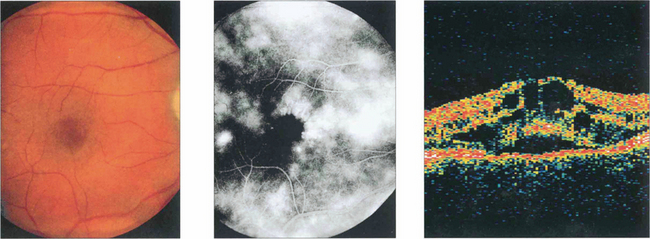
Fig. 10.14 Macular oedema can be seen with posterior uveitis of any type or severity; it is the most common cause of visual loss, although mild degrees can be compatible with normal visual acuity. Depending on the duration and severity of inflammation, the oedema resolves with the uveitis leaving a normal macula or progresses to permanent retinal damage. Macular oedema is often difficult to visualize ophthalmoscopically unless the macula is viewed stereoscopically with a fundus lens (see Ch. 1). Fluorescein angiography can be very useful in its assessment. In mild cases leakage will be seen from the parafoveal retinal capillaries; in more established cases there is pooling of fluorescein within the intraretinal cystoid spaces, giving a petalloid appearance to the angiogram. This patient with mild posterior uveitis had an acuity of 20/60, biomicroscopy showed macular thickening and fluorescein angiography shows marked macular oedema. Optical coherence tomography (OCT) clearly shows the intraretinal cystic spaces and macular thickening.
ANTERIOR UVEITIS
ACUTE ANTERIOR UVEITIS
Ankylosing spondylitis
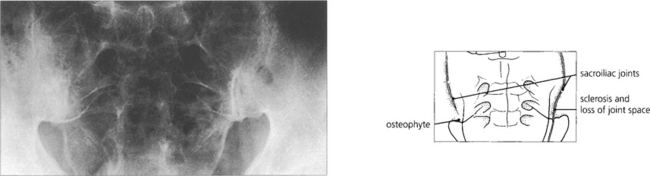
Fig. 10.15 About 50 per cent of HLA-B27-positive patients will have evidence of ankylosing spondylitis which is seen in its earliest form in the sacroiliac joints. There is sclerosis of the periarticular bone with narrowing and irregularity of the joint space, progressing eventually to ankylosis. Similar changes are seen in the spine.
Herpes zoster ophthalmicus
Keratitis (see Ch. 4) and anterior uveitis are common features of herpes zoster ophthalmicus and may occur independently of each other. It is said that keratitis and uveitis are particularly frequent if the vesicles appear along the side of the nose, the cutaneous distribution of the nasociliary nerve that also innervates the iris and pupil but this is not invariably so.

Fig. 10.18 Herpes zoster ophthalmicus with involvement of the nasociliary nerve along the lateral border of the nose. Cutaneous lesions may vary in severity from confluent vesicles to the occasional punctate lesion.
CHRONIC ANTERIOR UVEITIS
Juvenile idiopathic arthritis
Fig. 10.20 This little girl aged 4 years with pauciarticular disease has a swollen right knee on which she cannot weight bear.
By courtesy of Dr B Ansell.
Fuchs’ heterochromic cyclitis
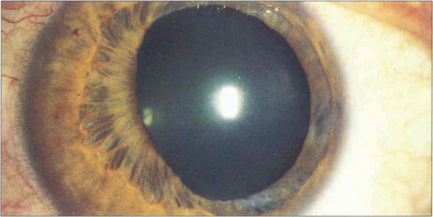
This is a distinctive entity with many features not seen with other forms of uveitis. Small diffuse KPs are scattered over the whole of the corneal endothelium with a fluffy or feathery appearance of their border in contrast to the well circumscribed and inferiorly sited KPs seen with other types of uveitis. The eye is white and posterior synechiae do not form. The iris has a characteristic moth-eaten appearance and becomes de-pigmented, showing a bluish tinge in Caucasian patients. This depigmentation is not as obvious in heavily pigmented eyes where iris stromal atrophy is the hallmark. Heterochromic cyclitis is usually unilateral although bilateral cases rarely occur and are more difficult to diagnose. Glaucoma may develop and is associated with a fine neovascularization of the iris and angle (see Ch. 8). Cataracts are common and are hastened by steroid therapy; the benefit of steroids in this condition is unproven. Histopathological examination of iris specimens shows stromal atrophy with loss of pigment, hyalinization of blood vessel walls, proliferation of vascular endothelial cells and patchy loss of pigment epithelium. There is an inflammatory cell infiltrate of eosinophils, mast cells, lymphocytes and plasma cells; Russell bodies (immunoglobulins) are present. Recent evidence suggests that the condition is due to persistent localized rubella viral infection.
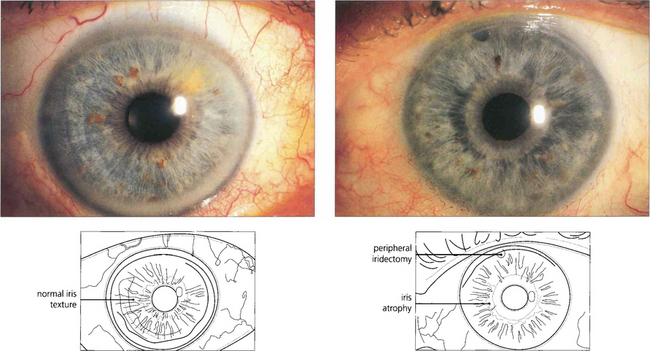
Fig. 10.22 The right eye of this patient is normal but the left shows stromal atrophy consistent with Fuchs’ heterochromic cyclitis. The left iris has a slightly bluish tinge. Note the peripheral iridectomy from previous glaucoma surgery.
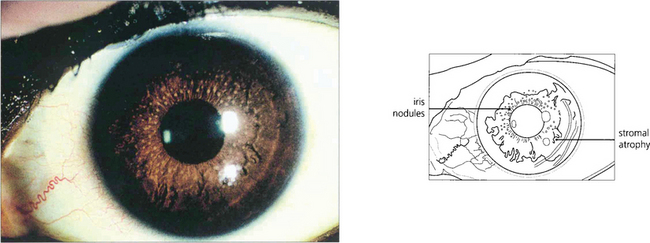
Fig. 10.23 In African Caribbean patients, heterochromia is not seen and iris stromal atrophy is the hallmark. Superficial nodules can be seen on the stromal surface in some patients.
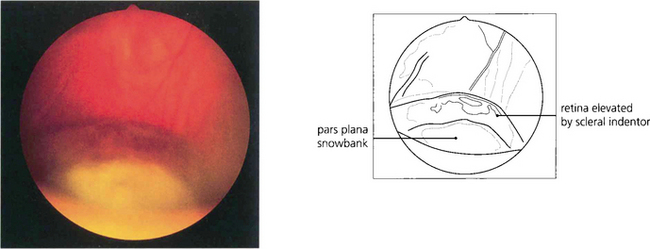
INTERMEDIATE UVEITIS
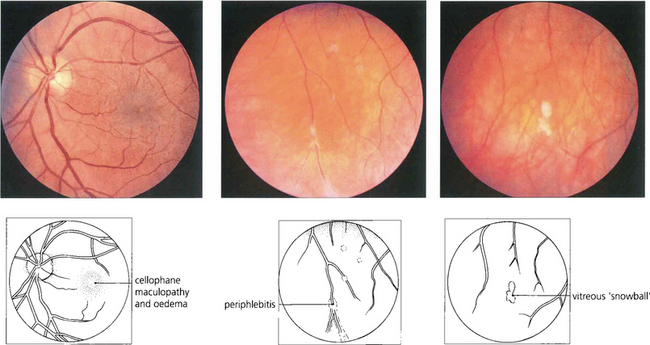
Fig. 10.26 This 42-year-old man presented with uniocular symptoms but had bilateral signs. The optic disc is normal but there is a trace of macular oedema with wrinkling of the internal limiting membrane causing blurring of vision. There was a low-grade vitreous cellular infiltrate, ‘snowballs’ within the gel inferiorly and periphlebitis of the equatorial retinal veins. The patient was systemically well and all investigations were normal.