Fig. 11.1
Snowball opacities
Epidemiology
Occurrence of intermediate uveitis varies worldwide. The prevalence of intermediate uveitis varies in different populations and accounts for 2–31 % of all uveitis presenting to tertiary eye centers in various parts of the world [7–21].
Percentage in western world: 1.4–22 %
Percentage in India: 9.5–17.4 %
Incidence: 1.4/100,000
Prevalence: 5.9/100,000
Patients of intermediate uveitis are usually in their third and fourth decade, though the disease affects patients in all age groups [19, 22]. Intermediate uveitis accounts for 10–12 % of all uveitis seen in children [23]. There is no gender or racial predilection. Bilaterality is seen in 70–90 % [12, 19, 22]. Few familial cases have been reported. Human leukocyte antigen (HLA) studies have shown common HLA haplotypes in a few families suggesting heritable cause in the etiology of the disease [24–28]. Human leukocyte antigen (HLA) DR15, a sub-allele of HLA-DR2, has highest association with intermediate uveitis and is present in 64.3–72 % of patients with intermediate uveitis [29]. HLA-DR15 positivity and intermediate uveitis association are seen in multiple sclerosis, optic neuritis, and narcolepsy [29].
Pathogenesis
Pathology
Snowbanking in pars planitis shows exudates deposited on the peripheral retina and pars plana. Histological examination of these exudates reveals a collapsed vitreous, blood vessels, fibroglial cells including fibrous astrocytes, and scattered inflammatory cells, mostly lymphocytes. Peripheral veins show lymphocytic cuffing and infiltration [30].
Immunology
Intermediate uveitis is a T-cell-mediated disease which can be initiated by an unknown antigen. The antigen may be infectious or noninfectious. Intermediate uveitis may be infectious because it is seen in tuberculosis, Lyme disease, syphilis, and cat-scratch disease. It may be autoimmune as it is seen in multiple sclerosis and sarcoidosis. Type II collagen in vitreous or type II major histocompatibility antigen on vascular endothelium may act as autoantigen initiating recruitment of activated T cells to stimulate a local vasculitis, leading to vitreous inflammation [12]. 95 % of cells in vitreous are T cells in intermediate uveitis, of which CD4+ cells are 35–90 % [31, 32]. Macrophages, epithelioid cells, and multinucleated giant cells are also seen in active inflammation [33]. Though HLA associations are studied in intermediate uveitis, it only identifies an individual at risk of developing intermediate uveitis but is not a diagnostic marker [29, 34].
Clinical Features
Bilateral
Minimal anterior chamber reaction
Anterior vitreous cells
Vitreous haze
Snowball vitreous opacities
Snowbanking
Cystoid macular edema
Symptoms
Patients with intermediate uveitis usually have insidious onset. They typically complain of floaters, blurring of vision, and mild photophobia. The eye will be usually white and quiet initially. The benign nature of the disease in initial stages postpones the patient’s visit to ophthalmologist. Minimal loss of central vision can occur in early stages due to cystoid macular edema or early posterior subcapsular cataract. Chronic cystoid macular edema, retinal detachment, complicated cataract, and secondary glaucoma may cause severe loss of vision in late stages of the disease [35].
Signs
Anterior Segment
White eye with presence of mutton-fat keratic precipitates is the usual presentation in intermediate uveitis associated with tuberculosis, sarcoidosis, and multiple sclerosis. Minimal anterior chamber reaction may be present due to spillover of retrolental cells. Posterior synechia with posterior subcapsular cataract is seen in long-standing cases. Band-shaped keratopathy along with posterior synechia is seen in chronic intermediate uveitis in children.
Posterior Segment
Vitritis is the hallmark of intermediate uveitis and is graded from trace to 4+ cells according to standardization of uveitis nomenclature [11]. Cells are always present in vitreous in active intermediate uveitis. Absence of vitreous cellular activity precludes the diagnosis of active intermediate uveitis. Inflammatory cells aggregates in vitreous are called snowballs, some of which may coalesce. Accumulation of yellow-grey exudates at the ora serrata with or without membrane formation is the characteristic feature of pars planitis. Snowbanks are exudates on the pars plana, found usually inferiorly, but may also extend 360 degrees of the retinal periphery. Snowbanking is usually associated with the more severe form of the disease and warrants aggressive therapy. Presence of snowbanking is not an absolute requirement for the diagnosis of intermediate uveitis but its presence should guide one to look for associated neovascularization which can be potential source of vitreous hemorrhage. Retinal changes in intermediate uveitis include tortuosity in arterioles and venules, sheathing of peripheral veins, neovascularizations, and retinal detachments (Fig. 11.2) [36].


Fig. 11.2
UBM showing pars plana membranes
Complications
1.
Cataract: Cataract formation in intermediate uveitis increases with the duration and severity of the disease. Inflammation along with steroid therapy will hasten its formation. Posterior subcapsular cataract is the commonest form. Early immunosuppression rather than oral steroids in young patients may delay the formation of the cataract [37].
2.
Glaucoma: Secondary glaucoma can be due to steroid response, active inflammation, chronic course, and increasing age in intermediate uveitis [38].
3.
Macular edema: Cystoid macular edema is the commonest complication in intermediate uveitis and is the cause of significant visual loss in patients with intermediate uveitis. Incidence is 12–51 %. It is directly proportional to the severity and duration of the disease (Figs. 11.3 and 11.4) [39].
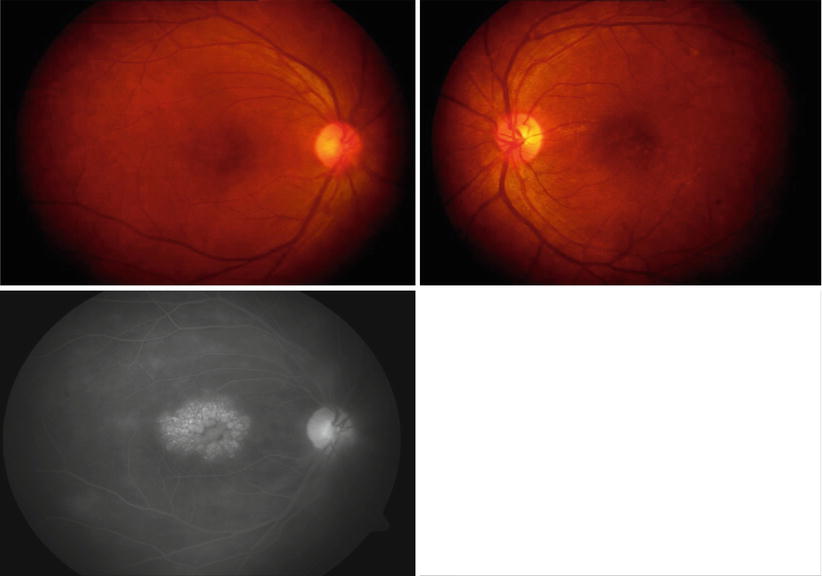
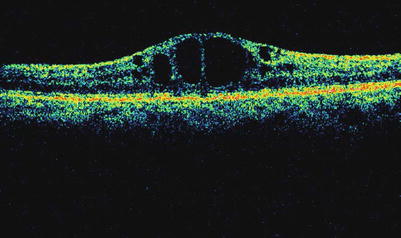
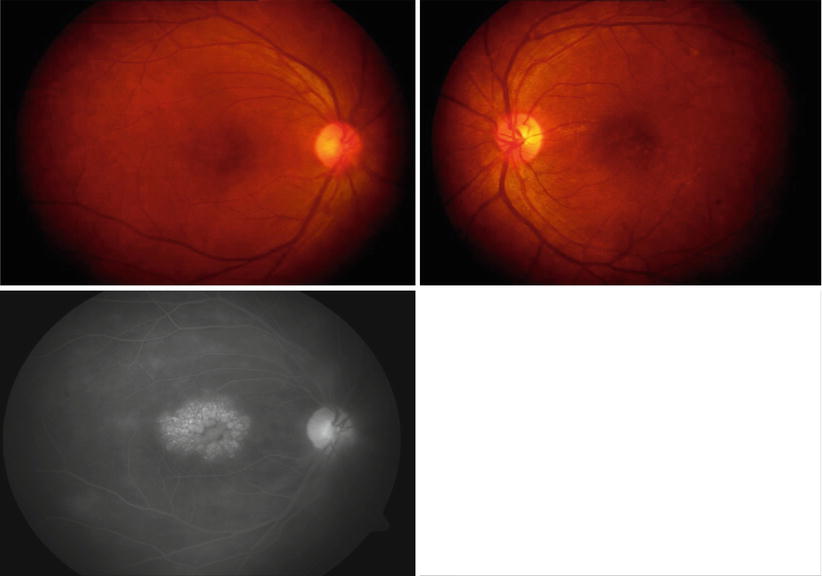
Fig. 11.3
Cystoid macular edema
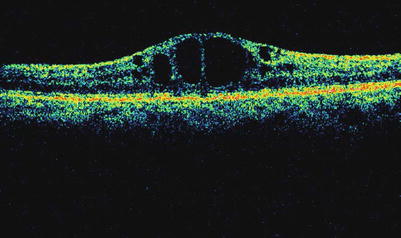
Fig. 11.4
OCT showing cystoid macular edema
4.
Epiretinal membrane: Though rare, this causes irreversible loss of vision in patients with intermediate uveitis. Unlike macular edema, this is not related to duration and severity of the disease [40].
5.
6.
Retinal detachment: Vitreous traction secondary to long-standing vitreous inflammation and subsequent peripheral hole formation will lead to combined retinal detachment in cases of intermediate uveitis [44].
7.
Phthisis bulbi: Total retinal detachments, proliferative vitreoretinopathy, or a cyclitic membrane formation in untreated cases may cause ciliary body traction, detachment and hypotony leading to phthisis bulbi [45].
Differential Diagnosis
Systemic Associations [46]
Infections: Tuberculosis, syphilis, Lyme disease, cat-scratch disease, hepatitis C
Noninfectious disorders: Sarcoidosis, multiple sclerosis, intraocular lymphoma, TINU syndrome
Ocular Differential Diagnosis [47]
1.
Fuchs heterochromic iridocyclitis: Unilateral, stellate diffuse nonpigmented keratic precipitates with vitreous debris. Minimal inflammation with or without posterior subcapsular cataract and/or secondary glaucoma.
2.
Toxocara granuloma: Unilateral, posterior pole, or peripheral granuloma with vitreous membranes and vitritis.
3.
Acute retinal necrosis: Unilateral panuveitis with raised intraocular pressure. Peripheral retina showing necrotizing retinitis with vasculitis and vitritis.
4.
Vogt-Koyanagi-Harada disease: Bilateral granulomatous panuveitis with disk edema and exudative retinal detachment.
5.
Endogenous endophthalmitis: Seen in young patients post fever, intravenous fluids/drugs, dental extraction. Diagnostic vitreous tap will help in diagnosis.
Diagnostic Evaluation
Laboratory tests:
1.
Complete blood count
2.
Erythrocyte sedimentation rate
3.
Mantoux test
4.
QuantiFERON TB GOLD
5.
Serum angiotensin-converting enzyme
6.
VDRL
7.
TPHA
Radiology:
Ancillary tests:
1.
2.
3.
Ultrasound B-scan – In cases where fundus view is limited by posterior synechia and complicated cataract
4.
Treatment
Indications for Treatment
1.
Best corrected visual acuity less than 6/12 in unilateral cases
2.
All bilateral intermediate uveitis irrespective of visual loss
3.
Development of complications of intermediate uveitis
Medical Treatment
Local Therapy
Topical steroids – for spillover anterior uveitis.
Topical NSAIDs – for cystoids macular edema.
Mydriatics – to break the posterior synechiae.
Posterior subtenon injection of triamcinolone acetate(40 mg/0.5 ml) (Fig. 11.5). Complications of periocular injections are increased IOP, cataract, and aponeurotic ptosis.
Fig. 11.5
Technique of posterior subtenon injection
Intravitreals – triamcinolone, dexamethasone, bevacizumab.
Intravitreals for Cystoid Macular Edema in IU
IVTA (intravitreal triamcinolone) – Several of the recent investigations have shown that between 50 and 70 % of patients may benefit for up to 6 months with visual acuity improvement and resolution of CME following a single 4 mg injection of IVTA. Cataract and glaucoma are the documented side effects [58, 59].
Dexamethasone intravitreal implant (Ozurdex) is one of the most potent, with an anti-inflammatory activity that is sixfold greater than that of triamcinolone and 30-fold greater than cortisol. In the dexamethasone implant, the active drug is dispersed through a biodegradable copolymer of lactic acid and glycolic acid (PLGA), forming a matrix structure [60].
Intravitreal bevacizumab (Avastin) seems to be an effective, fast-acting, and safe treatment in the management of inflammatory CME [61].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


