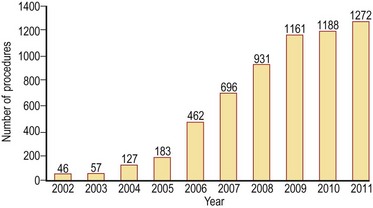
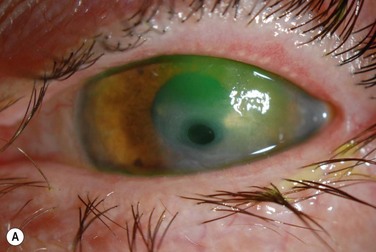
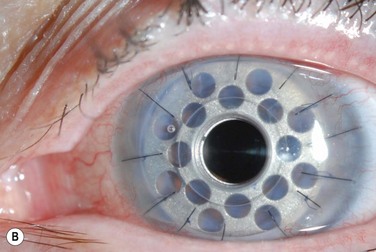
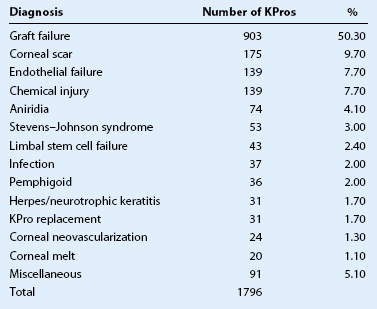
49 In the past, keratoprosthesis implantation was considered a surgery of last resort, fraught with complications and generally poor outcomes. There has been a dramatic increase in the use of the type I Boston keratoprosthesis (Boston KPro) over the last decade as design modifications to the device itself and changes to the postoperative regimen have improved outcomes and reduced postoperative complications (Fig. 49.1). Graft failure remains the most common indication for the Boston KPro (Table 49.1)1. However, in recent years, the Boston KPro has been used successfully as the primary corneal surgery in conditions in which standard penetrating keratoplasty (PKP) has a poor prognosis, including neurotrophic or vascularized host beds (Fig. 49.2), congenital or acquired limbal stem cell deficiency, autoimmune ocular disorders, and pediatric corneal opacities. Cicatricial and inflammatory autoimmune conditions remain the most challenging KPro cases, and need further advances with immunomodulation and improved biologic materials before the Boston KPro will find widespread acceptance as a treatment for these devastating ocular surface diseases.2 Table 49.1 Surgeon-supplied Diagnoses for Type I Boston KPros 2010–2011 2040 KPros were ordered from 1/1/2010 to 12/31/2011. Diagnoses were supplied for 1796 cases. Miscellaneous includes any diagnosis with fewer than 20 cases. The 5-year success rate of corneal grafts in patients with herpetic keratitis is significantly less than that in other corneal diseases, such as keratoconus and corneal dystrophies.3 Anesthesia of the host corneal bed, frequent graft rejection episodes, corneal vascularization and poor wound healing all contribute to the suboptimal outcomes of PKP in the setting of herpetic disease.1 In contrast, case reports and small case series suggest the Boston KPro can be successful in patients with herpes simplex or herpes zoster, even in the setting of corneal anesthesia and active inflammation.3–5 The Boston KPro was used in 17 eyes of 14 patients who had repeatedly failed traditional PKP.3 Twelve patients had herpes zoster or herpes simplex as the initial diagnosis, while two patients had keratoconus and developed herpetic keratitis in the corneal graft. Visual acuity improved from light perception to 20/200 preoperatively to 20/25 to 20/70 in 15 of 17 eyes. No complications were reported in 10 patients over a follow-up period that ranged from 7 to 39 months. The remaining patients experienced complications from pre-existing glaucoma or new-onset sterile vitritis.3 The keratopathy associated with congenital aniridia results from corneal epithelial stem cell deficiency and corneal invasion by conjunctival stem cells causing recurrent erosions, chronic pain, corneal ulceration, scarring, and vascularization.6 Treatment with PKP provides short-term visual rehabilitation, but long-term outcomes are poor, due to underlying stem cell deficiency. Keratolimbal allograft can provide visual rehabilitation but requires systemic immunosuppression.7 The Boston KPro offers another option for the visual rehabilitation of aniridic keratopathy and has the advantage of not requiring immunosuppression. In a retrospective multicenter study of the Boston KPro in aniridia, 14 of 15 patients experienced improved visual acuity from a median of counting fingers to 20/200.6 No KPro extrusions were reported throughout a follow-up period ranging from 2 to 85 months. Preoperative optic nerve and foveal hypoplasia limited the final postoperative vision. Further investigation of the Boston KPro as a standard treatment approach to aniridic keratopathy is underway, and results thus far are encouraging. In pediatric PKP, surgically induced astigmatism hinders visual rehabilitation and amblyopia management.1 In addition, the robust immune response in children leads to an increased risk of immunologic rejection and visually significant corneal neovascularization. The Boston KPro provides rapid visual rehabilitation, thus facilitating amblyopia management in children, and has the additional advantage that there is no risk of rejection. Very few reports of pediatric KPro have been published. Following the initial report of two cases,8
Indications for the Boston Keratoprosthesis
Introduction
Use of the Boston KPro in Herpetic Keratitis
The Boston KPro in Congenital Aniridia
Use of the Boston KPro in Children
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Ento Key
Fastest Otolaryngology & Ophthalmology Insight Engine