PET/CT has revolutionized the evaluation of patients with head and neck cancer by allowing more accurate staging, more focused treatment modalities, earlier detection of recurrent disease, and identification of incurable disease. In some clinical scenarios, PET/CT is clearly useful, while in others the cost may not be warranted. In this chapter, the authors review the literature on the use of PET/CT in head and neck cancers (in particular squamous cell carcinoma) and provide an evidence-based approach to the use of PET/CT for staging, treatment planning, monitoring of treatment response, and surveillance of treated patients with squamous cell carcinoma. They also briefly address the use of PET/CT for thyroid cancer, lymphoma, and melanoma. At the end of each section, key points are summarized in a box for quick reference.
Head and neck cancer accounts for approximately 3% to 5% of all new cancer diagnoses in the United States with 40,000 new cases diagnosed each year . These figures encompass cancers arising from the lip, oral cavity, nasal cavity, paranasal sinuses, pharynx, and larynx, of which the vast majority (90% to 95%) are squamous cell carcinomas arising from mucosal linings of the upper aerodigestive tract. Other, rare cancers that may involve the head and neck include salivary tumors, thyroid cancers, lymphoma, and melanoma.
Early diagnosis and accurate staging are essential for treatment planning and can strongly influence prognosis. Likewise, early identification of tumor recurrence can often be treated with additional surgery or re-irradiation. A combination of history, physical exam, endoscopy, and tissue sampling has historically been the mainstay of diagnosis and staging. The use of cross-sectional imaging (CT and MRI) has greatly improved staging and monitoring for disease recurrence. Small metastases and/or early recurrent disease, however, can still be missed .
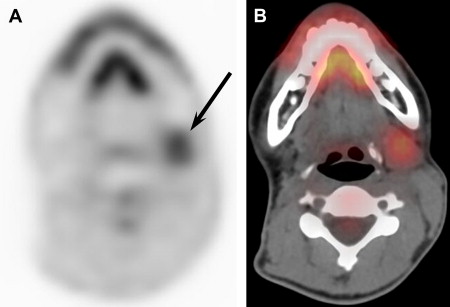
Functional imaging with 18F-fluorodeoxyglucose (FDG) positron emission tomography (PET) can be used to fill these gaps and improve characterization of both primary tumors and metastatic disease. PET has been shown to be effective in the diagnosis of many different types of cancer, including head and neck squamous cell carcinoma (HNSCC) ; however, the poor spatial resolution of PET and the lack of anatomic landmarks can make exact localization of disease difficult. In addition, normal anatomic structures may show variable FDG uptake causing errors in interpretation ( Fig. 1 ). As a result, combined PET/CT scanners have become available that allow for both anatomic and functional characterization of disease at the same time.
PET/CT has revolutionized the staging and surveillance of patients with HNSCC by allowing more accurate staging, more focused treatment modalities, earlier detection of recurrent disease, and identification of incurable disease to avoid overtreatment. The integration of PET and CT is more accurate than either modality alone for the detection of malignancy in the head and neck . There is improved localization of abnormalities, better differentiation of therapeutic changes from residual disease, and improved assessment of tumor extent . There are, however, several potential drawbacks to PET/CT imaging for cancers of the head and neck. Compared with conventional imaging modalities, PET/CT is more expensive. In addition, some cancers of the head and neck do not uniformly accumulate FDG, and potential false positives are numerous .
Staging of HNSCC
Squamous cell carcinomas of the head and neck are staged according to the American Joint Committee on Cancer (AJCC) Staging Manual. Information regarding the primary tumor size and extent (T), regional nodal involvement (N), and distant metastases (M) are synthesized to tabulate a stage allowing for more precise treatment planning and accurate prognostic information .
A combination of history, physical examination by an experienced clinician, endoscopy and tissue sampling with fine needle aspiration (FNA), or core biopsy has been the mainstay for diagnosis and staging of HNSCC, but imaging has now become an integral part of the work-up. Imaging allows for a more clear assessment of degree of infiltration by the primary tumor, involvement of lymph nodes, and detection of distal metastases or second primary tumors. This ultimately improves diagnosis and staging and allows for optimal treatment planning and accurate posttreatment follow-up.
T stage
Criteria for defining the T stage in patients with HNSCC vary slightly according to the site of primary tumor. Generally speaking, accurate and complete assessment of the T stage requires knowledge not only of the size of the primary lesion but also the depth of invasion and involvement of surrounding structures. Imaging with contrast-enhanced CT or MRI has become an essential complement to physical examination and biopsy when assessing the T stage before initiating treatment . CT can provide information regarding the depth of local invasion and infiltration into adjacent structures. In most cases, CT and MRI provide similar information and the decision regarding which modality to use is generally based on a radiologist’s personal preference. MRI is, however, superior to CT for several specific clinical questions such as presence or absence of perineural spread or invasion of bone marrow (see the article by Drs. Ahmad and Branstetter, elsewhere in this issue).
Multiple studies have shown PET to be highly accurate in detection of primary tumors ; however, PET has not been shown to be superior to conventional cross-sectional imaging modalities (CT and MRI). Furthermore, metabolic information alone is not sufficient to provide the information required to accurately and completely stage the primary lesion. Combined PET/CT scanning supplements the functional information with anatomic information from a contrast-enhanced CT. To date, PET/CT has, however, not been shown to be superior to standard anatomic imaging modalities in evaluation of the initial T stage of the primary tumor . Therefore, only patients who are at substantial risk of nodal or hematogenous metastases (T3 or T4) should undergo evaluation with staging PET/CT.
N stage
The spread of disease to regional lymph nodes is the most important prognostic factor in squamous cell carcinoma of the head and neck. With the exception of primary nasopharyngeal cancers, staging for nodal metastases in HNSCC is uniform under the AJCC system. Characteristics that need to be evaluated include the total number of nodes involved, the size of the involved nodes, and the location (unilateral or bilateral and specific levels) and morphology of the nodes involved.
Compared with physical exam, imaging clearly improves the detection of regional lymph node metastases with CT outperforming MRI ; however, no definite criteria exist for identifying metastatic cervical lymph nodes on conventional imaging modalities. Size criteria are the most commonly reported. Smaller thresholds for lymph node diameter result in higher sensitivities at the expense of specificity. In HNSCC, there is high propensity for small lymph nodes to harbor tumor. Even at a commonly accepted threshold diameter of less than 10 mm, most malignant nodes in patients with HNSCC would be missed by conventional imaging modalities thereby understaging patients . Central necrosis, when present, has been shown to be specific for malignancy . It is, however, a later marker of metastatic adenopathy seen primarily in lymph nodes greater than 20 mm in diameter, thereby making it an insensitive indicator of disease on CT . Other criteria used include contrast enhancement with lymph nodes that have a greater degree of enhancement more likely to harbor tumor, and morphology with rounded shape more worrisome than reniform shape.
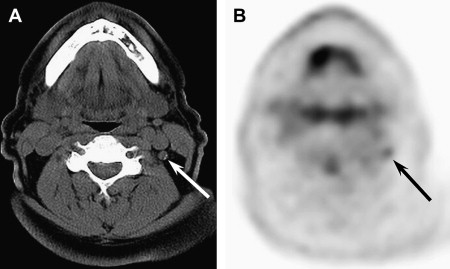
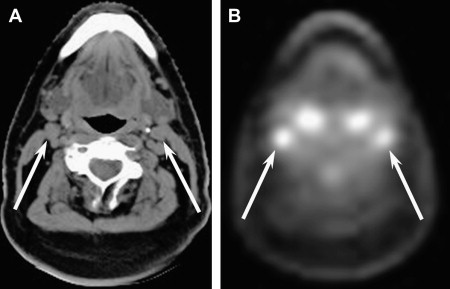
PET has been shown to be superior to conventional imaging modalities for the detection of regional nodal metastases . The increased glucose metabolism can be identified in lymph nodes infiltrated by tumor cells regardless of size criteria. The utility of PET alone is, however, limited by spatial resolution, which makes anatomic localization difficult especially given the complex anatomy within the head and neck. PET/CT bridges this gap by combining metabolic and anatomic information and allows for the most accurate assessment of regional nodal metastases ( Fig. 2 ). In a study of 20 patients with HNSCC, Schwartz and colleagues found PET/CT had an increased sensitivity (96%) for detection of nodal disease compared with CT alone (78%). Similar studies have shown that PET/CT significantly alters TNM scores in patients with HNSCC by identifying nodal disease not apparent by CT, MRI, clinical exam, or combination thereof. Koshy and colleagues found that PET/CT altered the TNM score in 36% of 36 patients compared with CT alone, while Ha and colleagues found that PET/CT altered the TNM score in 31% of 36 patients compared with either CT or MRI. In both of these studies, 7 of the 36 patients (19%) had changes to their N status based on the information garnered from PET/CT but not identified on conventional imaging. Goerres and colleagues found PET/CT altered the TNM score in 15% of 34 patients compared with clinical exam, CT, and chest radiography (in 7/34 patients [21%], the N stage changed). PET/CT is therefore the modality of choice when evaluating HNSCC patients for nodal metastatic disease.
M stage
Approximately 10% to 15% of patients with primary HNSCC will have distant metastases. The most common sites of involvement are the lungs, followed by the liver and skeletal system. The presence of distant metastases may indicate a need for additional therapeutic measures, whereas overlooked distant metastases can lead to inappropriately aggressive treatment . In most patients, distant metastatic lesions will be clinically silent. The following is a list of subsets of patients with HNSCC in whom screening for distant metastases would be indicated .
- •
≥ 4 lymph nodes metastases
- •
Bilateral lymph node metastases
- •
Lymph node metastases ≥ 6 cm
- •
Zone IV lymph node metastases
- •
Recurrent HNSCC
- •
Second primary tumor
Previous screening tests such as chest radiography, serum alkaline phosphatase, and liver function tests have been shown to be insensitive for the detection of distant metastases . Bone scans are of extremely low yield, especially in asymptomatic patients. Chest CT is better than plain radiography but will still miss a significant number of thoracic metastases .
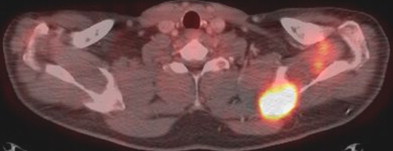
PET has previously been shown to improve detection of occult distant disease for other primary cancers including lung, esophagus, and lymphoma. Studies have showed similar success for patients with primary HNSCC . Limitations of poor spatial resolution and lack of anatomic detail on PET imaging are overcome by integrated PET/CT ( Fig. 3 ). Whole body PET/CT is more accurate than PET alone or traditional cross-sectional modalities for identification of distant metastases. Goerres and colleagues showed that PET/CT found distant metastases or second primaries in 24% of their patients newly diagnosed with SCC of the oral cavity initially screened by clinical exam, CT, and chest x-ray. Similarly, Ha and colleagues found that the TNM score was altered in 31% of their patients with previously untreated HNSCC initially staged with CT or MRI. PET/CT allows for better characterization of equivocal abnormalities on CT by PET and for more accurate anatomic localization of abnormalities on PET by CT . With greater sensitivity than conventional modalities for the detection of metastatic lesions, PET/CT is the modality of choice for staging of patients with advanced HNSCC.
Unknown primary tumors
Patients with HNSCC sometimes present clinically with an enlarging neck mass for which FNA reveals metastatic SCC. In most cases, the primary tumor will be found by physical exam, cross-sectional imaging, or endoscopic evaluation. Despite these efforts, 2% to 9% of patients presenting with nodal metastases will have an occult primary tumor . In these cases, the primary tumor may be too small (<5 mm) to be seen on endoscopy and imaging, or be in a location that may escape notice such as the tonsillar crypts. Likewise, cutaneous primary tumors and tumors outside the head and neck may be overlooked in the customary work-up.
When the primary tumor is found, the patient can be afforded the tissue sparing offered by modern focused radiation therapy techniques. Failure to find the primary relegates the patient to radiation of the entire upper aerodigestive tract, with the attendant morbidity of xerostomia and fibrosis.
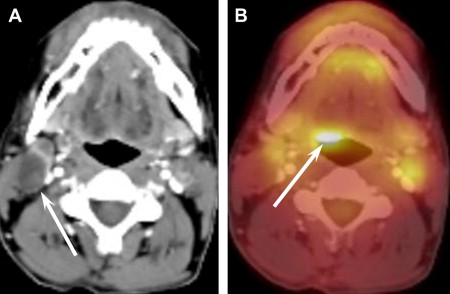
Evaluation of patients with unknown primaries traditionally consists of physical exam, panendoscopy (orophayrnx, hypopharynx, nasopharynx, larynx, and upper esophagus), anatomic imaging with CT and/or MRI, and blind tongue base biopsy. Numerous studies have addressed the ability of PET to identify primary locations after traditional work-up . A meta-analysis by Rusthoven and colleagues showed that PET was able to recognize a primary tumor after negative conventional work-up in one quarter of patients with an overall sensitivity and specificity of 88% and 75%, respectively. In a similar study by Miller and colleagues, PET was able to locate the primary tumor in 31% of patients studied with confirmed squamous cell carcinoma of the cervical lymph nodes and no visible primary tumor. PET was, however, negative in four patients in whom the primary tumor was discovered during routine panendoscopy. PET/CT has not been studied extensively, but is presumed to perform at least as well if not better than PET alone ( Fig. 4 ). A small series found that PET/CT helped identify more primary tumors (33%) than CT (18%) or PET (24%) alone . Despite these promising numbers, there were still false negatives with PET/CT, where the primary tumor was identified by other diagnostic procedures. Therefore, PET/CT is a supplement, not a substitute, for endoscopy and biopsy in the setting of an unknown primary.
The N0 Neck
The spread of disease to lymph nodes is the most important prognostic factor in squamous cell carcinoma of the head and neck. It is estimated that the 10-year survival rate for HNSCC drops from 85% to 10% to 40% in patients with positive lymph nodes. One of the more controversial topics in the management of HNSCC is the clinically node-negative (N0) neck.
An N0 neck means that there is no clinical evidence of metatstatic disease within the neck. This may be based on physical exam of a neck with no palpable adenopathy or be based on a negative radiologic evaluation for cervical metastases. The majority of patients truly do not have metastatic disease within the cervical nodes. There is, however, an approximate 20% risk of occult metastases in patients with a clinically node-negative neck ( Fig. 5 ).
Management of HNSCC with an N0 neck varies among institutions. Some clinicians advocate close observation while others choose to treat the nodes prophylactically, either with lymphadenectomy or external beam radiation. In patients in whom there is a low risk of occult metastases, observation is a reasonable recommendation. Proponents of observation feel that elective treatment of the neck in these patients would put patients through the risk of an unnecessary and potentially morbid procedure, which has not shown an increased survival benefit . Given the risk of occult metastases, many surgeons however feel that an elective neck dissection is a relatively low morbidity procedure which can provide invaluable staging information, the benefits of which outweigh the risk of external beam radiation or having to deal with advanced neck disease after primary treatment.
Recent studies have focused on PET as a diagnostic tool for evaluating the presence of occult metastases. However, these studies have shown that PET is not accurate enough to preclude neck dissection and spare patients this additional procedure ( Table 1 ) . This is likely a reflection of the poor spatial resolution of PET imaging combined with its inability to detect nodal metastases less than 5 mm in diameter. PET/CT has not been studied extensively in the N0 neck but is presumed to perform similarly because of the inherent limitations of PET described previously. PET/CT cannot therefore preclude neck dissection in patients with advanced primaries but clinically node negative necks. Staging Squamous Cell Carcinoma key points below:
- •
T1 disease is unlikely to present with distant metastases, so radiologic staging is not necessary.
- •
T2 disease remains controversial.
- •
Whole-body PET/CT is the modality of choice for staging patients with advanced (T3 and T4) HNSCC.
- •
PET/CT finds 20% to 30% of unknown primary tumors above and beyond the traditional search, but PET/CT is a supplement, not a substitute, for endoscopy and biopsy.
- •
PET/CT is not sufficiently accurate to preclude neck dissection in patients with advanced primaries but clinically node negative (N0) necks.
| Author and Year | No. Patients | Specificity, % | Sensitivity, % |
|---|---|---|---|
| Wensing, et al, 2006 | 28 | 33 | 76 |
| Schoder, et al, 2006 | 36 | 67 | 85 |
| Stoekli, et al, 2002 | 12 | 25 | 88 |
| Myers, et al, 1998 | 12 | 78 | 100 |
Treatment planning
The current standard of care for patients with HNSCC involves combinations of surgery, radiation, and chemotherapy. Although the high doses of radiation used for treatment are effective, there is potential for significant toxicity, which leads to decreased quality of life and diminished patient compliance. Newer treatment modalities such as intensity-modulated radiation therapy (IMRT) and image-guided stereotactic radiosurgery (Gamma Knife and CyberKnife) aim to deliver radiation more efficiently and effectively. Essential to this is accurate delineation of targets. CT and MRI are traditionally used for target definition because of their high spatial resolution. These conventional imaging modalities are unfortunately insufficient for tumor definition in instances where the primary tumors are of small volume. Furthermore, as discussed earlier, CT/MRI criteria for lymph node involvement generally relies on size criteria and therefore diseased nodes may not be included in the radiation field if they are not “pathologically” enlarged.
There has been significant recent interest in the use of integrated PET/CT for radiotherapy planning. When compared with CT, PET/CT has been shown to more accurately assess gross target volume (GTV), which is essential to IMRT . Numerous additional studies have showed similar results . Because of its ability to provide both anatomic and functional information, PET/CT is able to provide for improved tumor coverage and sparing of normal tissues. This ultimately leads to improved treatment response while minimizing adverse effects. Treatment Planning summary below:
- •
PET/CT is superior to conventional imaging modalities for radiation treatment planning, allowing for improved tumor coverage and sparing of normal tissues.
Treatment planning
The current standard of care for patients with HNSCC involves combinations of surgery, radiation, and chemotherapy. Although the high doses of radiation used for treatment are effective, there is potential for significant toxicity, which leads to decreased quality of life and diminished patient compliance. Newer treatment modalities such as intensity-modulated radiation therapy (IMRT) and image-guided stereotactic radiosurgery (Gamma Knife and CyberKnife) aim to deliver radiation more efficiently and effectively. Essential to this is accurate delineation of targets. CT and MRI are traditionally used for target definition because of their high spatial resolution. These conventional imaging modalities are unfortunately insufficient for tumor definition in instances where the primary tumors are of small volume. Furthermore, as discussed earlier, CT/MRI criteria for lymph node involvement generally relies on size criteria and therefore diseased nodes may not be included in the radiation field if they are not “pathologically” enlarged.
There has been significant recent interest in the use of integrated PET/CT for radiotherapy planning. When compared with CT, PET/CT has been shown to more accurately assess gross target volume (GTV), which is essential to IMRT . Numerous additional studies have showed similar results . Because of its ability to provide both anatomic and functional information, PET/CT is able to provide for improved tumor coverage and sparing of normal tissues. This ultimately leads to improved treatment response while minimizing adverse effects. Treatment Planning summary below:
- •
PET/CT is superior to conventional imaging modalities for radiation treatment planning, allowing for improved tumor coverage and sparing of normal tissues.
Monitoring treatment response
Assessment of patients during and after therapy is vital to determine whether an alternate therapeutic approach is needed or whether additional therapy is warranted. Clinical examination is often insufficient to determine the effectiveness of treatment for HNSCC. Conventional cross-sectional imaging studies, while better than clinical examination, are still insensitive to subtle or early changes. Postsurgical and postradiation changes can complicate identification of recurrent or residual disease on physical exam and/or anatomic imaging with CT or MRI . In addition, gadolinium enhancement on MRI can be seen in both residual tumor and treated, tumor-free soft tissues after chemoradiation.
PET alone, without combined CT, has been previously shown to be valuable in monitoring treatment response. It can detect metastatic disease and can be beneficial for differentiating radiation and surgical changes from residual or recurrent tumor because cancer cells retain more FDG for longer periods of time than normal tissues. Poor spatial resolution, however, makes anatomic localization difficult. Recent work has shown improvement using integrated PET/CT ( Fig. 6 ). With sensitivity and specificity of 77% and 93%, respectively, PET/CT had an overall accuracy of 86% for the detection of residual disease, and is superior to contrast-enhanced CT . Similar studies showed PET/CT had sensitivity greater than 90% for localization of recurrent disease . PET/CT is therefore a useful tool for monitoring treatment response in HNSCC and for restaging recurrences including nodal disease and distant metastases.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


