Purpose
To assess eye-specific epiretinal membrane (ERM) incidence 3 years after phacoemulsification surgery, and ERM detection bias attributable to cataract.
Design
Cohort study.
Methods
We recruited 1932 cataract surgical patients aged ≥64 years at Westmead Hospital (2004-2007). The surgical eye of each patient was assessed for presence of cellophane reflex or preretinal fibrosis at preoperative and 1-month-postoperative visits, and annually thereafter, using retinal image grading. Agreement on ERM detection between preoperative and 1-month-postoperative visits was assessed using kappa statistics. Cumulative incidence of ERM from 1 month to 3 years postoperatively was estimated using Kaplan-Meier methods and compared to the 5-year incidence of idiopathic ERM in right eyes of age-matched Blue Mountains Eye Study (BMES) participants.
Results
ERM prevalence was 13.9% among 1394 participants with retinal photographs taken 1 month postoperatively. Of 1040 participants with retinal photographs from both preoperative and 1-month-postoperative visits, ERM was detected in 3.1% and 14.8%, respectively, with low diagnostic agreement (kappa = 0.17). Of 1119 subjects without ERM 1 month post surgery, the 3-year cumulative incidence of ERM was 11.2% (95% confidence interval [CI], 9.4%-13.4%; cellophane reflex 6.6%; preretinal fibrosis 4.2%). The age-standardized 3-year incidence of ERM in the surgical cohort (12.1%, 95% CI 8.6%-16.9%) was higher than the 5-year incidence of the BMES subsample (4.4%, 95% CI 3.0%-6.0%).
Conclusions
A substantial under-detection of ERM in eyes before cataract surgery could incorrectly contribute to ERM incidence after surgery. Over 3 years, ERM developed in >10%, including preretinal fibrosis in 4%, of surgical eyes free of ERM 1 month post surgery.
Epiretinal membranes (ERM) are a frequent, age-related eye condition, occurring in 6%-19% of eyes in persons aged 40 years or older. The ERM prevalence in post–cataract surgical eyes ranged from 17%-28% in previous population-based studies. On fundus photographs, ERM present as 2 forms: cellophane reflex, an early, usually asymptomatic form; and preretinal fibrosis, a more severe form with associated folds. ERM have been shown in previous observational studies to be associated with past cataract surgery. As cataract may obscure a clear view of fundus photographs, ERM prevalence could be markedly underestimated in preoperative eyes and the incidence of new ERM overestimated postoperatively. To assess incident ERM in eyes after cataract surgery, it is necessary to separate the contribution of increased detection from a true increase in the development of ERM in these eyes.
In this study, we aimed to assess detection bias by examining the difference in ERM detection in the same eyes before and after cataract surgery using retinal images taken before and soon after cataract surgery. We also aimed to assess the incidence and progression of ERM over a 3-year period from 1-36 months after phacoemulsification cataract surgery in an older cataract surgical cohort, the Australian Prospective Cataract Surgery and Age-related Macular Degeneration Study. Lastly, we aimed to compare ERM incidence between this cohort (eyes after cataract surgery) and a subsample of the Blue Mountains Eye Study (BMES), who were aged ≥64 years and had not had cataract surgery.
Methods
The Australian Prospective Cataract Surgery and Age-related Macular Degeneration Study is a hospital-based, prospective cohort study of cataract surgical patients aged ≥64 years recruited between 2004 and 2007 from Westmead Hospital, a tertiary referral center, and private ophthalmology clinics in urban districts of western Sydney, Australia. The study adhered to the tenets of the Declaration of Helsinki and was approved by the Human Research Ethics Committees of the University of Sydney and the Sydney West Area Health Service. All patients provided written informed consent. Details of the study have been previously described.
Of 1932 patients recruited for phacoemulsification surgery at Westmead Hospital, 1861 patients had undergone surgery, attended 1-month-postoperative visits, and were then followed annually up to 36 months after their surgery. All patients underwent phacoemulsification surgery with capsulorrhexis (mean diameter 5.2 mm), hydrodissection, and intraocular lens (IOL) implantation. Of the 71 patients who did not attend 1-month-postoperative visits, 63 either had not yet had cataract surgery or had surgery performed elsewhere, 7 withdrew consent before the 1-month visit, and 1 had an undetermined type of eye surgery; thus, they were excluded.
In this report, the following patients were excluded: 110 with preoperative ocular conditions known to predispose to ERM, including moderate-to-severe diabetic retinopathy (modified Airlie House, Early Treatment Diabetic Retinopathy Study [ETDRS] score ≥43), retinal vascular occlusion, and cystoid macular edema; and 256 who did not attend any of the postoperative visits at either 12, 24, or 36 months, which included those who died (n = 72), were too ill (n = 43), refused (n = 101), lived too far away (n = 17), or were uncontactable (n = 23).
Of the remaining 1495 patients, 1394 (93.2%) had retinal images of sufficient quality for analysis of ERM prevalence. Of the 101 (6.8% of 1495) patients who did not have retinal images taken at the 1-month visit, 21 (20.8% of 101) refused photography, and the remainder had no specific reason for the lack of 1-month images.
In order to compare ERM detected preoperatively and 1 month postoperatively in the same eyes, 1040 of the 1394 patients had available images from both visits and thus were included in this analysis. Of the 1394 patients, 193 had ERM at 1 month, and 82 had ungradable retinal images at follow-up visits, leaving 1119 patients who had no evidence of ERM at the 1-month visit but had gradable images at 1 or more follow-up visits to determine ERM incidence.
The BMES is a population-based prospective cohort study of a suburban Australian population aged 49 years or older at baseline. This study also adhered to the tenets of the Declaration of Helsinki and was approved by the Human Research Ethics Committees of the University of Sydney and the Sydney West Area Health Service. All participants provided written informed consent. Survey methods and procedures, including stereo retinal photography, were described elsewhere. In summary, of the 3654 baseline (1992-1994) participants, 2334 (75.0% of 3111 survivors) were reexamined at 5-year follow-up visits (1997-1999). For comparison of ERM incidence in the BMES population with that in the Australian Prospective Cataract Surgery and Age-related Macular Degeneration Study cohort, we selected a subsample of BMES participants aged ≥64 years at baseline who had no ocular pathologies (moderate-to-severe diabetic retinopathy, retinal vascular occlusion, or cystoid macular edema) that predispose to ERM formation, substantial cataract, or cataract surgery (n = 781, 33.5% of 2334). Substantial cataract was defined as presence of nuclear cataract ≥ standard photograph 4 of the Wisconsin cataract grading system, posterior subcapsular cataract graded as ≥5% of the lens area, or cortical opacity ≥25% of the lens area.
Measurements
Eye examinations were conducted preoperatively and at 1, 12, 24, and 36 months postoperatively. Presenting visual acuity (VA), with habitual correction if worn, and pinhole-corrected VA were measured using a back-illuminated logarithm of the minimal angle of resolution (logMAR; Vectorvision CSV 1000, Vectorvision Inc, Dayton, Ohio, USA) chart.
Mydriatic retinal photography of both eyes, including ETDRS standard field 1 (optic disc) and field 2 (macula), was performed at each visit, using a retinal camera (Topcon TRC 50 IA; Topcon Optical, Tokyo, Japan) with Kodachrome 64 35-mm slide film or a mydriatic digital camera (Canon CF-60DSi; Canon, Tokyo, Japan). The classification of ERM lesions was similar to that used in the BMES, which was adopted from the Beaver Dam Eye Study (BDES). ERM were classified into 2 forms: an early and less severe form known as cellophane reflex; and a later form, preretinal fibrosis, that included retinal folds. Eyes with both cellophane reflex and preretinal fibrosis were classified as preretinal fibrosis only. Grading of preoperative photographs and side-by-side grading of the 1-, 12-, 24-, and 36-month photographs taken at the postoperative visits were performed by an experienced grader, with adjudication by a senior researcher (J.J.W.) and a retinal specialist (P.M.).
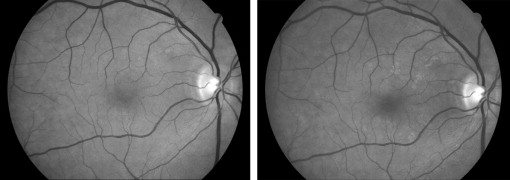
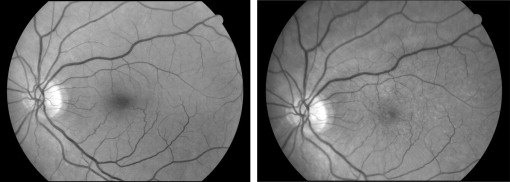
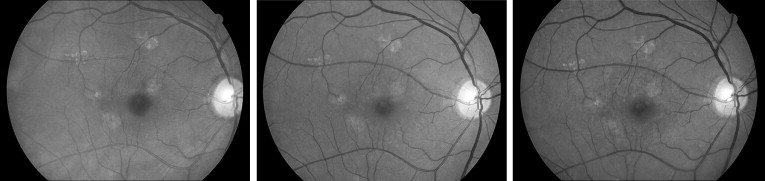
Incidence of ERM was determined if either cellophane reflex or preretinal fibrosis was newly found at any of the annual follow-up visits in operated eyes that had no signs of ERM at baseline ( Figures 1 and 2 ). Progression of ERM was defined when the area of preretinal fibrosis or cellophane reflex was detected to increase by >25% of the initial area from the 1-month visit to any subsequent postoperative visits ( Figure 3 ). Regression of ERM was defined by any of the following criteria: (1) decrease by 25% or more in the area involved; (2) disappearance of ERM; or (3) preretinal fibrosis reverting to cellophane reflex.
Demographic data and a medical history were collected preoperatively and verified against patient medical records.
Statistical Analysis
SAS v 9.13 (SAS Institute Inc, Cary, North Carolina, USA) was used for statistical analyses. The agreement in ERM detection between the preoperative and 1-month-postoperative visits was tested using simple kappa coefficients. Both the prevalence and incidence of ERM were defined using the study (operated) eye of each patient, and only 1 eye of each patient was included in the analyses. For patients who had already had cataract surgery in their first eye before study recruitment, the study eye was the second eye that was operated on after recruitment. The cumulative incidence rates for ERM and their subtypes, cellophane reflex and preretinal fibrosis, from the postoperative 1-month to 36-month period were calculated using Kaplan-Meier (product-limit) estimates. The 36-month cumulative incidence of ERM in eyes after cataract surgery in the Australian Prospective Cataract Surgery and Age-related Macular Degeneration Study was retrospectively compared to the 5-year idiopathic ERM incidence in the right eyes of BMES participants aged 64+ years. Ninety-five percent confidence intervals (CI) were reported.
Results
The mean age of the 1394 patients who attended 1-month-postoperative visits was 74.9 years (standard deviation 5.9 years). Of the 1394 patients, 87.1% (n = 1214) and 77.4% (n = 1079) attended the 24- and 36-month visits, respectively. Apart from age, the preoperative characteristics of the 1394 patients who attended were similar to those of participants who had withdrawn ( Table 1 ).
| Characteristic | Included Participants (N = 1394) | Withdrawn Participants (N = 255) | P Value |
|---|---|---|---|
| Age, mean years ± SD | 74.9 ± 5.9 | 76.4 ± 6.8 | .0013 |
| Female, % | 57.7 | 61.6 | .25 |
| Diabetes, % | 24.6 | 28.6 | .17 |
| Coronary artery disease, % | 22.3 | 27.5 | .070 |
| Prior cataract surgery, % | 25.3 | 26.5 | .69 |
| AMD, % | 16.5 | 13.5 | .26 |
Of 1394 surgical eyes with 1-month-postoperative images, ERM prevalence was 13.8% (n = 193) (cellophane reflex 7.8%; preretinal fibrosis 6.0%). Of 1040 eyes with both preoperative and 1-month-postoperative images, 3.1% (n = 32) and 14.8% (n = 154) were found to have ERM at the preoperative and 1-month-postoperative visits, respectively. Of the 154 eyes with ERM detected at the 1-month-postoperative visit, 87.0% (n = 134) were not detected preoperatively ( Table 2 ). Kappa was 0.17 between ERM detection at the preoperative and 1-month-postoperative visits of the same eyes. Of 146 (14.0% of the 1040) eyes that were classified differently between the preoperative and 1-month-postoperative visits, 65.1% (n = 95) had macula-centered images with poor focus from the preoperative visit, while 15.8% (n = 23) had poor-quality images from the 1-month-postoperative visit.
| 1-Month-Postoperative Participants, N (%) | Total | ||
|---|---|---|---|
| ERM | None | ||
| Preoperative participants | |||
| ERM | a | b | |
| 20 (13.0) | 12 (1.3 a ) | 32 (3.1) | |
| None | c | d | |
| 134 (87.0 b ) | 874 (98.7) | 1008 (96.9) | |
| Total | 154 (100) | 886 (100) Agreement = 86.0% Simple kappa = 0.17 (95% CI 0.10-0.25) | 1040 (100) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


