Immunology of Allergic and Multisystem Diseases That Affect the Eye
Mitchell H. Friedlaender
Hay fever and its ocular manifestation, hay fever conjunctivitis, are allergies to common airborne substances. The pollen of trees, grasses, and weeds and house dust, animal danders, molds, industrial chemicals, and rarely certain foods are responsible for these recurrent and often seasonal allergies. These reactions are a manifestation of type I hypersensitivity and are mediated by immunoglobulin E (IgE). The mucous membranes—nasal or conjunctiva, or both—are affected. Hay fever conjunctivitis is characterized by injection, chemosis, itching, and watery discharge. Conjunctival scrapings contain eosinophils.
Immunopathology
Hay fever (allergic rhinitis) is an immediate hypersensitivity reaction to the environmental allergens mentioned previously, most of which are chemically complex substances derived from plants and animals (Table 34-1). Allergens vary from one geographic area to another, and it is important for the clinician to know which ones are common in his or her region of the country and the time of year that various trees, grasses, and weeds pollinate. Although the related symptoms may occur year-round, they tend to have seasonal peaks of severity. In many parts of the country, ragweed pollen is the most common and most troublesome allergen, particularly between July and mid-October when the plant is pollinating. Air-sampling devices for identifying and quantitating a currently prevalent pollen are available.
Table 34-1. Allergens That Cause Asthma and Rhinitis | ||
|---|---|---|
|
The allergen comes into direct contact with the nasal mucosa or conjunctiva and induces a type I hypersensitivity reaction. It interacts with IgE bound to tissue mast cells and leads to the release of preformed mediators, such as histamine, and synthesized mediators, such as leukotrienes and prostaglandins. These mediators affect blood vessels, smooth muscle, and secretory glands, which in turn are responsible for the clinical manifestations of allergy. The combination of an allergen with a mast cell–bound molecule causes a change in the Fc portion of the molecule attached to the cell membrane. This in turn activates a serine esterase enzyme and initiates a chain of intracellular biochemical events that lead to the physiologic release of mediators. The release of the mediators is inhibited by the elevation of intracellular cyclic adenosine monophosphate (cAMP), the levels of which can be increased by beta-adrenergic stimulation, prostaglandins, and histamine. The release of histamine and other mediators is facilitated by cholinergic stimulation.
The mast cell is structurally and functionally heterogeneous. Different populations of cells may respond differently to physiologic, immunologic, and pathologic stimuli. Two main types of mast cells have been identified in ocular allergic disease based on the relative amounts of two neutral proteases in their cytoplasmic granules.1,2 Tryptase-containing (T) mast cells and tryptase/chymase-containing (TC) mast cells have both been identified in the conjunctiva. In severe allergic conjunctivitis, such as vernal conjunctivitis, both T and TC mast cells increase in numbers and are found throughout the conjunctival stroma and epithelium.3 Most of the mast cells, however, appear to be TC mast cells. Mast cell granules are membrane-bound and contain relatively large amounts of mediators, including histamine, heparin, and tumor necrosis factor alpha (TNF-alpha). They also contain superoxide dismutase, peroxidase, and numerous acid hydrolases, which may act to degrade extracellular matrix.
Inflammatory mediators are secreted by activated cells and serve to trigger or enhance specific aspects of inflammation. Such compounds are said to be proinflammatory, meaning that they promote inflammation. Mediators can be arbitrarily divided into four types: (i) those with vasoactive and smooth muscle contracting properties, (ii) chemotactic factors, which attract other cells, (iii) enzymes, and (iv) proteoglycans. Vasoactive and smooth muscle–constricting mediators are prominent in ocular allergy. Histamine is a preformed mediator and a major mediator of allergic inflammation. It exerts its effect by acting on target cell receptors, known as H1, H2, and H3. H1-related effects are most important in allergies because they mediate bronchiolar smooth muscle contraction and increased vascular permeability. Arachidonic acid metabolites include prostaglandins, leukotrienes, thromboxanes, and lipoxins. These chemicals have various effects but generally promote increased vascular permeability and smooth muscle constriction. Platelet activating factor (PAF) and adenosine have similar effects.
Chemotactic factors attract various kinds of cells to the inflammatory reaction. More than 35 of these factors have been identified. Enzymatic mediators, including tryptase and chymase, are released during mast cell degranulation. They may have an effect on host tissues or interact with the complement and clotting systems. Mast cells are rich in proteoglycans, protein-polysaccharide complexes that form much of the structural matrix of the granules and serve as binding sites for heparin and other mediators.
Eosinophils are a hallmark of the allergic reaction. Although their exact role remains unknown, they have several observed actions that are presumed to be important in the allergic response.5 They may limit the allergic response through the secretion of histaminase, which inactivates histamine, and aryl sulfatase, which inactivates certain leukotrienes. They also contain several toxic substances that may contribute to the pathology and morbidity of the allergic reaction. Proinflammatory mediators derived from eosinophils include major basic protein (MBP), eosinophil cationic protein (ECP), eosinophil-derived neuroprotein (EDN), and Charcot-Leyden crystal (CLC) protein.
Although everyone in a particular environment may be exposed to the same allergens, only atopic subjects develop clinical allergy. The reasons for individual variations in the response to allergens are not entirely clear. It has been suggested that in allergic subjects the nasal mucosa may be more permeable to allergens than in normal subjects, probably because of local edema, vasodilatation, and epithelial hyperplasia.6 In children, there is a striking association between IgA deficiency and allergic disease, possibly because the absence of IgA at the mucosal surface reduces the opsonization and phagocytosis of the allergens.7 These allergens can then stimulate IgG-producing lymphoid tissues.8 There is evidence that genetic factors also play a role in allergic sensitization.9 For example, there is an association between human leukocyte antigen B7 (HLA-B7) and the IgE response to ragweed antigen Ra5; immune-response genes govern antigen recognition at the T-cell level and may account for impaired IgA production. Absence of local defense mechanisms can increase the penetration of allergenic substances and trigger the overproduction that is probably due to excessive T-helper cell activity and a reduced T-suppressor-cell population.10,11
Locally synthesized IgE concentrates on mast cells and basophils in numbers ranging from 10,000 to 40,000. The percentage of occupied receptors per cell is higher in allergic than in nonallergic individuals. The interaction of antigen and cell-bound IgE results in the release of histamine, eosinophil chemotactic factor A (ECF-A), leukotrienes, and PAF. These mediators, which affect local blood vessels and smooth muscle, lead to the typical signs of allergic rhinitis and conjunctivitis.
Recent studies on mouse models of allergic conjunctivitis have provided important insights into the immune regulation of both the early phase reaction and late phase reaction of allergic conjunctivitis. Mounting evidence suggests that IFN-gamma is crucial for optimum expression of allergic conjunctivitis. Costimulatory molecules influence the induction of Th2 immune responses and the early-phase reaction, whereas regulatory T cells shape the expression of the late-phase reaction of allergic conjunctivitis.12 Experimental allergic conjunctival models and clinical research studies have shown that T helper type 2–related mechanisms are definitely involved in the sensitization phase of ocular allergy; however, both T helper type 1 and type 2 cytokines are overexpressed in the active disease, contributing to the development of ocular inflammation.13
Drug Allergy
Drug reactions are too common in medical practice and specifically in ophthalmology. When drugs are used topically, it is often difficult to distinguish between their toxic and allergic side effects. Drug allergy may be caused by any one of four hypersensitivity mechanisms, but type IV (delayed) hypersensitivity reactions are the most common.
Immunopathology
Type I (anaphylactic) hypersensitivity reactions are the most serious and are potentially fatal. They occur within moments after the administration of a drug and are mediated by IgE. The typical clinical manifestations are urticaria and morbilliform eruptions that affect the skin, including the skin of the lids. Other manifestations are hypotension, shock, asthma, and laryngeal edema. Anaphylactic reactions may occur in response to such antibiotics as penicillin and streptomycin. (Penicillin also can cause adverse side effects as a result of types II, III, and IV hypersensitivity reactions.)
Type II (cytotoxic) hypersensitivity occurs when antibody reacts with antigen attached to a target cell. These reactions are complement dependent. Usually a complex that contains drug, antibody, and complement becomes fixed to the cell membrane, and this leads to lysis of target cells (leukocytes or platelets). Type II reactions can be induced by penicillin, methyldopa, sulfonamides, quinidine, or incompatible blood transfusions.
Type III (immune-complex) hypersensitivity drug reactions may lead to urticaria, serum sickness, or a multisystem, complement-dependent vasculitis. Immune complexes are deposited within tissues, especially blood vessels, and the complement pathways are activated, resulting in local inflammatory foci. Bilateral iritis has been described in a patient who developed serum sickness after a series of injections of antipneumococcal horse serum for pneumonia, and a similar type of uveitis has been produced experimentally in the rabbit.14
Type IV (delayed) hypersensitivity drug reactions are commonly encountered as contact allergies to topical medications. In ophthalmology, allergies of this type often are reactions to topical antibiotics, anesthetics, dilating agents, and certain drug preservatives.
Cytokines are thought to play a role in acute and/or immune-mediated adverse drug reactions due to their ability to regulate the innate and adaptive immune systems. This role is highly complex owing to the pluripotent nature of cytokines, which enables the same cytokine to play multiple roles depending on target organ(s) involved.15
Serum Sickness
Serum sickness is a type III hypersensitivity reaction in which immune complexes are deposited in various tissues. It usually follows the injection of heterologous proteins.16 Antitoxins, such as those prepared for the treatment of diphtheria, rabies, snake venom, and clostridial infections, may produce this type of reaction, and certain drugs, such as penicillin and the sulfonamides, also have been implicated. The signs and symptoms appear 1 or 2 weeks after the injection of a foreign protein and include arthritis, fever, urticaria, lymphadenopathy, splenomegaly, occasionally glomerulonephritis and laryngeal edema, and various ocular lesions.14,17 Immune complexes are thought to be deposited in the uveal tract (as in the kidney and synovial membranes), where they fix complement and attract inflammatory cells. Bilateral anterior chamber and keratic precipitates may be seen. Serum sickness iritis has been reported after an injection of antipneumococcal horse serum (for pneumococcal pneumonia) or an injection of tetanus antiserum.
Laboratory studies demonstrate an elevated sedimentation rate, leukocytosis, hematuria, proteinuria, and low levels of serum complement. The disease is usually self-limited and free of complications. Urticaria can be treated with epinephrine and antihistamines. Arthritis usually responds well to salicylates. If the patient is severely ill, a short course of systemic corticosteroids can be given. Uveitis responds well to topical corticosteroids and dilating drops. A patient described by Theodore and Lewson14 developed bilateral iritis in association with generalized serum sickness on two occasions, 9 days and 30 days after a series of inoculations with antipneumococcal horse serum for pneumonia.1 Wong et al18 produced in a rabbit experimental uveitis similar to the uveitis described in serum sickness.
Sarcoidosis
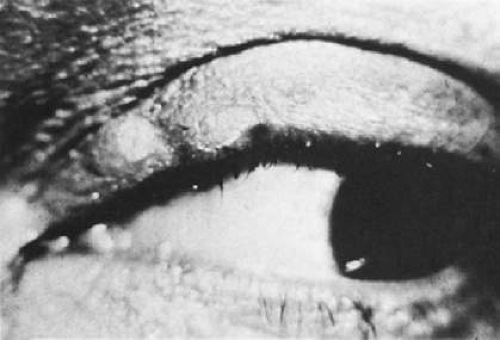
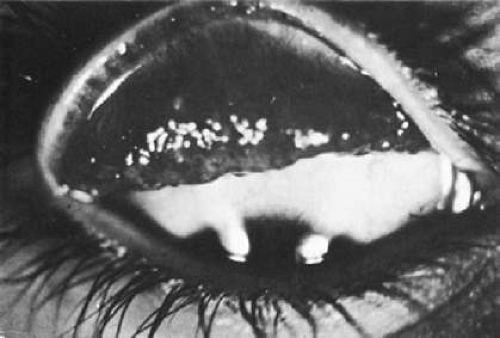
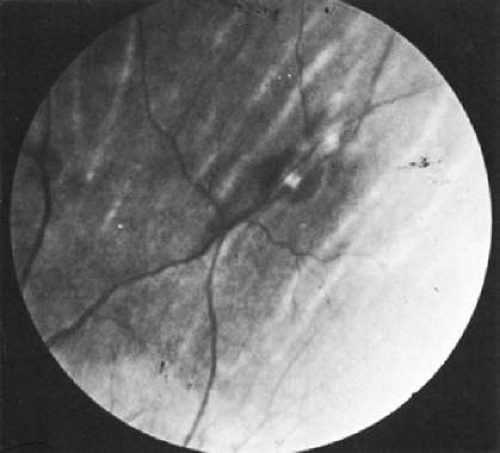
Sarcoidosis is a multisystem disease of unknown cause but with various immunologic defects. It can affect almost any organ, but the principal targets are the lungs and lymph nodes. Ocular lesions—most commonly iridocyclitis, but also eyelid and conjunctival nodules, keratitis, and retinal, optic nerve, and orbital lesions—occur in approximately 26% of cases (Figs. 34-1, 34-2, 34-3, 34-4, 34-5). An ocular syndrome with the characteristics of sarcoidosis but lacking systemic disease also has been seen. Sarcoidosis is a noncaseating granulomatous disease, likely of autoimmune etiology, that causes inflammation and tissue damage in multiple organs, most commonly the lung, but also skin, and lymph nodes. Reduced dendritic cell (DC) function in sarcoidosis peripheral blood compared with peripheral blood from control subjects suggests that blunted end organ cellular immunity may contribute to sarcoidosis pathogenesis. Successful treatment of sarcoidosis with tumor necrosis factor (TNF) inhibitors, which modulate DC maturation and migration, has also been reported. Together, these observations suggest that DCs may be important mediators of sarcoidosis immunology.19
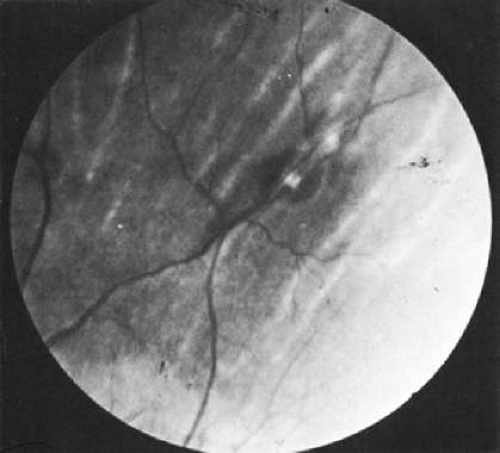 Fig. 34-5. Conjunctival biopsy in sarcoidosis showing granuloma formation. (Courtesy of Dr. R. Weinberg.) |
Immunopathology
Although various agents, including mycobacteria, pine pollen, organic dusts, beryllium, fungi, and viruses, have been linked with sarcoidosis, its cause remains unknown. It is often classified as an immunologic disorder because of the characteristic alterations in cell-mediated immunity associated with it.20,21,22 It still is not known, however, whether sarcoidosis is the result of an immunologic disturbance or whether the immunologic disturbances are secondary to widespread lymph node inflammation from another cause or causes. A slow virus remains an etiologic possibility, but viral isolation attempts have been unsuccessful.23 Recently a transmissible agent, possibly mycobacterial or viral, that was isolated from human sarcoid tissue homogenates has produced epithelioid and giant cell granulomas in the footpads of mice. The ability to produce granulomas is destroyed when the homogenates are autoclaved.
Immunologic features of sarcoidosis include (i) accumulation of T cells and monocyte-macrophage populations, (ii) activated CD4 T cells, (iii) polyclonal gammopathy, and (iv) depressed cellular immunity. Activated CD4 T cells spontaneously release interferon gamma, interleukin-2, and other cytokines, producing many T cells through chemotaxis and mitogenesis at the site of disease24
There are three types of immunologic abnormalities in sarcoidosis: (i) depression of delayed hypersensitivity, (ii) lymphoproliferation with increased serum gamma globulins, and (iii) granulomatous reactions. Depression of delayed hypersensitivity is a well-known feature of sarcoidosis. The reactivity of the skin to a variety of antigens—mumps, tuberculin, dinitrochlorobenzene (DNCB), pertussis, and keyhole limpet hemocyanin (KLH)—is depressed or absent.20 This suggests a T-lymphocyte–mediated anergy and impaired cellular immunity. The tuberculin skin test is negative in two thirds of patients with sarcoidosis (although it may become positive when the disease resolves), and most patients cannot be sensitized to either DNCB or KLH.20 Whether this impaired delayed hypersensitivity in sarcoidosis is due to an abnormality of circulating T lymphocytes or to circulating serum inhibitors is still unknown.
Most in vitro studies of sarcoidosis show depressed T-cell function and overactive B-cell function.20,25 When the lymph nodes are affected, the circulation of T lymphocytes may be impaired, and this may contribute to the lowering of the T-cell counts.26 Lymphocytes from patients with sarcoidosis respond less actively to the mitogen phytohemagglutinin than do the lymphocytes of other subjects, but during remission this response is restored.27 The lymphocytes also show a greater spontaneous blastogenic response in vitro, especially after they have been cultivated for 5 to 7 days. This phenomenon is associated with the release of lymphokines, and recently serum migration inhibition factor (MIF) was detected in affected patients. As a result, attempts have been made to establish an in vitro test for sarcoidosis based on MIF production.28 However, although inhibition takes place when sarcoid spleen is used as an antigen, the lymphocytes of some of the controls also are positive. The results of other attempts to produce MIF with Kveim antigens and lymphocytes from sarcoid patients also have been mixed, and the fact that lymphocytes from patients with Hodgkin disease and tuberculosis also respond positively may limit the usefulness of MIF production as a test for sarcoidosis.
In contrast to the depressed cellular immunity in sarcoidosis, antibody production is overly active. During active disease the levels of IgG, IgA, and IgM are elevated. As soon as there is clinical improvement, the levels of IgG and IgM drop back to normal, but the IgA level usually remains elevated. High levels of circulating antibody to Epstein-Barr virus and the viruses of herpes simplex, rubella, measles, and parainfluenza have been reported.29,30
False-positive results in other serologic tests and abnormally severe antibody reactions to mismatched blood also have been described.31 Serum IgD levels are either normal or elevated (although in middle-aged patients they may be depressed), and serum IgE levels are significantly elevated.32,33,34 Elevated immunoglobulin levels are the rule in the bronchial secretions of sarcoidosis patients but also have been noted in various other diseases. There is no evidence that patients with sarcoidosis have any particular HLA type.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree