Purpose
To investigate the immunohistochemical features of ocular adnexal pleomorphic adenoma and adenoid cystic carcinoma.
Design
Retrospective clinicopathologic study.
Methods
Clinical records and microscopic slides of 7 cases of each tumor type were reviewed. Immunohistochemical probes for Ki-67 and p53, and newer nuclear markers MYB for adenoid cystic carcinoma and PLAG1 for pleomorphic adenoma, were employed.
Results
Pleomorphic adenomas were asymptomatic, whereas adenoid cystic carcinomas were painful. No pleomorphic adenomas recurred; 4 adenoid cystic carcinomas recurred, resulting in 3 deaths. Unusual histopathologic variants for which immunohistochemistry proved useful included a myoepithelioma, an atypical pleomorphic adenoma, tubular and solid/basaloid variants of adenoid cystic carcinoma, and a morphologically heterogeneous adenoid cystic carcinoma of a Wolfring gland. For the pleomorphic adenomas, the average Ki-67 proliferation index was 3.8%; p53 was weakly staining, with an average positivity of 18.5%; PLAG1 was strongly positive in all cases; MYB was negative in 5 cases and weakly focally positive in 2 cases. For the adenoid cystic carcinomas, the average Ki-67 proliferation index was 29.1%; p53 stained positively and strongly with an average of 39%; none stained positively for PLAG1; and 6 out of 7 were MYB positive.
Conclusions
Between pleomorphic adenoma and adenoid cystic carcinoma, there was no overlap in Ki-67 positivity. Positivity for p53 showed overlap in only one lesion of each type. PLAG1 and MYB positivity were highly discriminating between pleomorphic adenoma and adenoid cystic carcinoma. Immunohistochemical analysis should be investigated further for its role in the evaluation of pleomorphic adenoma and adenoid cystic carcinoma.
In comparison with salivary gland epithelial tumors, the immunohistochemical study of those of the lacrimal glands (both major and accessory) is a neglected subject. The present article, based on the investigation of 14 benign and malignant lacrimal gland epithelial tumors, is intended to establish a baseline for a set of immunohistochemical markers that in certain circumstances could provide assistance in the diagnosis of difficult or controversial cases. Examples might include discrepant diagnostic opinions encountered with small piecemeal excisions, needle biopsies, recurrent tumors, mesenchymal and neurogenic spindle cell tumors distinct from myoepitheliomas, invading carcinomas from surrounding compartments, and metastases in the lacrimal fossa region. Benign and malignant epithelial tumors with ambiguous or aberrant morphologic features, such as an atypical pleomorphic adenoma displaying internal worrisome cytologic features; tumors with overlapping sclerotic stromas; adenoid cystic carcinoma or poorly differentiated carcinoma arising in situ within the capsular confines of a pleomorphic adenoma; infiltrative carcinoma arising in a pleomorphic adenoma (also called carcinoma ex pleomorphic adenoma or malignant mixed tumor); and adenoid cystic carcinoma with fields imitating a pleomorphic adenoma or a basaloid monomorphic tumor (adenoma) must also be considered separately. We have selected two well-established probes for estimating the degree of atypicality in lacrimal epithelial tumors: Ki-67 for DNA synthesis prior to mitosis and aberrant p53 suppressor gene protein; and two newer markers, PLAG1 for supporting the diagnosis of pleomorphic adenoma and MYB for adenoid cystic carcinoma. We preliminarily outline an immunopathologic approach based on our findings for the diagnosis of benign and malignant lacrimal gland epithelial tumors.
Methods
This retrospective study was conducted under the auspices of the Massachusetts Eye and Ear Infirmary Institutional Review Board (protocol # 13-034) and in compliance with the rules and regulations of the Health Insurance Portability and Accountability Act and in adherence to the Declaration of Helsinki and all relevant federal and state laws. The cases were identified by searching through the records of the David G. Cogan Laboratory of Ophthalmic Pathology at the Massachusetts Eye and Ear Infirmary from 2007 to 2013 for lacrimal gland and orbital specimens with diagnoses of adenoid cystic carcinoma (7 cases) and pleomorphic adenoma or benign mixed tumor (7 cases). The clinical records, clinical photographs, radiologic imaging studies, and operative reports were reviewed. Archived tissue blocks with adequate remaining tissue for additional staining of slides were available for all cases selected for inclusion. Tumor sections were stained with hematoxylin and eosin, periodic acid Schiff, and mucicarmine. Formalin-fixed, paraffin-embedded specimens were used to prepare 5-μm sections for immunohistochemical staining. The immunoperoxidase method was applied with appropriate controls to validate antibody quality. The following probes were utilized: MYB (clone EP769Y; Epitomics, Burlingame, California, USA; 1:200); PLAG1 (mouse monoclonal; Abnova, Taipei, Taiwan; 1:150), both processed at the Department of Pathology, Brigham and Women’s Hospital, using a Dako autostainer; p53 (mouse monoclonal; Leica Biosystems, Newcastle, UK; prediluted); and Ki-67 (mouse monoclonal, Dako, Carpinteria, California, USA; 1:200), employing a Leica Bond III autostainer, both processed at the Diagnostic Immunopathology Laboratory, Massachusetts General Hospital, Boston. The chromogen diaminobenzidine was used and the tissues were counterstained with hematoxylin. MYB and PLAG1 staining were initially evaluated blindly by a single pathologist (J.F.K.) and confirmed by another (F.A.J.). Staining in >50% of tumor cells was scored as strongly positive, >5 and <50% of cells as weakly positive, and <5% of cells as negative. Specific cell counts for nuclear positivity were performed for Ki-67 and p53 in two high-power fields, and the results were averaged.
Results
Clinical Findings
The clinical features of the cases involved in this study are summarized in Table 1 for the pleomorphic adenomas and Table 2 for the adenoid cystic carcinomas. Among the cases of pleomorphic adenoma, three were male and four were female ( Figure 1 , top left). The mean age at presentation was 47 years. Five patients presented with an upper eyelid mass, two had mild proptosis (2 mm), and one had lateral upper eyelid ptosis. The mean duration of symptoms was 39 months. Radiologic imaging showed a well-defined, rounded mass; one lesion displayed intralesional foci of calcification but without major bone changes ( Figure 1 , top right). Another tumor occurred as an enlargement of the palpebral lobe of the lacrimal gland, which was readily visible on physical examination with eyelid eversion. The first surgery in all cases was an attempt at complete excision, and an incisional biopsy was studiously avoided. No patient has experienced a recurrence, with an average follow-up of 15 months. However, only one of the seven cases had a follow-up of longer than 3 years (37 months).
| Case # | Age/Sex | Laterality | Visual Acuity | Symptoms/Duration | Radiologic Findings | Treatment | Length of Follow-up (months) | Outcome |
|---|---|---|---|---|---|---|---|---|
| 1 | 55/M | Left | 20/20 | Proptosis (2 mm); 6 mo | Well-demarcated, round, lobulated mass with calcific foci; slightly enlarged orbit | Tumor resection | 37 | No evidence of recurrence |
| 2 | 51/F | Right | 20/20 | Eyelid mass and swelling, ptosis; 60 mo | No imaging studies done | Tumor resection | 14 | No evidence of recurrence |
| 3 | 18/F | Right | 20/20 | Eyelid mass; 60 mo | Well-demarcated, round mass | Tumor resection | 4 | No evidence of recurrence |
| 4 | 55/M | Right | 20/20 | Eyelid mass; 12 mo | Well-demarcated, round mass | Tumor resection | 12 | No evidence of recurrence |
| 5 | 69/F | Left | 20/25 | Eyelid mass; 96 mo | Well-demarcated, round, lobulated mass | Tumor resection | 13 | No evidence of recurrence |
| 6 | 54/M | Left | 20/25 | Proptosis (2 mm); 24 mo | Enlargement of palpebral lobe of lacrimal gland | Tumor resection | 14 | No evidence of recurrence |
| 7 | 28/F | Right | 20/20 | Eyelid mass; 12 mo | Well-demarcated, round, lobulated mass; bone indentation | Tumor resection | 8 | No evidence of recurrence |
| Case # | Age/Sex | Diagnosis/Laterality/TNM Staging | Visual Acuity | Symptoms/Duration | Radiologic Findings | Treatment | Length of Follow-up (months) | Outcome |
|---|---|---|---|---|---|---|---|---|
| 8 | 10/F | ACC of lacrimal gland, right (T2N0M0) a | 20/20 | Proptosis (2 mm), eyelid swelling; 5 mo | Irregular mass with calcific foci | Tumor resection + radiotherapy | 132 | Recurrence after 10 yrs treated with surgery + brachytherapy (placement of radiation catheters); alive |
| 9 | 53/F | ACC of lacrimal gland, right (T4bN0M0) | 20/20 | Proptosis (4 mm), pain, globe displacement, diplopia; 1 mo | Irregular mass with bony destruction | Tumor resection with bone removal + radiotherapy | 25 | Recurrence after 1 yr; alive |
| 10 | 59/M | ACC of lacrimal gland, right (T4bN0M0); HIV infection | 20/30 | Pain, eyelid swelling, ptosis; 6 months | Irregular mass with bony erosion | FNAB b + tumor resection + radiotherapy + chemotherapy | 53 | Lung metastasis after 2 yrs; died of disease |
| 11 | 89/M | ACC of lacrimal gland, left (T4bN0M0) | 20/25 | Proptosis (2 mm), ptosis; 7 months | Irregular mass with bony erosion | Tumor resection + radiotherapy | 84 | Recurrence after 6 yrs treated with exenteration; died of disease |
| 12 | 50/F | ACC of lacrimal gland, left (T4bN0M0) | 20/20 | Proptosis (3 mm); 4 mo | Irregular mass with bony destruction | Tumor resection with bone removal + radiotherapy | 178 | Recurrence after 9 years treated with tumor resection + proton beam radiotherapy; alive |
| 13 | 37/M | ACC of accessory lacrimal gland, right (T1N0M0) | 20/20 | Eyelid mass and swelling; 1 month | Well-demarcated mass in inferolateral orbit | Incisional biopsy + tumor resection + radiotherapy | 9 | No evidence of recurrence; Alive |
| 14 | 27/M | ACC of maxillary sinus and orbit, right (T4bN2cM0) | 20/20 | Pain, proptosis (7 mm) diplopia; 23 months | Tumor in maxillary sinus and orbit with bony destruction | Incisional biopsy + radiotherapy | 15 | Brain metastasis after 1 year; died of disease |
a ACC, adenoid cystic carcinoma; T, tumor, N, node, M, metastasis; T, size and extent of tumor; N, regional lymph node metastasis; M, distant metastasis (Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. American Joint Committee on Cancer Staging Manual, 7th ed. New York: Springer, 2010:569-576).
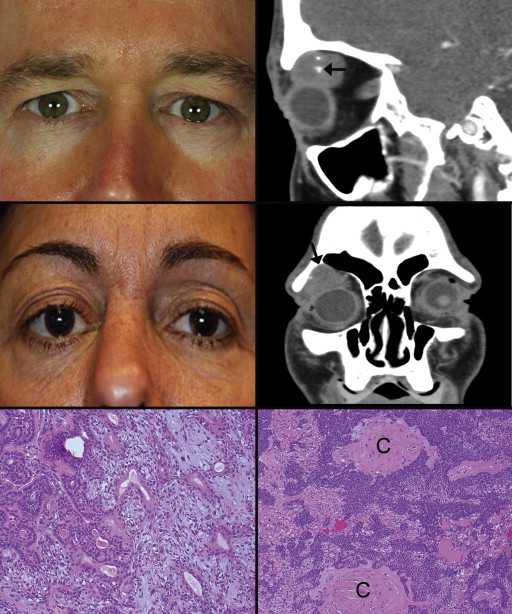
Five adenoid cystic carcinomas arose in the major lacrimal gland, one in an accessory lacrimal gland of Wolfring in the lower eyelid, and one in the maxillary sinus with secondary orbital extension. The American Joint Committee on Cancer (AJCC) TNM (tumor, node, metastasis) classification for each tumor is given in Table 2 . Four patients were male and three were female, with a mean age at presentation of 46 years ( Figure 1 , middle left). Five patients manifested proptosis (2 to 7mm), three complained of pain, and two had diplopia. The mean duration of symptoms was 7 months. Radiologic imaging showed bony destruction, erosion or remodeling of the orbital roof in four of the five lesions arising in the lacrimal gland ( Figure 1 , middle right). The orbital floor and medial wall in the primary maxillary tumor invading the orbit were partially destroyed. There were no bony changes in the tumor arising in the accessory gland of Wolfring. One tumor contained intralesional calcification without adjacent bony changes. The patient with the adenoid cystic carcinoma primarily in the maxillary sinus with orbital extension was the only patient who had regional lymph node involvement at the time of initial presentation. In all cases, a malignancy was strongly suspected based on the clinical and radiologic findings, and the widest excision possible was undertaken in the face of infiltrative margins. Average follow-up has been 71 months. Tumor recurrence has been found in four patients. Four patients are alive with disease and three have died as the result of their disease.
Histopathologic Findings
The diameters of the pleomorphic adenomas ranged from 1.2 cm to 2.6 cm, with a mean of 1.6 cm. All were invested with a variably thick pseudocapsule and all but one of the lesions were composed of a mixture of double-layered, epithelium-lined glandular structures with small to patulous lumens ( Figure 1 , bottom left) and spindly outer myoepithelial cells. The lumens commonly contained amorphous, eosinophilic secretory material that was positive for periodic acid Schiff (PAS) and mucicarmine. Basophilic mucoid stromal material surrounded the ductlike units. The outer myoepithelial cells of the ductular structures delaminated into the stroma. One myoepitheliomatous tumor predominantly displayed non-lumen–forming oval and spindle-shaped cells. This variant manifested stromal regions of compacted collagen ( Figure 1 , bottom right). One lesion was remarkable because of its scattered, atypical, hyperchromatic spindle cells ( Figure 2 , top left) and atypical low cuboidal cells, which created micro-acinar units ( Figure 2 , top right and inset). Another tumor exhibited foci of dystrophic calcification.
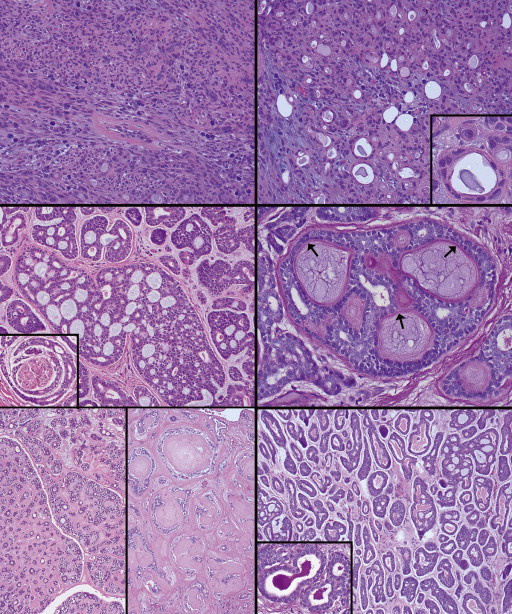
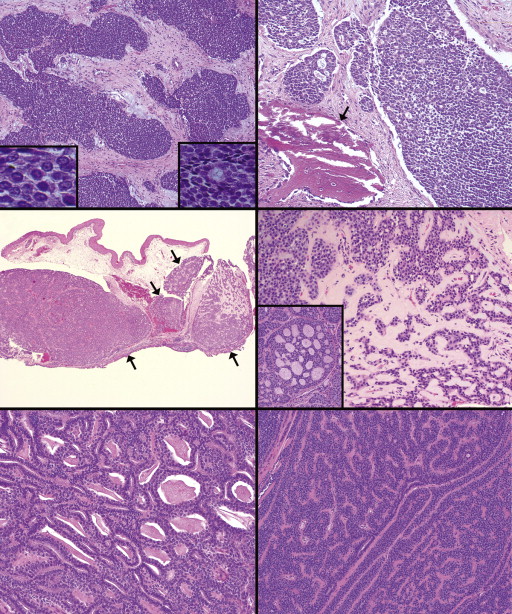
Of the five adenoid cystic carcinomas arising primarily in the main lacrimal gland, the widest diameters of the lesions ranged from 1.4 cm to 3.1 cm, with a mean of 2 cm. The lesions were removed only exceptionally as single specimens and more typically fragmentarily. The outer perimeters of some lesional fragments possessed only thin partial pseudocapsules that were commonly infiltrated by small islands of tumor cells. Five tumors had a combination of cribriform ( Figure 2 , middle left and middle right) and tubular patterns; one cribriform lesion was reduced to small tumor cell clusters with pseudolumens or curvilinear strands by a prominent enveloping and compressive hyaline stroma ( Figure 2 , bottom left, left and right panels); one lesion in the sinus had a trabecular pattern occasionally punctuated by minute lumens; one had a predominantly tubular pattern ( Figure 2 , bottom right); and one had a predominantly solid/basaloid pattern ( Figure 3 , top left and top right). A final tumor manifested a mixture of the most unusual features: subconjunctival multinodularity due to its origin in an accessory gland of Wolfring in the lower lid tarsus ( Figure 3 , middle left); small lumen-forming cellular clusters suggestive of a pleomorphic adenoma ( Figure 3 , middle right); tightly packed tubular structures ( Figure 3 , bottom left); and interanastomosing cords of small, banal, basaloid cells encountered more typically in extremely rare monomorphic adenomas ( Figure 3 , bottom right). In lesions with a tubular pattern, the true lumens focally contained PAS and mucicarmine-positive eosinophilic secretions ( Figure 2 , bottom right inset). Evidence of perineural invasion was seen in three cases ( Figure 2 , middle left inset).
Immunohistochemical Findings
The immunohistochemistry results of nuclear staining with the four probes are summarized in Table 3 . The Ki-67 proliferation index for the pleomorphic adenomas ( Figure 4 , top left) was relatively low with an average of 3.8% (range of 2.6% to 5.4%). The average Ki-67 proliferation index for adenoid cystic carcinomas ( Figure 4 , top right) was 29.1% (range of 23.8% to 42.5%). The basaloid variant had the highest Ki-67 positivity of 42.5% ( Figure 4 , top right inset). p53 in the pleomorphic adenomas ( Figure 4 , middle left) displayed an average positivity of 18.5% (range, 11.9% to 28.9%). The average p53 positivity in the adenoid cystic carcinomas ( Figure 4 , middle right) was 39% (range, 24.2% to 50.3%). Two cases (the solid/basaloid adenoid cystic carcinoma and the adenoid cystic carcinoma originating in the maxillary sinus) were totally negative for p53, possibly an artifactual finding. In all specimens of pleomorphic adenoma, PLAG1 stained strongly positive in the outer ductular myoepithelial cells and spindled stromal cells ( Figure 4 , bottom left and bottom right). The adenoid cystic carcinomas were all negative for PLAG1 ( Figure 5 , top left). None of the pleomorphic adenomas stained strongly positive for MYB: two cases stained focally and weakly positive for MYB, and five cases were totally negative, including the myoepitheliomatous variant ( Figure 5 , top right and middle left). In six cases of adenoid cystic carcinoma, tumor cells stained strongly positive for MYB ( Figure 5 , middle right, bottom left and bottom right), whereas one case was negative. Positive staining was seen in both the outer myoepithelial cells and the inner luminal cells in cases with mixed tubular-cribriform and predominantly tubular patterns. MYB staining was diffuse and uniform within the solid lobules of cells of the basaloid tumor ( Figure 5 , bottom right).
| Ki-67 Proliferation Index (Mean [Range]) | P53 Positivity (Mean [Range]) | PLAG1 (Positive/Negative) | MYB (Positive/Negative) | |
|---|---|---|---|---|
| Pleomorphic Adenoma (n = 7) | 3.8% [2.6 − 5.4%] | 18.5% [11.9 – 28.9%] | 7 b /0 | 2 c /5 |
| Adenoid Cystic Carcinoma (n = 7) | 29.1% [23.8 – 42.5%] | 39% [24.2 – 50.3%] a | 0/7 b | 6 b /1 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


