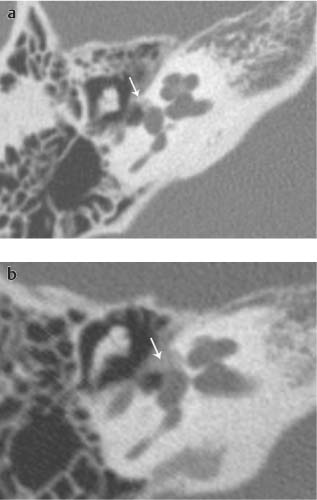
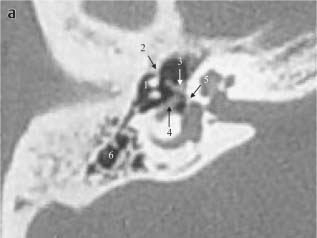
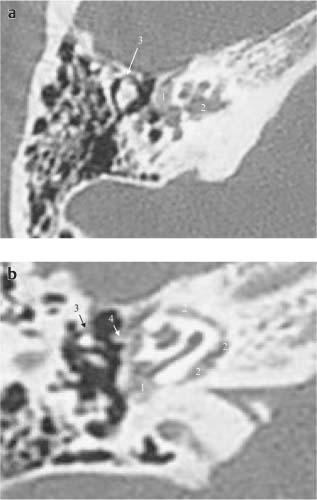
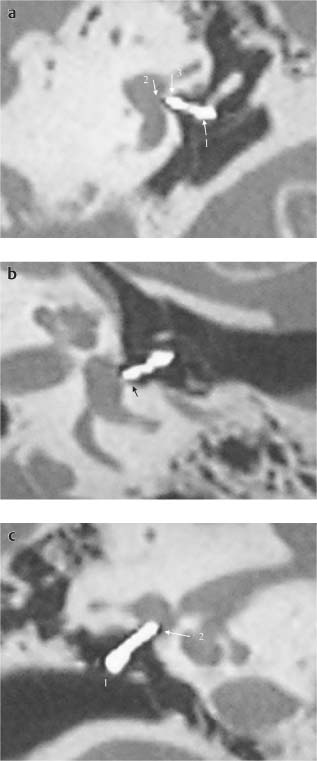
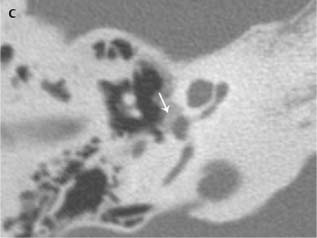
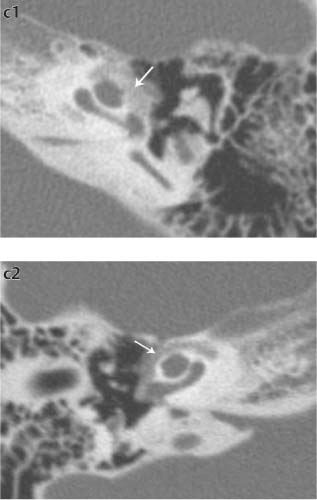
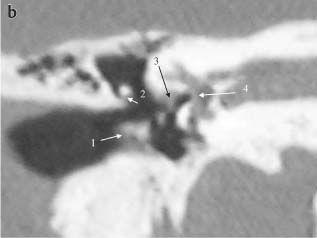
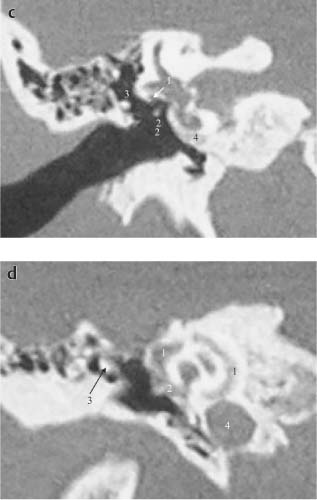
Chapter 11 Imaging for Stapes Surgery High-resolution computed tomography (HRCT) with 0.5-mm slices permits visualization, location, and quantification of an otosclerotic focus in 74% of patients with a clinically suspected otosclerosis. Multi-planar reconstruction on a workstation increases the rate of detection to 85%. A recent study (Naumann et al. 2005, 19-R) has shown that there is a correlation between the size of the otosclerotic focus and the extent of the conductive hearing loss but no correlation between the otosclerotic cochlear involvement and the extent of the sensorineural hearing loss (Figs. 185a–c and 186a–c). Fig. 185 Classification of fenestral otosclerotic foci without cochlear involvement into three classes according to size. Radiologically the visible otosclerosis should be called otospongiosis because the ossified “otosclerotic” focus may be indistinguishable from the other bone. Axial HRCT scans, right ear (key level: oval window). a Otospongiosis limited to fissula ante fenestram (Class 1). b Otospongiosis involving the anterior half of the oval window and cochleariform process (Class 2). c Otospongiosis extending over entire oval window niche (Class 3). Fig. 186 Classification of cochlear otosclerosis according to size (three classes). a Otospongiosis not exceeding diameter of one cochlear turn (Class 1). Left axial HRCT scan (key level 1: oval window). b Otospongiosis invading more than one cochlear turn but not involving entire otic capsule (Class 2). Left axial HRCT scan (key level 1: oval window). c2 Otospongiosis involving entire otic capsule (Class 3). Right axial HRCT scan (key level 1: oval window). The precise preoperative determination of size and location of an otosclerotic focus in combination with the anatomic details of the oval window niche (e.g., narrow niche due to a large focus and/or an overhanging dehiscent facial nerve) has a large influence on the surgical planning (Fig. 187a, b). Fig. 187 The patient is a 46-year-old female with stapedial otosclerosis Class 1 and right 40-dB conductive hearing loss. a Right axial HRCT. Key level 1: oval window. The malleus (1) is fixed to the anterior tympanic spine (2). Note the cochleariform process with the tendon of the tensor tympani muscle (3), the dehiscent and low tympanic segment of the facial nerve (4), the stapes footplate with anterior otosclerotic focus (5), and the fair pneumatization of the mastoid (6). Conclusion: The patient underwent an endaural meatoplasty, superoanterior canalplasty, and a malleostapedotomy (angulated titanium stapes prosthesis) (Fig. 119L2C). The air–bone gap was closed within 10 dB. Furthermore, we have been surprised to find unexpectedly extensive cochlear otosclerosis in conjunction with minimally reduced inner ear function. In such a situation the patient is advised to follow a preoperative fluoride therapy (50 mg sodium fluoride daily) for 3–6 months to limit the growth of active otosclerotic foci and to reduce bleeding when creating the stapedotomy hole in the diseased footplate (Fig. 188a–d). Fig. 188 The patient is a 40-year-old female with combined conductive (40 dB) and sensorineural (30 dB) hearing loss (right ear). a Right axial HRCT. Key level 1: oval window. Note the stapedial focus Class 2 (1) and cochlear focus Class 3 (2). There is a dehiscent tympanic segment of the facial nerve narrowing the oval window niche. The malleus head is in contact with the anterior tympanic spine (3). b Right axial HRCT. Key level 2: round window. The round window is nearly occluded by cochlear otosclerosis (1). The entire otic capsule is invaded by otospongiosis (2). The malleus head is in contact with the anterior tympanic spine (3). Note that the anterior tympanic spine is directly opposite the tendon of the tensor tympani muscle (4). d Right coronal HRCT. Key level: basal turn of cochlea. Massive invasion of the otic capsule by Class 3 cochlear otospongiosis (1). The round window is occluded by otospongiotic bone (2). Note the malleus head (3) and ICA (4). Conclusion: The patient was informed of the unexpected extent of her cochlear otospongiosis, was treated preoperatively for 6 months with sodium fluoride, and was operated on thereafter with an endaural anterosuperior canalplasty and incus-stapedotomy (drilling of thick footplate, titanium stapes prosthesis) (p. 224). The round window was not drilled out. Six months following surgery the conductive hearing loss was reduced within 10 dB. The sensorineural hearing has remained unchanged. Visualization of the complete stapes piston on HRCT scans provides multiple benefits. Changes in position and/or shape of the prosthesis may be responsible for a recurrent hearing loss after stapes surgery. The Teflon-wire and Teflon-platinum pistons (which we used from 1978 to 1996) were difficult to depict radiologically because only their metallic portion was visible (Fig. 189a–d). The introduction of the titanium stapes piston (TSP) in September 1996 changed this situation since the TSP can be visualized in its totality using thin section HRCT images and a workstation. Fig. 189
Incus-Stapedotomy and Malleo-Stapedotomy
 Diagnosis of Otosclerosis
Diagnosis of Otosclerosis
Fenestral otosclerosis (classification)
Cochlear otosclerosis (classification)
Malleo–stapedotomy
Incus-stapedotomy
 Titanium Stapes Prosthesis
Titanium Stapes Prosthesis
a) Incudo- and Malleo-Stapedotomy

Perilymph fistula after stapes surgery
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree