Historical Overview
Rupal H. Trivedi
M. Edward Wilson
This chapter highlights the historical aspects of cataract management in children. We also take an opportunity to give credit to the innovators whose efforts have helped us reach the current level of success in the management of pediatric cataracts. In the past, poor outcomes from pediatric cataract surgery prompted many surgeons to use a conservative approach (described in Chapter 8). Since then, many surgical strategies have come and gone. They have, however, led us to where we are today. Our current “modern” techniques will also, someday, be included in the historical approach category. We need to study the past so the lessons learned do not have to be learned again. Also, one must not forget the giants of thought and skill on whose shoulders we now stand. They led the way to our current understanding and our current technology.
IS SURGERY RECOMMENDED FOR VISUALLY SIGNIFICANT BILATERAL CONGENITAL CATARACTS? IF YES, AT WHAT AGE?
Thick secondary membranes, glaucoma, and corneal decompensation occurred so frequently after pediatric cataract surgery that surgical aggressiveness seemed pointless to many surgeons.
In 1805, James Ware made the statement, “Operation is not so certain a cure for children as in persons of more advanced age.”1 He further noted, “Children born with cataracts, are in general so unmanageable that the operation becomes almost impracticable. For these reasons it is advisable to postpone it until they arrive at the age of reason and reflection, and feel by experience the necessity of submitting to it” (as cited in Ref.2). There has been a good deal of variance regarding the age at which congenital cataracts should be operated upon.
By 1830, Mackenzie questioned (as cited in Ref.2), “In cases of congenital cataract, ought the operation to be delayed till the patient has attained an age sufficient to enable him to give his assent, or ought to be practiced during infancy?” He then answered: “The answer decidedly is to operate in infancy—about the age of from 18 months to 2 years.”
Gurhrie in 1830 stated (as cited in Ref.2): “some surgeons recommending 6 months, others 20 months to 3 years. If the child is healthy at 3, 4 and certainly 6 months, the operation ought to be performed.”
In 1882, Critchett3 noted that “a considerable diversity of opinion still exists as to the period of life when operative measures become not only justifiable, but expedient, and also as to the form of operation which should be adopted in any given case.”
In 1908, Treacher Collins recommended: “to wait until a child is 10 months old before operating. Before that the amount of aqueous humour is so small that it does not suffice for solution of the liberated lens substance”(cited in Ref.4).
In 1936, Kirby (as cited in Ref.2) stated: “if the operation is decided upon, it may well be performed early, as good results are obtained with careful needling.”
In 1948, Cordes recommended that for bilateral dense infantile cataract, the first eye could be operated at 6 months of age, while second eye surgery could wait until 2 to 3 years of age.2
It was reported in the older literature that eyes operated for congenital cataract tended to develop retinal detachments (RDs), irrespective of what age the cataract surgery is undertaken. Unilateral surgery for bilateral congenital cataracts has been advocated in the past because of the reported high incidence of subsequent RD, bilaterality of complication, and poor outlook for successful RD repair.5 When the inevitable RD occurred approximately 25 years later, the cataract in the remaining eye could then be removed with the hope of restoring useful vision and function for another 25 years, until this eye in turn sustained a RD.
Current recommendation of timing of cataract surgery is described in Chapter 6.
SHOULD SURGERY BE DONE FOR UNILATERAL CONGENITAL CATARACT? IS THERE EVER A GOOD VISUAL OUTCOME?
Historically, the management of dense unilateral cataract was very controversial since dense amblyopia was always present and was often severe and unrelenting. Dense unilateral congenital cataract was once regarded as having a dismal visual prognosis. Even today, children with unilateral congenital cataracts remain challenging, and their visual outcomes are still often disappointing.
In 1957, Costenbader and Albert6 stated that they had not seen a single child with a monocular congenital cataract who had benefited from surgical removal of the lens opacity. They noted that it was best not to operate on eyes with a congenital monocular cataract because of morbidity and a poor visual result. They6 further noted that “…since visual acuity is not improved, strabismus is not favorable influenced, and photophobia is not alleviated, we would unequivocally advise against surgery in unilateral congenital cataract unless the cataract is becoming hypermature. The appearance of the eye is usually not improved; function has not been helped, and the eye has been jeopardized if surgery is performed….” (p. 428)
Frey and coworkers,7 in 1973, report that “…some children with monocular cataract can achieve useful central vision” and were the first to advocate that “the dictum of extreme conservatism in the management of monocular cataracts in children needs to be re-evaluated” (p. 388).
Even as late as 1979, Francois8 wrote that “everyone knows the uselessness of operating on unilateral congenital cataracts, as the functional result is always very bad.”
Subsequently, in a landmark paper, Bellar, Hoyt, and coworkers9 in 1981, demonstrated that excellent visual results could be obtained in selected children with monocular congenital cataracts. They reported early treatment and compliant contact lens wear and patching. They emphasized the importance of detection and treatment during the sensitive period of vision development. They further noted,9 “… we believe that surgery during the neonatal period is not only justified but probably essential in any successful treatment of monocular congenital cataract…” (p. 564).
A review of the literature published from 1980 to 1993 revealed that 37% of infants with early surgery achieved a visual acuity outcome of 20/80 or better after surgery for dense unilateral congenital cataract.10 Birch and Stager11 have reported that there exists a 6-week window of time, beginning at birth, during which treatment of a dense congenital unilateral cataract is maximally effective. If treatment is initiated during this period and the child is compliant with contact lens wear and occlusion therapy, an excellent visual acuity outcome can be obtained. Early treatment with good compliance is also associated with a lower prevalence of strabismus and a higher prevalence of fusion and stereopsis.
Taylor,12 in his Doyne Memorial Lecture published in 1998, points out that unilateral congenital cataract is not a socially significant disease since it must be a coincidence of considerable rarity when a person who has such a cataract treated successfully (creating a spare eye) blinds the phakic eye. He points out that if days off work, long-distance travel, repeated clinic visits, fees, and all other disturbances are taken into account, the costs and the disturbance to the daily lives of patients and their parents are very substantial.12 He points out that even at major referral centers, a good functional result (e.g., driving vision) is unlikely to be achieved in more than 50% of patients presenting with unilateral congenital cataract. Taylor12 acknowledged, however, that an increasing number of cases with some degree of binocular vision were being reported; this has functional benefits of its own and, also, reduces the normally very high incidence of strabismus.
In 2001, Wright stated, “Not all children treated aggressively will obtain that lofty goal of good visual acuity and binocular vision, but it is guaranteed that without aggressive treatment virtually all children with a visually significant cataract at birth will end up with a blind eye and strabismus…” (p. 1122).13 We concur with Wright’s view in our practice and continue treating these eyes surgically as soon after 30 days of life as possible.13 In recent years, dense monocular infantile cataract has changed from a “hopeless” disease to a treatable, although demanding and sometimes frustrating, condition. If treatment is initiated in the ideal 4- to 6-week age (allowing the newborn to “feed and grow” for 30 days but still removing the unilateral cataract during the 6 weeks window), and the child is compliant with optical correction and occlusion therapy, an excellent visual acuity outcome can be obtained.11 In the past few years, advances in surgical
techniques and aphakic correction have occurred but amblyopia is still the major determinant of the ultimate visual outcome of pediatric cataract surgery. Gradually, the evolution of cataract surgical techniques combined with early detection and surgery and the ability to provide early, effective, and constant optical rehabilitation led to better outcomes.
techniques and aphakic correction have occurred but amblyopia is still the major determinant of the ultimate visual outcome of pediatric cataract surgery. Gradually, the evolution of cataract surgical techniques combined with early detection and surgery and the ability to provide early, effective, and constant optical rehabilitation led to better outcomes.
OPERATIVE TECHNIQUES
In 1951 Cordes described that the ideal operation for congenital cataract should meet the following conditions.14
It would be a single procedure providing for the removal of the major portion of the lens, so that the rest could absorb.
There would be no interference with the pupil, and the danger of incarceration or adherence of the iris to the wound would be minimal.
There would be no interference with the posterior capsule and the vitreous.
The danger of glaucoma would be minimized.
Unfortunately, this ideal operation did not exist then and still does not exist today. Pediatric cataract surgery involves higher rate of intraoperative and postoperative complications, and we have learned that dealing safely with the necessity of “interference” with the posterior capsule and the vitreous is a must for the young child. Innovations in surgical techniques and technology have allowed us to achieve improved anatomical and visual outcomes from our pediatric cataract surgeries.
Optical Iridectomy
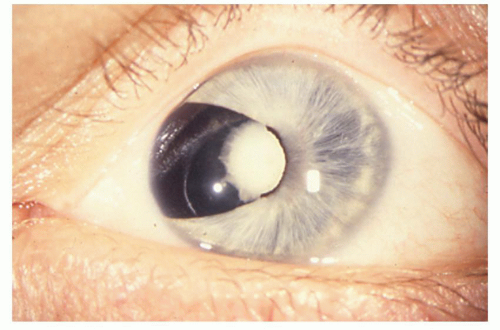
For visually significant congenital cataracts, some surgeons resorted to an optical iridectomy to avoid the inflammatory response and membranes that developed when the lens was entered (Fig. 11.1). Optical iridectomy was useless when total cataracts were present. However, it was recommended in cases of fetal nuclear opacity, zonular or polar cataracts in which dilation of the pupil improved vision.14 Optical iridectomy was often performed for the purpose of helping near vision, in the inferior nasal sector between 4 and 5 o’clock in the right and 7 and 8 o’clock in the left eye. Some surgeons preferred the 12 o’clock position for cases where the development of the cataract would later make a more radical intervention necessary. However, the upper eye lid covered the upper part of the cornea and reduced, to some extent, the benefit of the intervention.15 This optical iridectomy technique preserved accommodation and avoided secondary membranes.6 In multi-handicapped children with bilateral central fetal nuclear cataracts, this technique was advocated also to avoid contact lens and spectacle problems. However, the visual results were not satisfactory. Despite bilateral surgery, nystagmus nearly always developed and vision was rarely better than 20/200 even when a clear zone existed peripheral to the fetal nuclear opacity.16
Discission/Needling
Although couching for cataract was practiced in the Hellenistic period, its use in children was not ideal: an already tricky operation was turned into an exceptionally difficult one by the child’s anatomy and the lack of an anesthetic (cited in Ref.12). Needling/discission is probably the oldest of all surgeries for removal of congenital cataracts. Aurelius Cornelius, a Roman physician who lived 2,000 years ago (quoted in Ref.17




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree