Purpose
To evaluate the health-related quality of life and emotional status of anophthalmic patients.
Design
Prospective, cross-sectional study.
Methods
The study included 134 monocular anophthalmic patients and 48 healthy volunteers who visited the department of Ophthalmology at the Yonsei University College of Medicine, Seoul, Korea, between July and December 2008. Surveys were administered to participants to evaluate their sociodemographic characteristics and disease-related factors. Data collected from the Short-Form 36-Item Health Survey (SF-36) and the Hospital Anxiety and Depression Scale survey instruments were analyzed to identify significant differences and correlations between categories.
Results
Anophthalmic patients scored lower in all categories of SF-36 compared with controls. Married females and participants with children generally had lower scores on the SF-36, and some of the differences were statistically significant. There were significant negative correlations between all SF-36 scores and participant self-evaluations on whether they had negative feelings regarding their social interpersonal relationships as a result of wearing prostheses. Those who scored higher on the Hospital Anxiety and Depression Scale anxiety and depression scales tended to evade social interrelations significantly.
Conclusions
Anophthalmic patients had lower health-related quality-of-life scores than healthy individuals. This finding was particularly evident in terms of the patients’ own perceptions of their social relationships, which were negatively affected by their use of prosthetic eyes. Such perceptions reduced their quality of life and heightened their anxiety and depression. Therefore, it is important to evaluate both the physical and emotional well-being of anophthalmic patients to identify those patients who will need additional physical and mental support.
The loss of an eye, regardless of whether it results from serious disease or injury, can disturb a patient’s life and ultimately can result in mental trauma. In certain cases, patients may need to undergo surgery to remove an eye. This procedure has devastating emotional effects on the patient, such as morbid fears of meeting new people and entering new social environments because of their appearance, defined as anthrophobia. In addition, patients can experience inferiority complexes and fears of being socially outcast.
Proper surgical and maintenance procedures are required to promote the natural appearance of ocular prostheses and to minimize any mental distress. A satisfaction survey of anophthalmic patients who have ocular prostheses was performed, and the overall rate of satisfaction with the prosthesis was relatively high (71.8%). However, even with structured and focused cosmetic treatments, patients can become mentally traumatized both during and after the treatment process. Patients can lose self-confidence and can develop problems initiating and maintaining social relationships. Furthermore, ophthalmologists still are unsure about the extent of the physical and emotional problems that affect these patients. At present, rehabilitation efforts directed toward the patient’s psychological and emotional instabilities that stem from the removal of an eye have been insufficient. Therefore, this study was designed to evaluate the quality of life and emotional status of anophthalmic patients by assessing their levels of depression and anxiety using established survey instruments. These objective evaluations may aid in the identification of anophthalmic patients who are more likely to need additional physical and mental support.
Methods
Study Design and Recruitment
This cross-sectional study included 134 anophthalmic patients and 48 healthy volunteers who visited the Department of Ophthalmology at the Yonsei University College of Medicine, Seoul, Korea, between July and December 2008. The control group comprised healthy volunteers who were age matched and gender matched to the study group. Patients who could not fill out the survey themselves were provided with support from those conducting the research.
The survey included the following categories: gender, age, marital status, number of children, disease history, prior surgeries, and cause and duration of anophthalmos. The medical outcome study Short-Form 36-Item Health Survey (SF-36) was used to assess the quality of life, and the Hospital Anxiety and Depression Scale (HADS) was used to evaluate the degree of anxiety and depression.
Survey Instrument
The Korean version of the SF-36 was used to evaluate the health-related quality of life of the study participants. It has been shown previously to be a credible and reasonable instrument to measure the quality of life in study groups. The survey contained 8 itemized categories and 36 questions. The 8 categories were as follows: (1) physical functioning (e.g., walking, lifting), (2) role function-physical (e.g., limitations in ability to perform usual activities), (3) body pain (BP; e.g., level of body pain or discomfort), (4) general health perceptions (GH; e.g., global evaluation of health), (5) vitality (VT; e.g., energy level or fatigue), (6) social functioning (e.g., impact of health or emotional problems on social activities), (7) role function-emotional (e.g., impact of emotional problems on work or daily activities), and (8) mental health (e.g., anxiety, depression, sense of psychological well-being). The raw data from the 8 categories were converted into scores, were categorically combined, and then were rescaled on a scale of 100. Higher combined scores represented a better quality of life. The first 4 categories were grouped as the physical component summary (PCS), and the last 4 categories were grouped as the mental component summary (MCS). Finally, these 8 categories were converted into scores and evaluated with respect to the sociodemographic and clinical characteristics of the participants. These scores then were assessed for their correlation with levels of anxiety and depression, which were measured using the next survey instrument.
The HADS was used to measure the anxiety and depression levels of patients. Developed by Zigmond and Snaith in 1983, this method is a self-rating screening instrument for anxiety and depression levels of patients that can be carried out during the short waiting times when patients are visiting nonpsychiatric hospital clinics. The HADS consists of 7 anxiety-related categories (HADS-A) and 7 depression-related categories (HADS-D). The total scale is defined as the sum of HADS-A and HADS-D, so it contains 14 categories. Each category is scored from 0 (never) to 3 (almost), and higher scores are associated with higher levels of anxiety and depression (ranges were as follows: 0 to 7, normal; 8 to 10, probable disorder; and 11 to 21, possible disorder). The reliability and validity of the Korean version of HADS was established previously. A score of 8 commonly is used as the cutoff for anxiety and depression in HADS-based studies. In a previous Korean population-based study, a cutoff of 8 was reported to reflect best the sensitivity and specificity of both HADS-A and HADS-D. Therefore, a score of 8 was used as the cutoff point in this study for dividing participants into groups of high and low levels of anxiety and depression. The sociodemographic factors, clinical characteristics, and SF-36 scores were compared independently with groups with scores less than and more than 8 for HADS-A and HADS-D.
Statistical Analysis
A two-sample t test was used to compare scores for all SF-36 categories according to gender, marital status, and number of children. This statistical test also was used to compare the scores for all SF-36 categories between the study and control groups.
An analysis of variance was performed to compare the differences between all SF-36 categories scored according to the cause of blindness and duration of anophthalmos, the participant’s self-evaluation regarding whether they had negative feelings about their social interpersonal relationships because of wearing a prosthesis, and the participant’s self-evaluation of how the prosthesis cosmetically compared with their normal eye.
The correlations between the SF-36 scores with both age and the total HADS scale were analyzed using the Pearson correlation test. The Spearman rank correlation test was used to analyze the correlation between the SF-36 scores and the cause of blindness and duration of anophthalmos, the participant’s self-evaluation regarding whether they had negative feelings about their social interpersonal relationships because of wearing a prosthesis, and the participant’s self-evaluation regarding how the prosthesis cosmetically compared with their normal eye.
The Pearson chi-square test or Fisher exact test was used to compare gender, marital status, presence of children, and the cause of blindness according to HADS-A and HADS-D scores.
The Cochran-Armitage trend test was used to analyze the trend of the duration of anophthalmos, the participant’s self-evaluation regarding whether they had negative feelings about their social interpersonal relationships because of wearing a prosthesis, and the participant’s self-evaluation of how the prosthesis cosmetically compared with their normal eye according to HADS-A and HADS-D scores.
All statistical analyses were performed using the SAS statistical software package version 9.1 (SAS Institute, Cary, North Carolina, USA). A P value less than .05 was considered to be statistically significant.
Results
Table 1 provides the sociodemographic characteristics of the 134 patients and 48 healthy volunteers in this study. In the patient group, the mean age ± standard deviation was 43 ± 15.7 years, and there were slightly more female participants (n = 71; 53%). Of the 134 participants, 62% were married and 60% had children. The right eye was affected in 63 (47%) patients. There were 9 (6.7%) patients diagnosed with depression, and only 6 of these patients were taking medicine for their depression. The most common cause of blindness was physical trauma (52%). The normal control group involved 48 individuals between 23 and 76 years of age (mean age, 41.2 years; 26 women). There were no significant differences in the demographic data between the patient and control groups.
| Characteristics | Patients (n = 134) | Controls (n = 48) | P Value |
|---|---|---|---|
| Mean age ± SD (yrs) | 43.4 ± 15.7 | 41.2 ± 18.8 | .461 a |
| Sex | |||
| Male | 63 (47%) | 22 (46%) | .888 b |
| Female | 71 (53%) | 26 (54%) | |
| Marital status | |||
| Married | 83 (62%) | 29 (60%) | .852 b |
| Single, divorced, or widowed | 51 (38%) | 19 (40%) | |
| Children yes | 80 (60%) | 26 (54%) | .505 b |
| Diagnosis of depression | 9 (6.7%) | 0 (0%) | .115 c |
| Cause of blindness | |||
| Eye disease | 40 (30%) | ||
| Trauma | 70 (52%) | — | — |
| Eye malignancy | 24 (18%) | ||
| Duration of anophthalmos (yrs) | |||
| Acute (within 1 yr) | 9 (6.7%) | ||
| Recent (1 to 5 yrs) | 13 (9.7%) | ||
| 5 to 10 | 13 (9.7%) | — | — |
| 10 to 20 | 39 (29%) | ||
| 20 to 30 | 24 (18%) | ||
| More than 30 | 36 (27%) |
As shown in Figure 1 , all categories of the SF-36 survey were scored significantly lower than those of the normal control group ( P < .05, t test). The mean ± standard deviation values for PCS and MCS of anophthalmic patients were 46.2 ± 8.4 and 47.8 ± 9.4, respectively.
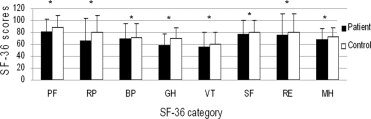
Table 2 provides the HADS data and responses to the self-questionnaire. The mean ± standard deviation values for HADS-A and HADS-D were 5.9 ± 3.8 and 5.1 ± 3.5, respectively. The percentage of participants with a score of 8 or higher with respect to HADS-A and HADS-D were 29.9% and 28.4%, respectively. Only 7.5% of patients reported that the prosthetic eye was not different cosmetically from the normal opposite eye; however, 43.3% believed both eyes appeared moderately and definitely different. With respect to the negative impact of the prosthetic eye on their social interpersonal relationships, only 6.7% reported never, and 42% answered frequently or always.
| HADS-A (anxiety) | |
| Mean ± SD | 5.9 ± 3.8 |
| 0 to 7 (n) | 94 (70.1%) |
| 8 to 21 (n) | 40 (29.9%) |
| HADS-D (depression) | |
| mean ± SD | 5.1 ± 3.5 |
| 0 to 7 (n) | 96 (71.6%) |
| 8 to 21 (n) | 38 (28.4%) |
| Self-questionnaire 1: Is prosthetic eye cosmetically different from the normal opposite eye? | |
| Not different (score 1) | 10 (7.5%) |
| Minimally different (score 2) | 66 (49.3%) |
| Moderately different (score 3) | 38 (28.4%) |
| Definitely different (score 4) | 20 (14.9%) |
| Self-questionnaire 2: How often does your prosthetic eye negatively impact your social interpersonal relationships? | |
| Never (score 1) | 9 (6.7%) |
| Infrequently (score 2) | 67 (50%) |
| Frequently (score 3) | 26 (19%) |
| Always (score 4) | 32 (23%) |
The SF-36 PCS and MCS scores of patients negatively correlated with age ( P < .05, r = −0.6306; P < .05, r = −0.2098, Pearson correlation). Female participants had lower scores in all SF-36 categories compared with male participants, particularly with regard to the 6 categories (BP, GH, VT, social functioning, mental health, and PCS), which were significantly lower ( P < .05, t test). The married participants had lower scores in all SF-36 categories compared with single participants, particularly with regard to the physical functioning, role function-physical, BP, GH, VT, social functioning, and PCS categories, which were significantly lower ( P < .05, t test). The participants with children had lower scores in all SF-36 categories compared with those without children, particularly with regard to the physical functioning, BP, GH, VT, and PCS categories, which were significantly lower ( P < .05, t test).
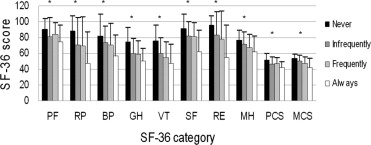
There were significant differences in the scores of all SF-36 categories regarding whether the participants had negative feelings about their social interpersonal relationships as a result of wearing a prosthesis ( P < .05 for all categories, analysis of variance; Figure 2 ). There were also significantly negative correlations between all SF-36 scores and the participant’s self-evaluation regarding whether they had negative feelings about their social interpersonal relationships as a result of wearing a prosthesis ( P < .05, Spearman rank correlation; Table 3 ).
| SF-36 Category | r | P Value |
|---|---|---|
| Physical functioning | −0.230 | .0075 |
| Role function-physical | −0.259 | .0025 |
| Body pain | −0.270 | .0016 |
| General health perception | −0.286 | .0008 |
| Vitality | −0.303 | .0004 |
| Social functioning | −0.345 | < .0001 |
| Role function-emotional | −0.334 | < .0001 |
| Mental health | −0.237 | .0059 |
| Physical component summary | −0.333 | .0023 |
| Mental component summary | −0.261 | < .0001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


