Although unilateral hearing loss is often the initial sign of vestibular schwannoma (VS), the pathogenesis of the associated structures within the cerebellopontine angle can result in vestibular, facial, or vascular symptoms. Removal of a VS causes deficits in hearing, balance, and gaze stability. The resulting hearing loss eliminates the benefits of binaural listening that provide localization, loudness summation, and listening-in-noise ability. Reduced balance and gaze stability increase fall risk. This review discusses modern treatment options for auditory and vestibular rehabilitation including contralateral routing of signals (CROS), bilateral CROS, bone-anchored implants, tinnitus management, gaze and gait stability exercises.
| APHAB | Abbreviated Profile of Hearing Aid Benefit |
| BiCROS | Bilateral CROS |
| BAI | Bone-anchored implant |
| CPA | Cerebellopontine angle |
| CROS | Contralateral routing of signals |
| DVA | Dynamic visual acuity |
| GHABP | Glasgow Hearing Aid Benefit Profile |
| HSN | Head shaking–induced nystagmus |
| IAC | Internal auditory canal |
| rTMS | Repetitive transcranial magnetic stimulation |
| SCC | Semicircular canal |
| SNR | Signal-to-noise ratio |
| SSD | Single-sided deafness |
| SSQ | Speech, Spatial and Qualities of hearing scale |
| THI | Tinnitus Handicap Inventory |
| TRQ | Tinnitus Reaction Questionnaire |
| UHL | Unilateral hearing loss |
| VPT | Vestibular rehabilitation |
| VS | Vestibular schwannoma |
Vestibular schwannomas (VS) are benign tumors arising from the Schwann cell of the vestibular nerve, often in the internal auditory canal (IAC). The incidence of VS has been estimated to be between 7 and 15 people per million, and constitute about 80% of all tumors found in the cerebellopontine angle. Along with the vestibulocochlear nerve (CN8), the IAC houses the facial nerve (CN7) and the internal auditory artery. Symptom presentation is usually related to where the tumor arises. If the tumor arises in the IAC, tinnitus and hearing loss are often the first symptoms. However, if the growth occurs in the cerebellopontine angle (CPA), the tumor may become quite large before symptoms of hearing loss are revealed. Thus, although unilateral hearing loss (UHL) is often the initial sign of VS, the pathogenesis of the associated structures within the space can sometimes result in vestibular (ie, vertigo, imbalance), facial, or even vascular symptoms (ie, headaches, fatigue) as the driving force for an individual to seek medical attention.
Total hearing loss in the affected ear may be a significant handicap. Abnormal vestibular function occurs in many patients but usually abates with central compensation. Hearing loss becomes a long-term disability, often requiring sustained intervention and management throughout the life of the patient. For those who do not have spontaneous vestibular compensation or are slow to compensate, vestibular rehabilitation, chemical labyrinthotomy with gentamycin, or tumor removal may be necessary.
Auditory habilitation
Hearing Loss
UHL is the most common symptom of patients with VS, followed by tinnitus and imbalance. Often, whether from natural history, radiation, or surgery, the result is profound hearing loss. The deficits associated with UHL have been well documented. These individuals experience reduced sound awareness, difficulty communicating in noise, and reduced ability to localize. The communication deficits experienced by individuals with severe to profound UHL may produce psychological, social, and vocational issues.
The auditory pathway consists of afferent fibers transmitting acoustic information regarding frequency, intensity, and timing of a sound source to the auditory cortex. The auditory fibers are tonotopically organized, allowing for preservation of frequency-specific cues that provide discrete information to higher-order auditory structures regarding pitch and loudness. Binaural hearing integrates the timing and intensity differences of acoustic signals arriving at each ear to interpret the spatial aspects of sound. This process enables the auditory system to efficiently separate and localize sounds, increase loudness, and improve sound quality. Hearing impairment from VS may occur at the cochlea, cochlear nerve, brainstem, or a combination of sites. Binaural cues such as interaural timing and level differences, binaural summation, and head-related transfer function play a critical role in localization and listening-in-noise ability. Although ipsilateral coding is maintained in the better hearing ear, for adults in complex listening environments, the loss of binaural cues can result in a considerable handicap.
Clinical evaluation
The goals of auditory rehabilitation in the VS population are to:
- 1.
Restore access to sound
- 2.
Reduce the associated deficits caused by the hearing loss.
To provide the best form of rehabilitation, accurate assessment of these deficits must be made. A comprehensive evaluation is conducted of the integrity of the peripheral and central auditory systems to determine the degree of associated handicap.
Standard audiometric test battery
The objectives are to:
- 1.
Establish frequency specific residual hearing sensitivity for both ears
- 2.
Confirm or deny the presence of a contributing conductive component
- 3.
Assess word-recognition ability in quiet.
The resulting data provide the clinician with tangible hearing outcomes as a starting point for the counseling process. The patient on a watch-and-wait plan may have a notably different auditory profile from one who has undergone complete resection. It can be expected that the rehabilitation of these patients may differ substantially. Clinicians cannot anticipate an individual’s success in real-world listening without establishing a more complete auditory profile that assesses individualized performance beyond that of the pure tone audiogram. Auditory processing capabilities can vary significantly by individual.
Speech in noise
Compromised speech-in-noise ability is a primary deficit experienced by individuals with severe to profound UHL. A good test battery should include speech-in-noise measures to evaluate each patient’s signal-to-noise ratio (SNR) loss. Which is the increase in SNR ratio required to obtain 50% correct words, sentences, or words in sentences, compared with normal performance. This component is important because not all patients will demonstrate the same degree of impairment in noise. Taylor demonstrated that individuals who presented with similar hearing loss configurations on pure tone audiometric testing could vary by more than 20 dB in performance on speech-in-noise measures. This finding is powerful evidence that an individual’s performance in noise cannot be predicted on the pure tone audiogram alone. Real-world listening is far more complex and dynamic than what is represented in the standard audiogram. By including speech-in-noise measures in the evaluation process, the clinician is provided with individualized deficit-specific information regarding communication ability in complex listening environments. This information is not only valuable in determining appropriate intervention, but also functions as a counseling tool to assist the clinician in setting realistic expectations for the patient’s communication needs.
Sound localization
The ability to localize sounds becomes impaired in UHL patients because of the loss of interaural level and timing cues. Objective assessment of localization is not regularly incorporated into the clinical test battery. Current treatment options such as contralateral routing of signal (CROS) hearing aids (see later discussion) and bone-conduction implants continue to be limited in their ability to remediate the loss of localization. Clinicians should take care to counsel patients in detail regarding expectations for localization after treatment.
Subjective measures
Along with the auditory impairment, patients and their clinicians must consider the psychological, social, and vocational impact that may be contributing to the handicap. Subjective assessment of how the hearing loss is affecting the patient’s quality of life is an important parameter in the determination of postoperative treatment options. A subjective questionnaire should be specific and should be selected based on the communication needs of the patient. Several measures exist in the literature and include the following:
The Abbreviated Profile of Hearing Aid Benefit (APHAB) is a widely used 24-item subjective outcome measure evaluating disability associated with hearing loss. Specifically it assesses ease of communication, reverberation, listening in background noise, and aversiveness to sound. The APHAB is a popular tool, due to its usefulness for determining disability and the change in disability after treatment.
The Glasgow Profile of Hearing Aid Benefit (GPHAB) is an outcome measure that assesses auditory disability, handicap, hearing aid benefit, and hearing aid satisfaction using 4 specific listening and communication situations. In addition, the GPHAB allows patients to identify up to 4 additional situations for customized assessment.
The Speech, Spatial and Qualities of hearing scale (SSQ) is a validated measure to assess impairment associated with binaural function. The 3 domains provide comprehensive information about listening to speech in complex environments, including localization, direction, and movement of sound, segregation of sounds, and ability to attend to multiple auditory inputs. The SSQ is unique in that it allows for some assessment of localization. The deficit-specific questions of the SSQ make it an ideal tool for use in the VS population.
Physical and cognitive contributors should also be considered prior to intervention.
Intervention
Appropriate intervention addresses the goals of the patient through compensation for the physiologic and subjective handicaps as indicated by outcome measures. Preoperative hearing loss can range from mild to profound. Most preoperative hearing losses can be successfully treated with traditional amplification as long as the hearing loss is not too severe and word-recognition ability remains intact. Despite good residual hearing across the low- to mid-frequency range, some preoperative VS patients present with unaidable high-frequency hearing loss. These patients can be considered for alternative amplification options such as frequency-compression and frequency-transposition hearing aids. These devices attempt to shift sound from the unaidable high-frequency region to a lower frequency to be interpreted by the ear. This option varies in success, and is sometimes rejected because of dissatisfaction with sound quality.
For those patients whose hearing loss progresses to the severe to profound UHL range, also referred to as single-sided deafness (SSD), a variety of options exist ( Table 1 ). The treatment goal for these patients is to provide access to sound arriving at the affected ear, thereby compensating for the head-shadow effect. Patients with severe to profound UHL are not candidates for traditional amplification. These patients must consider options that use their better hearing ear to provide access to sound arriving from the SSD ear. The anticipated effect of this is restoration of sound awareness and improvement in listening-in-noise ability.
| Treatment | Benefits | Limitations |
|---|---|---|
| CROS hearing aid |
|
|
| BiCROS hearing aid |
|
|
| Transcranial CROS |
|
|
| Bone-conduction hearing aid |
|
|
| TransEAR |
|
|
| Bone-anchored implants |
|
|
a Although some clinicians allow trials with a demonstration device at home, that is not the recommendation of the authors, whose opinion is that this often leads to misconception about device performance, due to lack of control regarding device placement, output levels, distortion, and feedback.
Options for these patients traditionally have been limited to CROS and bilateral CROS (BiCROS) amplifiers. The CROS system attempts to restore access to sound arriving from the affected side by collecting sound with a microphone placed on the SSD ear and transferring it via wired or wireless transmission to a receiver in the normal ear. However, obstacles such as the need to wear bilateral hearing aids, occlusion in the normal ear, and poor or unnatural sound quality have led to poor acceptance of these devices. Historically, patients who rejected CROS amplifiers were left to rely entirely on their better hearing ear.
Other treatment options have focused on bone conduction as a means to transmit sound to the functioning cochlea. Some early attempts at this included the transcranial CROS and the bone-conduction hearing aid. The transcranial CROS attempted to stimulate the contralateral cochlea by sending an air-conduction signal via a high-power hearing aid in the nonfunctioning side. This device was not well accepted, due to reports of discomfort and poor sound quality. Although bone-conduction hearing aids tend to provide better sound quality and ease of listening, they have seen little use in the adult population because of physical discomfort and lack of aesthetic appeal.
In recent years treatment options have expanded to include alternative forms of bone-conduction stimulation to remediate profound UHL. Based on the same principles, improvements in technology have led to options that provide good sound quality, comfort, and aesthetic appeal. The TransEAR (Ear Technology Corporation, Johnson City, TN, USA) amplifier uses a bone conductor that is custom fitted to the medial bony portion of the ear canal, thereby sending the acoustic information through the skull via vibration to the functioning cochlea in the opposite ear. Sophono Inc (Boulder, CO, USA) has introduced a transcutaneous bone-conduction implant recently approved by the Food and Drug Administration. A dental bone conductor appliance has been developed by Sonitus Inc (San Mateo, CA, USA). As of this writing, percutaneous bone-anchored implants (BAIs) are approved and marketed in the United States by Cochlear Corp. (Denver, CO, USA) and Oticon Medical (Somerset, NJ, USA).
Recently BAIs have gained increased popularity as a treatment option for patients with profound UHL. As with the previously discussed options, BAIs ( Fig. 1 ) collect sound arriving at the nonfunctioning ear and deliver it to the functioning cochlea by way of bone conduction. As an implant system, BAIs consist of an osseointegrated titanium fixture with a percutaneous abutment that is implanted into the mastoid bone behind the ear, which allows for direct bone conduction ( Fig. 2 ) in contrast to transcutaneous stimulation by a bone-conduction hearing aid. A sound processor is attached to the implant externally and transmits sound via vibration of the skull to the functioning cochlea.

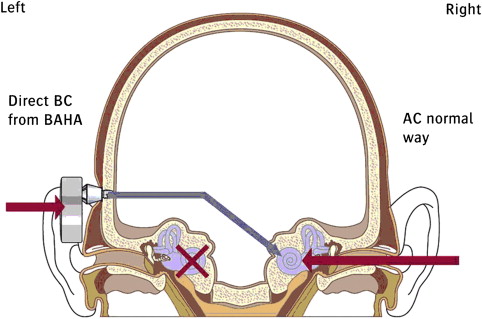
Quickly becoming the standard form of treatment, BAIs have met with some controversy because they require surgical intervention to remediate the hearing loss. The goals of BAIs for SSD are the same as those previously discussed for noninvasive options: to compensate for the head-shadow effect and restore sound awareness on the impaired side. As a result, clinicians are faced with the challenge of deciding whether the benefit received by a BAI warrants recommending a more invasive form of treatment. There is strong evidence that patients who receive a BAI for remediation of UHL experience improvement in both quality of life and listening-in-noise ability. Furthermore, comparison studies have consistently reported improved performance and patient satisfaction with BAIs compared with the noninvasive CROS hearing aid. Although there is considerable support for the use of BAIs over CROS, there has been some criticism regarding the quality of these studies. At present, a critical mass of literature comparing the TransEAR amplifier with BAIs does not exist.
None of the listed treatment options restores true binaural hearing. The treatments are a means to provide access to sound arriving at the impaired ear. Benefits are limited, even in BAIs, and no objective evidence exists to support restoration of localization ability. Degree of benefit varies by individual and must be thoroughly assessed before any treatment implementation. Counseling is an essential component of ensuring successful outcomes.
Selection process
Selecting the appropriate treatment for the patient is a comprehensive process. It should be a collaborative effort that includes the patient, his or her communication partners, the surgeon, and other health care professionals involved in the medical management. A protocol based on known auditory deficits of the individual seeking treatment is essential for determining treatment options, candidacy, and expected outcomes. For those patients wishing to pursue a BAI, it is the clinician’s responsibility to obtain as much information as possible to determine expected outcomes following surgery. The audiogram does not provide sufficient determination of candidacy; rather, it should be used as an indicator to identify those who may be a candidate. Candidacy should be determined by a comprehensive protocol evaluating the broad range of deficits and handicaps experienced by the patient.
- •
The evaluation process begins with comprehensive audiometry, including ear-specific word-recognition ability in quiet. The team reviews the hearing test and the expected auditory limitations associated with any hearing loss. The patient is then provided with information regarding all noninvasive alternative options, and a trial with a CROS hearing device is strongly encouraged.
- •
The next step is to assess speech-in-noise deficit using measures such as the Quick Speech-in-Noise Test (QuickSIN; Etymotic Research, Elk Grove Village, IL, USA), the Bamford-Kowal-Bench Speech-in-Noise test (BKB-SIN; Etymotic Research), or the Hearing in Noise Test (HINT; Maico, Eden Prairie, MN, USA).
- •
Individuals with severe to profound UHL struggle the most with listening in noise (11), particularly when the signal of interest is arriving at the affected side and noise is masking the better hearing ear. To assess binaural deficit related to the head shadow effect, testing should be conducted in the sound field with noise directed towards the better-hearing ear and speech stimuli towards the affected ear ( Fig. 3 ).
- ○
This can be repeated with both the noise and speech presented at 0 degrees azimuth or with speech presented at 0° azimuth and noise directed at the better hearing ear.
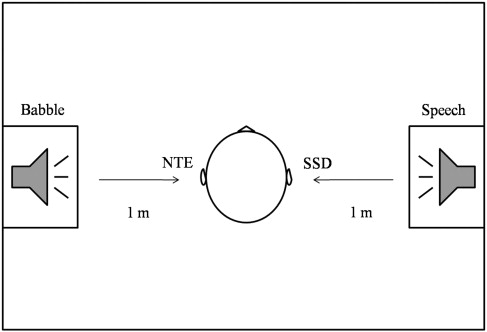
Fig. 3
Speech-in-Noise Test setup. Speech stimuli are directed toward the affected ear and babble noise is directed toward the better hearing ear.
- ○
- •
Baseline SNR loss is established for all conditions.
- •
Performance on speech-in-noise tasks is then reevaluated using the BAI bone-conductor demonstration device. The demonstration device is placed near the affected ear with the microphone directed toward the speaker.
- •
Performance is compared across varying conditions with the unaided baseline results, and potential benefit is predicted by overall improvement in adverse listening conditions. This course of action not only provides the clinician with objective data regarding the expected performance with the implant following surgery, but also helps to establish realistic expectations for the patient. Tests such as the QuickSIN and BKB-SIN use a multitalker babble noise source, resulting in a highly relatable testing experience for patients. Speech-in-noise testing will frequently result in patient responses such as “this is the first time someone has really tested my hearing loss” or “this is exactly like the problem I have when I’m at a restaurant.” Patients are able to experience the device by listening to it in-office and to appreciate the expected benefit using a simulated real-world listening environment, thus empowering both the clinician and the patient to make confident decisions regarding intervention.
- •
The same protocol ( Table 2 ) can be applied using CROS hearing aids, and should be included in the selection process. Performance can be compared with baseline and BAI results.
Table 2
Evaluation and verification treatment protocol for UHL
Assessment of Candidacy
- 1.
Basic comprehensive audiometric test battery
- a.
Pure tone air and bone thresholds, speech recognition, immitance measures
- b.
Ensure stable hearing, adequate residual hearing in better ear
- a.
- 2.
Establish communication handicap/disability
- a.
Use SSQ for assessment of localization/spatial deficits
- a.
- 3.
Speech-in-noise testing in the sound field
- a.
Establish SNR loss in unaided condition
- b.
Reassess using demonstration devices when applicable (BAI, CROS)
- c.
Speaker configuration
- i.
Speech to affected ear, noise to better ear (270°/90° azimuth)
- ii.
Speech to front, noise to better ear (0°/90° azimuth)
- iii.
Speech and noise to front (0°/0° azimuth)
- i.
- d.
Compare unaided to aided performance to predict benefit
- a.
Treatment Selection
- 1.
Review single-sided deafness and potential auditory limitations
- 2.
Review treatment options (see Table 1 )
- a.
Demonstrate devices to patients, report subjective benefit
- a.
- 3.
Discuss benefits and limitations in relation to results of initial assessment
Fitting and Verification
- 1.
Hearing aids
- a.
Electroacoustic analyses
- b.
Probe microphone measures
- a.
- 2.
Bone-anchored implant
- a.
Aided speech-in-noise testing in the sound field using previously described method
- i.
Compare results to unaided and preintervention assessment results
- i.
- b.
Aided loudness assessment using recorded speech at 55, 65, and 75 dBSPL
- a.
- 3.
Device orientation
- 4.
Validation of device benefit
- a.
Hearing outcome measures
- b.
Measures should be relevant the auditory deficits of the VS population
- a.
Management
- 1.
Initial follow-up at 2–4 weeks
- a.
Reassess hearing outcomes, fine tune as needed, verify speech-in-noise benefit
- a.
- 2.
Long-term follow-up should be structured based on patient’s communication needs and perceived handicap/disability
- a.
Recommended minimum is 3 months, 6 months, and annually
- a.
- 1.
- •
Time should be taken to demonstrate each device to the patient and review its function. The patient should be able to demonstrate the ability to manage the device, and this is even more crucial regarding the BAI, whereby the patient will be expected to manage the implant site as well as the external processor over a lifetime.
Once the evaluation process is complete, all of the data are reviewed with the patient to determine candidacy. No specific criteria exist for establishing the ideal candidate. Patients can present in a multitude of ways. The process is individual-specific and treatment decisions must be made with the patient. For example, consider the patient who demonstrates significant improvement on speech-in-noise testing, but displays very low handicap levels. Such a patient is not an optimal surgical candidate. Patients who present with very low handicap levels despite objective benefit often state postoperatively that they do not wear their devices often or that they do not perceive benefit from their device. Another patient may present with significant handicap but little to no benefit from aided speech-in-noise testing. This patient is likely to have unrealistic expectations and will be left frustrated and dissatisfied after surgery.
All of the aforementioned options are intended for patients who have normal to near-normal hearing in the better hearing ear. Indications for BAIs in this population have been limited to those persons who have less than 20 dB PTA in the better ear. However, many VS patients present with some degree of hearing loss in the better hearing ear. For these patients, particularly those with significant impairment, amplification of the better ear is required for adequate remediation of the hearing loss. This scenario has traditionally been addressed with bilateral CROS (BiCROS) amplification, and has recently been shown to have high satisfaction and acceptance rates. Increasingly, BAIs also are being used in this complex patient population. A recent study by Wazen and colleagues found that BAI patients with mild to moderate hearing loss in the better hearing ear showed improved performance on objective tests and that 91% reported improved quality of life. These findings are not without controversy, and it is noteworthy that these applications continue to be considered as outside the standard clinical guidelines. This fact underscores the importance of a comprehensive evaluation to determine candidacy. Conventional amplification may be considered for the better ear.
The evaluation and selection process uses a battery of objective and subjective tests to gather data for the clinician to use as a guideline in counseling the patient on the hearing loss, expectations, and options. Often, treatment is straightforward and patients find immediate success. However, for those patients who are faced with greater challenges such as reduced auditory processing ability, physical complications, cognitive factors, and so forth, motivation and realistic expectations will drive the outcome.
Fitting hearing devices
Regardless of which treatment option is selected, fitting a device is a multistep process. The fitting protocol will vary slightly based on the intervention. During the fitting appointment, the device is programmed to the patient’s residual hearing profile in the better hearing ear and to meet the listening needs of the patient. Adjustments may be made to increase patient comfort.
Key components to a successful fitting include:
- •
Ensuring that soft speech is audible
- •
Ensuring that loud sounds are within the level of patient comfort
- •
Maintaining clarity of speech.
Counseling patients on communication strategies and establishing realistic expectations with the patient and communication partners is a fundamental element of the fitting process. Care should be taken to ensure that device orientation, care, and maintenance are well understood.
The final step in the fitting process is device validation and verification. This step is an essential one in the process to determine whether the device is providing expected benefit and, in the case of hearing aids, meeting prescribed targets. Numerous options exist to assist the clinician in verification of performance, including, but not limited to, electroacoustic analyses, real ear measurements, functional gain testing, and speech-in-noise testing.
The accepted protocol for hearing-aid verification includes electroacoustic analyses and real ear measurements. BAIs are expected to be more difficult to verify objectively. At present, clinical tools for assessing frequency-specific output levels of implantable devices are lacking. A common means of validation/verification is testing threshold responses to narrow-band signals through the implant in the sound field. This method provides only limited information regarding device performance with soft sounds in a quiet environment. Just as the pure tone audiogram is not an accurate representation of real-world listening abilities, functional gain measures are not an accurate representation of device performance and have long been criticized in the hearing-aid model. The authors’ recommendation is to repeat the previously described preoperative test protocol using speech-in-noise measures with the patient’s implant system in place. This action will validate whether the patient is receiving the listening-in-noise benefit predicted in the preoperative assessment. Speech-in-noise measures can also be used to evaluate performance at varying input levels. Such measures will help to verify soft-speech audibility and intelligibility, and identify whether loud speech is too loud or uncomfortable. Lack of objective measures to verify frequency and gain-specific output of implantable devices underscores the importance of a good clinical protocol to ensure success of a given treatment. The subsequent component of the validation process is postoperative and rehabilitative outcome measures such as the APHAB, GHABP, and SSQ previously discussed. It is recommended that at a minimum these are completed during the 2-week and 6-month follow-up appointments.
Management of rehabilitation of the VS patient
Over time, patients are subject to changes in both their auditory profile and communication needs. Validation of user benefit and satisfaction is a fundamental component of ensuring successful long-term management of the VS patient, which is best achieved using subjective measures to determine each patient’s individual needs. Much of the rehabilitation process relies on counseling. Simply empowering patients and their communication partners by enabling them to understand the auditory deficit instantly aids in the process of establishing realistic expectations. Following this, they can be successfully educated on how to optimize communication in their daily life. Global strategies are provided, but situation-specific strategies help each individual achieve success based on his or her personal communication needs.
Tinnitus
Tinnitus is the second most common complaint of patients with VS, and it has been estimated that approximately 70% of VS patients present with tinnitus. Although tumor removal improves or even resolves tinnitus in many patients, it can also result in worsening of tinnitus. In severe cases, tinnitus can be debilitating and can negatively affect quality of life.
Tinnitus is complex and difficult to treat. Historically, this has led many clinicians to avoid assessment and treatment of tinnitus during the rehabilitation process. However, given the prevalence of tinnitus in the VS population, it is the clinician’s responsibility to assess the presence, severity, and psychosocial impact of tinnitus in these patients. Many patients report tinnitus, but what dictates its management is the degree to which it affects the patient’s life. This extent can be determined by a thorough history and by using subjective measures such as the Tinnitus Handicap Inventory (THI) and the Tinnitus Reaction Questionnaire (TRQ). The THI is a validated tool for assessing the impact of tinnitus on daily living, and can be easily incorporated into the rehabilitation process. The TRQ is used to assess the psychological distress associated with tinnitus, and can be used to assess changes over time.
Several proposed treatment options are available for patients with tinnitus; however, reported results and success rates vary considerably. The perception of tinnitus can provoke emotional reactions. For this reason, many treatment options have included treating the emotional response rather than the tinnitus itself. A good treatment protocol addresses both the physiologic and psychological components of the disorder. For this reason it is essential to include subjective assessments as well as objective data. With the appropriate information many patients can be successfully remediated with counseling and/or cognitive behavioral therapy. During the counseling process, patients should be provided with information regarding the origin of their tinnitus, its relationship to their VS, the emotional response to the tinnitus, coping strategies, lifestyle management, and treatment options. In many cases, simply informing the patient can result in reduced stress and anxiety, thereby reducing the negative response to the tinnitus. The goal of cognitive behavioral therapy is to reduce the negative associations to tinnitus by changing thought processes to alter the emotional response of the patient.
Many current treatment protocols call for sound generators in the ipsilateral ear to either mask the tinnitus or facilitate habituation. The application of this approach is limited in postsurgical treatment because of the profound hearing loss. As a result, treatment of tinnitus in the VS population is met with even greater challenges. Neuromonics (Neuromonics Inc, Bethlehem, PA, USA) tinnitus treatment (NTT) suggests a contralateral protocol for the assessment and treatment of patients with unilateral severe to profound hearing loss. NTT uses an acoustic stimulation to promote desensitization by prescribing a broadband signal customized for each patient’s audiometric profile combined with relaxing music that intermittently covers the patient’s tinnitus perception. As early as 1983, Tyler suggested the possibility of masking tinnitus using the contralateral ear. Subsequent research, however, has been limited and warrants further study.
New approaches to managing tinnitus include repetitive transcranial magnetic stimulation (rTMS). rTMS stimulates the motor cortex using low-frequency magnetic pulses applied at the temporal lobe, which is thought to produce an inhibitory effect on the tinnitus. Although not readily available for clinical application, rTMS has shown promise in recent studies. Khedr and colleagues were able to demonstrate temporary reduction in tinnitus even when stimulation was at the contralateral temporal lobe. Given that rTMS acts at the cortical level rather than at the ear level by previously described devices, may prove it to be a viable option for the VS population.
Treatment of tinnitus should include a multidisciplinary approach involving physicians, audiologists, psychologists, and/or psychiatrists. In some patients the perception of tinnitus is so debilitating that it results in depression and anxiety. Signs or reports of extreme emotional distress should not be overlooked. Clinicians should familiarize themselves with severe emotional signs or reactions to tinnitus and should have a clear protocol in place indicating when to refer to a psychologist and/or psychiatrist as part of the multidisciplinary treatment plan.
Occasionally, auditory rehabilitation of patients with severe to profound UHL is complicated by the presence of debilitating tinnitus. Tinnitus is an extremely complex disorder that warrants comprehensive evaluation and management. The clinical assessment and treatment options related to patients with VS provided in this article should provide a practical overview to clinicians faced with the added challenge of tinnitus management. For further information, the reader is encouraged to consult other relevant articles.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


