This article is a concise clinical review of preoperative, intraoperative, and postoperative auditory evaluation of patients with acoustic neuroma. The author describes behavioral audiometry, auditory brainstem response, and otoacoustic emissions for preoperative evaluation; auditory brainstem and direct eighth-nerve intraoperative monitoring for intraoperative evaluation; and touches on postoperative auditory assessment.
Preoperative evaluation of acoustic neuroma
Behavioral Audiometry
Because patients with acoustic neuroma (AN) typically present with unilateral sensorineural (SNHL) hearing loss as their most common presenting symptom, most of them would already have had behavioral audiometry. This test evaluates the entirety of the auditory system, including the tympanic membrane/middle ear, cochlea, cochlear nerve, dorsal and ventral cochlear nuclei, trapezoid body and its nucleus, superior olivary nuclei, lateral lemniscus and its nuclei, inferior colliculus, medial geniculate body, auditory radiations via the posterior limb of the internal capsule, and finally the auditory cortex in the transverse gyri of Heschl. For the purpose of this section, the focus is on tests that may be done as part of the preoperative assessment of a patient with AN. Pure tone auditory thresholds and speech discrimination score (SDS) are the most important factors in preoperative decision making. Even patients with relatively poor pure tone thresholds would remain candidates for attempted hearing-preservation surgery if their SDS were good enough to allow successful amplification. Traditionally the 50/50 rule is used as a guideline in this decision making; that is, a patient with hearing equal to or better than 50 dB pure tone average (PTA) and better than 50% SDS may be considered for hearing-preservation surgery. This also, of course, depends on tumor size because the likelihood of hearing preservation is inversely proportional to increasing tumor size.
Auditory Brainstem Response
Some investigators advocate the use of auditory brainstem response (ABR) testing as a way to prognosticate chances for hearing preservation. In the absence of a good-quality ABR, some surgeons would advise translabyrinthine surgery because there would be no ABR signal to monitor during attempted hearing-preservation surgery. On the other hand, those surgeons who routinely use direct eighth-nerve monitoring (DENM) during surgery have found that a cochlear nerve action potential (CNAP) is routinely recorded even when preoperative ABR is poor or absent. Therefore, ABR is thought to be of little utility for preoperative assessment by surgeons using DENM because it does not influence their decision to attempt hearing preservation or their ability to monitor hearing intraoperatively.
ABR is a far-field technique for monitoring sound-evoked electrical activity in the auditory system from the cochlea/cochlear nerve through the brainstem. Because signal amplitude is negatively affected by increasing distance from the source of the neuronal activity, ABR has relatively small amplitudes on the order of tenths of a microvolt. In addition, averaging of hundreds to thousands of stimulus/response events is necessary to separate the desired signal from the random background electrical activity of the brain. Given the necessity of averaging many stimulus/response events, obtaining an ABR can take from 2 to 5 minutes. Pure tone thresholds less than 70 dB at 2 kHz and more are usually required to achieve an interpretable ABR. In patients with hearing worse than this, waveforms III through V may be of poor quality or absent. However, poor-quality or absent ABR waveforms do not preclude attempted hearing preservation during surgery because DNEM is often useful in this setting. Since the identification of ABR as a reliable tool in the assessment of the auditory system, a significant amount of research has endeavored to identify the location of the neural generators for the waveforms.
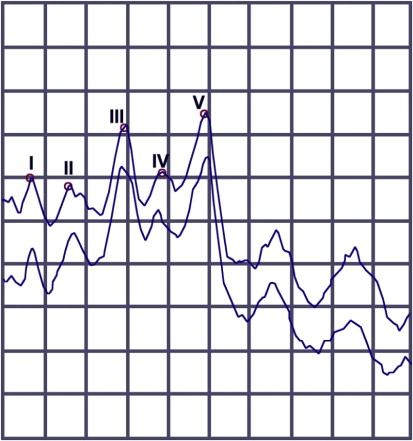
Animal studies investigating ABR, primarily in cats, were conducted in the mid- to late 1970s. Correlation of ABR waveforms with their neural generators in humans was investigated in the mid-1970s and continued into the 1990s by studies looking at ABR abnormalities related to known lesions of the central nervous system and studies using intracranially recorded auditory responses during surgery. Based on these investigations, generally accepted neural generators for ABR waves I and II have been established. However, the precise identity of the neural generators for waves III, IV, and V remains unclear because of conflicting reports from various laboratories. Fig. 1 demonstrates a normal ABR with the waveforms labeled with Roman numerals I through V. Table 1 indicates the first 5 ABR waveforms, their typical latencies, and their proposed neural generators. The most important waveforms regarding preoperative and intraoperative assessment of the auditory system in patients with ANs are I, III, and V. These waveforms correlate with the functional status of anatomic structures from the cochlea to the inferior colliculus. If these waveforms are present preoperatively then reasonable cochlear nerve integrity can be assumed. Likewise, if these waveforms are present at the conclusion of acoustic tumor surgery, the likelihood of hearing preservation is good.
| Waveforms | Proposed Neural Generators | Latency (ms) |
|---|---|---|
| I | Cochlear nerve: modiolus/IAC | 1.7 ± 0.15 |
| II | Cochlear nerve: proximal CPA portion | 2.8 ± 0.17 |
| III | Cochlear nucleus | 3.9 ± 0.19 |
| IV | Superior olive/lateral lemniscus | 5.1 ± 0.24 |
| V | Terminal fibers of lateral lemniscus into inferior colliculus | 5.7 ± 0.25 |
Otoacoustic Emissions
Otoacoustic emissions (OAEs) in their different variations (distortion product OAE and transient-evoked OAE) can differentiate cochlear from noncochlear hearing losses and, thus, may be useful in a retrocochlear screening test battery. Although the expected pattern would be one of poor hearing and intact OAEs, it was somewhat surprising to discover that more than half of ANs had reduced cochlear function as measured by OAEs. It has been shown that OAEs can be preserved in the setting of severe cochlear nerve dysfunction. Some tumors result in abnormally large OAE, presumably because of loss of efferent suppressions from tumor compression of the eighth cranial nerve. Intraoperative assessment of the auditory system is related to acoustic tumors because they are a measure of cochlear (outer hair cell) function and do not provide information regarding the auditory system more proximal to the cochlea. Nevertheless, intraoperative monitoring of OAE responses has been successfully accomplished, and responses were faster than ABR, suggesting their potential use within a battery of measures during surgery.
Intraoperative auditory assessment
Auditory Brainstem and Direct Eighth-Nerve Intraoperative Monitoring
The 2 most commonly used techniques for intraoperative auditory monitoring during AN resection are ABR and DENM. Because of early challenges maintaining electrode placement on the cochlear nerve during DENM, the technique fell into disfavor. This resulted in ABR becoming the most widely used auditory monitoring technique during AN surgery in the 1980s. However, the operating room poses several challenges to ABR monitoring. First, there can be a tremendous amount of electrical interference in the operating room, and ensuring that all equipment is properly grounded is necessary to minimize 60-Hz electrical interference that may overwhelm the ABR tracing. This susceptibility to electrical interference is related to the small response amplitudes found in far-field techniques, such as ABR. Another disadvantage of ABR for intraoperative monitoring during surgery is the inherent delay in obtaining a tracing. To compensate for the small response amplitudes, literally thousands of stimulus repetitions are required. At a stimulus rate of 11 per second, 2 to 3 minutes are typically needed to obtain an ABR tracing during surgery. This degree of time delay in the operative setting can allow irreversible damage to occur to the cochlear nerve or the cochlear blood supply. Injury to the latter is thought to be the predominant cause of hearing loss during AN removal.
The development of an electrode achieving more reliable and atraumatic positioning on the cochlear nerve in the late 1990s stimulated resurgence in the use of DENM. To perform DENM, the scalp electrode setup is the same as for performing ABR. The difference is that once the cochlear nerve is exposed, an electrode is placed on the cochlear nerve, preferably proximal to the area of tumor involvement. Because the electrode is placed directly on the nerve of interest, this is a near-field monitoring technique and therefore response amplitudes are much stronger than ABR reducing (but not eliminating) susceptibility to electrical interference. Typical CNAP responses are from 1 to 50 μV. Furthermore, because response amplitudes are larger, less averaging is needed to generate a reliable CNAP. DENM requires on average less than 20 stimulus/response events to record a CNAP. This translates to about 1 to 2 seconds to generate a CNAP, resulting in near instantaneous intraoperative feedback during AN surgery. Such rapid feedback regarding the integrity of the cochlea and cochlear nerve during tumor dissection allows for interruption of surgical maneuvers that may be placing undue stress on the nerve or cochlear blood supply. As mentioned earlier, studies have indicated that the CNAP, recorded from the proximal portion of the cochlear nerve, corresponds to wave II of the ABR.
In both ABR and DENM, the first sign of stress on the cochlear nerve or cochlear blood supply is a prolongation of the waveform latencies. Should further deterioration in function occur, response amplitudes begin to diminish. An exception to this can occur during DENM, when a drop in amplitude without a significant change in latency can occur if the area where the electrode is contacting the cochlear nerve is bathed in excess blood or cerebrospinal fluid (CSF). Blood in the area of the electrode/nerve interface appears to affect the CNAP recording more than CSF does. Preservation of CNAP at the conclusion of tumor removal is highly correlated with preservation of hearing. It is not uncommon to see CNAP amplitudes improve after tumor removal. The absence of a CNAP at the conclusion of tumor removal is likewise correlated with loss of hearing. Sometimes, however, hearing may be preserved despite an absent CNAP. This is likely caused by transient spasm of the internal auditory artery. The presence of good ABR waveforms is also highly correlated with hearing preservation, but the absence of a good ABR does not particularly predict hearing loss.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


