Chapter 57 Guide to Preoperative Parathyroid Localization Testing
![]() This chapter contains additional online-only content, available onexpertconsult.com.
This chapter contains additional online-only content, available onexpertconsult.com.
Introduction
Historically, preoperative localization studies for primary hyperparathyroidism were usually considered to be less important than the skill of the experienced parathyroid surgeon. The accuracy rate for the preoperative localization of a parathyroid adenoma for first-time operations was inferior to the results obtained by skilled surgeons.1–3 Approximately 95% of patients were cured after bilateral cervical exploration by experienced parathyroid surgeons without the help of localization studies.4,5 Furthermore, the use of localizing studies did not shorten operative and anesthesia times.1,4 However, in contrast to those who undergo a first-time operation, reoperative parathyroidectomy has higher failure and complication rates. Thus, localization studies are crucial for patients undergoing reoperation.
![]() Please see the Expert Consult website for more discussion of this topic.
Please see the Expert Consult website for more discussion of this topic.
The incidence of minimally symptomatic primary hyperparathyroidism rose dramatically as a result of routine measurements of serum calcium and the determination of serum parathyroid hormone by radioimmunoassay.6,7 For this reason, more patients were being referred for surgery, and some surgeons began to reassess the morbidity and the necessity of bilateral neck exploration.8–10 Although preoperative localizing studies were not necessary for patients undergoing initial bilateral neck exploration, current trends toward minimally invasive surgery with limited exploration of the neck are made possible by preoperative localization studies.
Parathyroid localizing studies have evolved since their inception in the late 1960s. Early attempts at localization were only occasionally successful. These included the use of 75Se-selenomethionine scanning,11,12,131I scintiscan,13 thermography,14,15 cine cervical esophagography,16–18 intravenous dye injection,19 angiography via injection of the thyrocervical trunk or inferior thyroid artery,20–22 pneumomediastinal radiolographic evaluation for glands located in the mediastinum,23,24 neck massage for parathyroid hormone (PTH) measurement,25,26 and thyroid lymphography.27 However, these methods are no longer used. Today, the role of preoperative localization studies is to assist the surgeon in identifying the exact anatomic location of a parathyroid tumor and enable a more focused or targeted exploration.28
In the age of minimally invasive parathyroidectomy, preoperative localization of the adenoma by imaging studies has become a necessity. Primary hyperparathyroidism is most likely caused by solitary adenomas (89%), whereas multigland disease (hyperplasia: 6%, double adenomas: 4%) and carcinoma (1%) are less common.29 Thus, minimally invasive parathyroidectomy is applicable to most patients with primary hyperparathyroidism. In this chapter, we review three types of parathyroid localization studies: radiology-based, nuclear medicine–based, and invasive procedures.
Localization Studies
![]() Please see the Expert Consult website for more discussion of this topic.
Please see the Expert Consult website for more discussion of this topic.
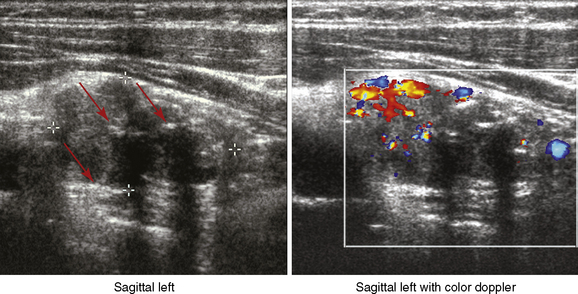
Ultrasonography to localize parathyroid tumors was first introduced in the late 1970s.30,31 Early ultrasound technology was limited to 5 MHz transducers, which gave static grayscale imagery.32 Currently, higher frequency transducers (10 to 15 MHz), along with color Doppler, allow for real-time sonographic images, and newer machines can perform three-dimensional computer reconstruction.33
Radiology-Based Studies
Ultrasonography
The sonographic appearance of a parathyroid adenoma is typically hypoechoic compared to the hyperechoic thyroid follicular nodules (Figure 57-1). Parathyroid glands are most commonly oval shaped but can be elongated, bilobed, or multilobed.34 Other abnormalities include parathyroid cysts, cystic components within larger solid lesions, giant adenomas, and calcifications. Parathyroid cysts are thin-walled structures, showing posterior enhancement and having no internal echoes. Cystic lesions within large solid adenomas can have anechoic areas with posterior acoustic enhancement. Giant adenomas are defined as those larger than 3 cm. Calcifications, although rarely found in parathyroid adenomas, are hyperechoic and cast discrete acoustic shadows (see Figure 57-1). Finally, an inhomogeneous pattern of hyperechoic and hypoechoic images may be found, corresponding to fat and hypercellular parathyroid tissue, respectively.
There are several advantages and disadvantages of ultrasound. Advantages of ultrasound are that (1) it is inexpensive, (2) there is no radiation or contrast exposure, (3) it is noninvasive, (4) it is excellent at detecting parathyroid tumors near the thyroid, (5) it identifies thyroid nodules,35 and (6) it can guide needle biopsy.3 The disadvantages of ultrasound are (1) it is operator dependent; (2) it misses substernal, retrotracheal, retroesophageal, and deep-seated parathyroid tumors; and (3) it is difficult to distinguish between small lymph nodes and small abnormal parathyroid glands.
Earlier studies of parathyroid ultrasound showed a wide range of sensitivities (20% to 79%),36,37 but a recent review showed the sensitivity and positive predictive value (PPV) of ultrasound ranging from 51% to 96% and 50% to 100%, respectively.38 This improvement is likely because of advances in sonographic technology as well as the increasing accumulated experience of surgeons and radiologists who perform neck ultrasound regularly. However, several factors decrease the sensitivity and PPV of ultrasound. These include concomitant thyroid nodules and multiple parathyroid adenomas or parathyroid hyperplasia.33–39 If in doubt, the clinician should consider performing percutaneous FNA of the lesion(s) in question and send the specimen for PTH measurement.
![]() Please see the Expert Consult website for more discussion of this topic.
Please see the Expert Consult website for more discussion of this topic.
Many surgeons prefer to perform their own neck ultrasound both preoperatively as a complementary addition to the physical exam, as well as intraoperatively as an aid for localization of a parathyroid adenoma. Ultrasound is used both to localize parathyroid adenomas and to evaluate the thyroid for pathology that may require concurrent operation.40,41 Surgeon-performed ultrasound in the clinic is convenient for patients because surgical decisions and operative planning can be made without multiple appointments. As more surgeons perform preoperative ultrasound, the cost may also decrease by streamlining care.42 Surgeon-performed ultrasound is as accurate as ultrasound performed by radiologists.40 Additionally, the surgeon can use ultrasound to determine the special relationship of the parathyroid to key anatomic landmarks (vascular and thyroid), which aids in placing the incision for minimally invasive parathyroidectomy.43,44
Surgeon-Performed versus Radiologist-Performed Ultrasound
Ultrasound is less accurate for localizing multiple adenomas or parathyroid hyperplasia whether it is performed by the radiologist or by the surgeon with sensitivities ranging from 13% to 24%.40,44 Overall, the accuracy of ultrasound depends on the experience and the interest of the person who performs it. Therefore, parathyroid surgeons need to be able to perform and interpret neck ultrasound.
![]() Please see the Expert Consult website for more discussion of this topic.
Please see the Expert Consult website for more discussion of this topic.
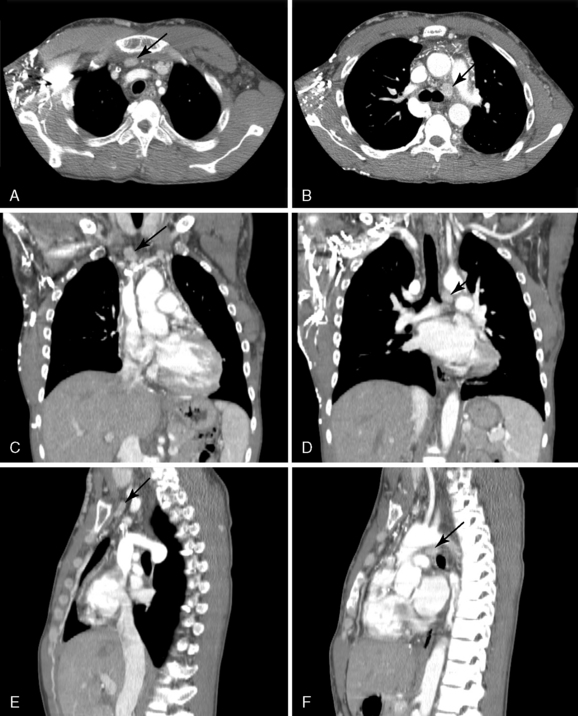
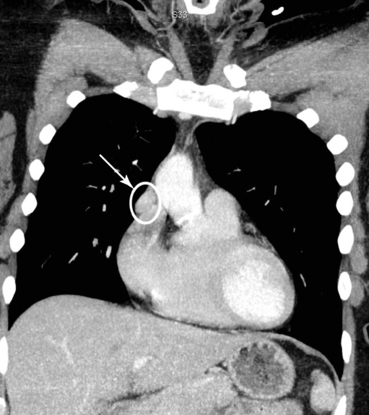
Computed tomography is generally considered to be a second-line imaging modality for parathyroid localization because of higher costs and radiation exposure. It is usually reserved for patients with persistent or recurrent hyperparathyroidism (Figure 57-3). It can be used when imaging tests such as ultrasound or sestamibi are negative, discordant, or ectopic.47,50,51 The criteria used to diagnose parathyroid disease on CT include site (extrathyroidal), morphology, demonstration of afferent vessels, and the degree of contrast enhancement relative to other structures in the neck.50 The expertise of the radiologist increases the accuracy of CT scanning as well.51,52 A retrospective study reported that for patients whose sestamibi scans were negative, thin-cut CT (2.5 mm collimation) helped locate the parathyroid tumor (lateralization: sensitivity 85%, specificity 94%; exact quadrant: sensitivity 66%, specificity 89%).53
Computed Tomography
Computed tomography is another noninvasive imaging technique used to localize abnormal parathyroid glands. The sensitivity of CT scans increases with the use of patient positioning harnesses (providing improved neck extension), intravenous contrast, and high-resolution CT scanners (2.5 to 3 mm cuts).45–47 The reported sensitivity of CT scans for localizing parathyroid adenomas ranges from 46% to 87%.48
There are several advantages and disadvantages of CT scanning in localizing abnormal parathyroid glands. CT is good for localizing ectopic glands, such as those in the anterior mediastinum or tracheoesophageal groove (see Figure 57-2). CT scanners are readily available in most hospitals, yield reproducible images, and can guide needle biopsy, and the interpretation is less subjective than for ultrasound. The disadvantages are the cost and exposure to radiation. Contrast enhancement is essential and it depends on the vascularity of the parathyroid gland.3,49 Small parathyroid glands next to the thyroid are harder to find, whereas lymph nodes, tortuous vessels and the esophagus may be mistakenly identified as parathyroid adenomas.48,49
![]() Please see the Expert Consult website for more discussion of this topic, including Figure 57-3.
Please see the Expert Consult website for more discussion of this topic, including Figure 57-3.
The so-called four-dimensional CT (4D-CT) adds to the timing of contrast perfusion to identify the adenoma. The 4D-CT can provide both the anatomic and physiologic details about the abnormal parathyroid gland in a single study. The parathyroid adenomas have rapid uptake and early washout of intravenous contrast compared to the thyroid. The 4D-CT scan was found in one study to be more accurate at localizing the parathyroid adenoma to a particular side (sensitivity: 4D-CT 88% versus sestamibi 65% versus ultrasound 57%) and quadrant (sensitivity: 4D-CT 70% versus sestamibi 33% versus ultrasound 29%) than either ultrasound or sestamibi.52
Magnetic Resonance Imaging
![]() Please see the Expert Consult website for more discussion of this topic, including Figures 57-4 and 57-5.
Please see the Expert Consult website for more discussion of this topic, including Figures 57-4 and 57-5.
Magnetic Resonance Imaging
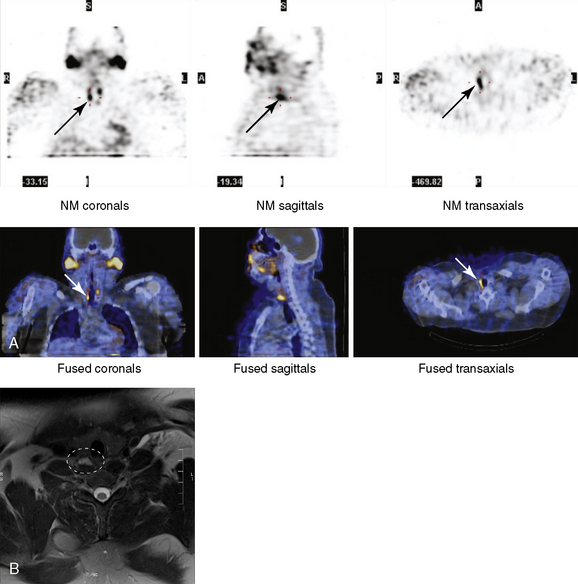
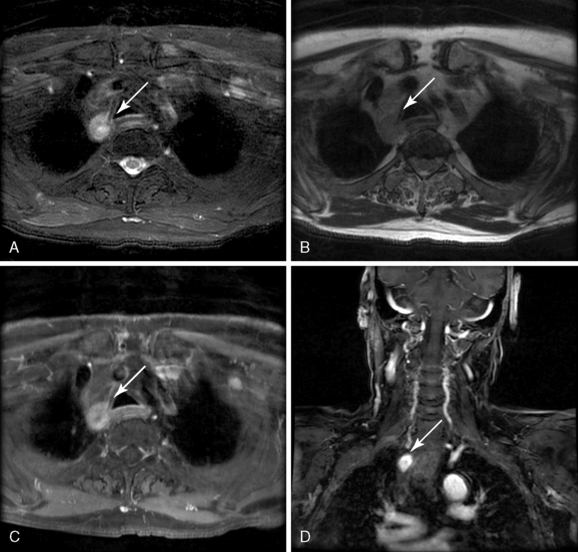
Like CT scanning, magnetic resonance imaging is primarily used as an adjunct for locating ectopic parathyroid glands and for patients who require reoperation because of persistent or recurrent hyperparathyroidism (Figure 57-4, B). A typical parathyroid adenoma on MRI is an enhancing lesion, with increased signal intensity on T2-weighted images and isointense on T1-weighted images (Figure 57-5). However, parathyroid adenomas may appear isointense or enhanced on both T1- and T2-weighted images.54 The sensitivity of MRI ranges from 50% to 88%, and it is very sensitive (up to 100%) for detecting ectopic parathyroid glands located in the mediastinum.55–57 Although MRI has improved over the years, enlarged lymph nodes or thyroid nodules can cause false positives.56,57 The advantages of MRI over CT scanning are that it does not require any ionizing contrast and has multiplanar capability with better tissue contrast.58 The disadvantages include cost and motion artifact, which makes interpretation difficult. MRI should not be the first or only imaging study performed, but it can be helpful when other imaging studies are negative or discordant. When MRI was combined with 99mTc MIBI scintigraphy, the sensitivity and positive predictive value were 94% and 98%, respectively.55 Future studies are needed to better define MRI’s exact role in parathyroid localization.
Nuclear Medicine-Based Studies
Introduction
![]() Please see the Expert Consult website for more discussion of this topic, including Figure 57-6, A and B.
Please see the Expert Consult website for more discussion of this topic, including Figure 57-6, A and B.
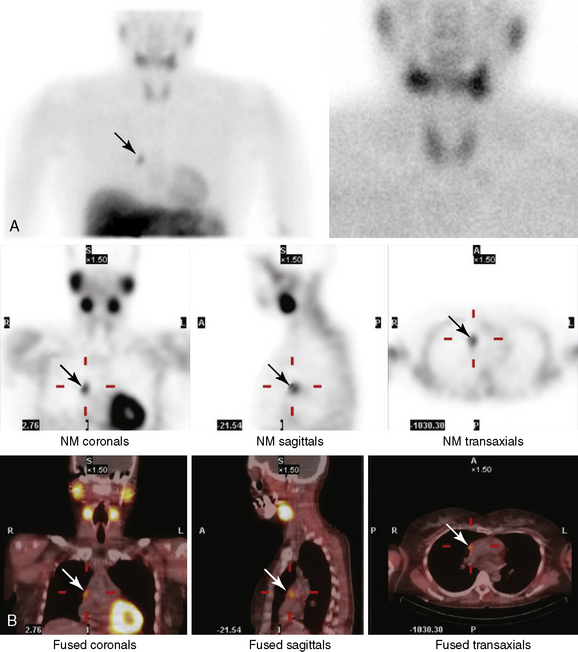
A basic understanding of how nuclear medicine scans work is important for understanding their advantages and limitations. Nuclear scintigraphy works by either oral or intravenous administration of a radionuclide tracer, which is preferentially taken up by the organ of interest. After the organ accumulates a sufficient amount of the tracer, the organ can be imaged by a by a gamma camera that captures gamma rays emitted by the radionuclide. Initially, nuclear medicine imaging was known as scintigraphy, which is now synonymous with traditional two-dimensional, or planar, nuclear medicine images. Planar nuclear images are produced by recording the image with a single gamma camera from a single point of reference (see Figure 57-6, A). Single-photon emission computed tomography (SPECT) improved on planar images by taking a series of two-dimensional images from multiple angles with either one or more gamma cameras. These images are reconstructed with a computer to produce three-dimensional tomographic images of the organ of interest (see Figure 57-6, B). The three-dimensional image adds more structural and anatomic information and improves the accuracy of localization.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree