Fig.18.1
Ex-Press glaucoma shunt (P model)
The Ex-Press device is made of implantable stainless steel similar to that used in cardiac stenting and is considered non-ferromagnetic [9, 10]. The device features an outer disc-like flange to stabilize depth of implantation and a spur-like inner projection to prevent extrusion after implantation [10, 11]. The flange and spur are designed and angled to conform to the anatomy of the peri-limbal sclera to stabilize the device [10]. There are three holes in the device near the distal tip providing an alternate conduit for aqueous humor flow, should blood, fibrin, or the iris block the main orifice [12]. The Ex-Press glaucoma filtration device was first described in 1998 in Israel and received the Food and Drug Administration approval in 2002. Approximately 75,000 devices have been implanted since that time [13].
Biocompatibility
In 2003, Nyska et al. found no evidence of active inflammatory reaction or tissue irritation at 3 and 6 months post-Ex-Press implantation in 8 rabbit eyes [10]. They reported a fibrotic capsule of variable thickness (up to 0.04 mm) surrounding the implants, devoid of inflammatory cells. Granulomatous inflammation and fibroblastic proliferation around foreign implants can be a major complication for glaucoma devices [14]. Aziz and colleagues described a histopathologic specimen of human ocular tissue surrounding an Ex-Press shunt [14]. They found minimal cellular reaction surrounding the implant and a thin fibrocellular tissue present deep to the implant. There was no granulomatous nor cellular inflammation identified around a shunt that had been in situ for 2 years. This biocompatibility may relate to the minimal tissue manipulation and trauma during implantation, as well as reduced cautery and absence of an iridectomy [10].
Indications
The general indications for implantation of an Ex-Press glaucoma shunt are similar to those for standard trabeculectomy and include failure to control IOP with maximal tolerable medical and/or laser therapy, nonadherence to medication (financial or physical restrictions), and intolerance of medical therapy (reactive or allergic) [12]. The Ex-Press shunt can be placed either nasally or temporally as long as there are 2–3 clock hours of viable conjunctiva available. This renders Ex-Press implantation a possible alternative in cases of failed glaucoma surgery where there is a small, non-scarred area of the remaining conjunctiva [15, 16]. Lankaranian and coworkers reported an IOP of 15 mmHg or lower 3 months after Ex-Press implantation in 65.3 % of patients who had previously undergone unsuccessful trabeculectomy [17].
The device is approved for use in open-angle glaucoma in phakic, pseudophakic, or aphakic eyes [18]. The use of an Ex-Press device has also been described in uveitic, pigmentary, traumatic, and neovascular glaucoma if there is no conjunctival scarring, inflammation, or uncontrolled bleeding [16, 19, 20]. There is, however, a potential risk of postoperative hyphema in neovascular glaucoma which may occlude the stent [1]. Dahan and Carmichael reported the use of Ex-Press devices in neovascular glaucoma secondary both to retinal vein occlusion and proliferative diabetic retinopathy [21]. After good initial lowering of IOP, 6 of the 12 cases failed owing to bleb fibrosis or uncontrolled rubeosis and 5 eyes had hyphema. Further reports of Ex-Press device use in chronic angle-closure and pseudoexfoliation glaucoma show good intermediate [17] (27 ± 13.2 months) and longer-term [22] (up to 5 years) success [1, 16, 19, 22]. Lankaranian and colleagues showed that the Ex-Press shunt lowered IOP to 5–21 mmHg with no medications in 55.4 % (83.7 %, with medications) of patients with primary open-angle, angle-closure, or pseudoexfoliative glaucoma over a mean follow-up period of 27 ± 13.2 months [17]. A single case report in 2007 described the efficacy of the Ex-Press glaucoma implant in an 11-year-old male with Sturge-Weber syndrome [23].
The Ex-Press device has shown short-term efficacy in the IOP reduction in vitrectomized eyes [24]. Ocular hypertension induced by pars plana vitrectomy is often resistant to medical therapy, and in cases where emulsified silicone oil blocks the trabecular meshwork, filtering surgery is a valid strategy. Vetrugno and colleagues reported four vitrectomized eyes with persistent ocular hypertension that following Ex-Press shunt insertion had IOP lower than 18 mmHg with no severe adverse effects [24]. There are no larger series or follow-up longer than 6 months published on this indication for Ex-Press implantation.
Ex-Press mini glaucoma shunt implantation in post-penetrating keratoplasty glaucoma has been reported since 2010 [25, 26]. In contrast to other glaucoma drainage devices, Ates and colleagues had relative success with the implantation of the Ex-Press device in patients with corneal grafts [25]. They reported a 93.3 % rate of glaucoma control (IOP <21 mmHg with or without medications) with a mean follow-up of 12.2 months. During this period of follow-up, there were no graft failures in their 15 eyes, with no observed endothelial damage related to the Ex-Press shunt, compared with that seen with other implantable devices [25, 27]. A potential advantage of a rigid metal shunt, if positioned correctly, is that it may be less likely than a flexible silicone tube to damage the endothelium.
Contraindications
In their discussion of Ex-Press shunt insertion, Sarkisian and colleagues discouraged implantation in patients with a narrow angle, owing to angle crowding and risks of endothelial and/or iris trauma [28]. In general, concurrent cataract extraction with Ex-Press insertion for IOP regulation has been recommended for cases of angle closure [12]. Congenital glaucoma and glaucoma associated with anterior segment dysgenesis (aniridia, Axenfeld-Rieger, or microphthalmia) are also relative contraindications for Ex-Press implantation. Such eyes often have thin sclera and altered angle anatomy, either of which may compromise successful and stable placement of an Ex-Press [29].
Another relative contraindication for Ex-Press implantation might be the presence of an anterior chamber intraocular lens [18]. Such a lens may increase risk of corneal endothelial damage should there be postsurgical hypotony with anterior chamber collapse.
Preoperative Considerations
At the preoperative review, the surgeon should determine the status and mobility of the conjunctiva and the health of the sclera in the anticipated surgical site, along with careful gonioscopy to determine angle depth and configuration. Peripheral anterior synechiae should be excluded near the planned insertion site. Lenticular status determines any need for combined cataract and glaucoma surgery [12]. If safe to do so, discontinuation of blood “thinners” may reduce the risk of intraoperative hemorrhage.
Anesthesia
Choice of anesthetic used for intraocular surgery depends on the patient, surgeon, and anesthetist [12]. Ex-Press shunt insertion is similar to trabeculectomy and can usually be performed under local or regional anesthesia (Video 18.1) [2, 7]. General anesthesia is required only in young, uncooperative, or disorientated patients.
Peribulbar, retrobulbar, and sub-Tenon injections are commonly used [12, 30]. Subconjunctival or topical anesthetic has been successful in cooperative patients, using tetracaine, lidocaine, or lignocaine jelly. Intracameral preservative-free lidocaine 1 % can be combined with topical anesthetic. Although no difference in pain has been reported when topical anesthesia is compared with peribulbar, the inability of the former to provide akinesia may compromise anterior chamber stability [31].
Surgical Technique
As originally conceived, the Ex-Press device was placed subconjunctivally [10]. This was associated with significant incidence of device erosion and overfiltration; in late 2005, implantation was reported to be safer under a scleral flap [11, 32]. This closely resembles trabeculectomy, requiring a conjunctival flap, scleral trapdoor, antimetabolite augmentation if indicated, and meticulous conjunctival closure [16, 33].
Optimal exposure of the surgical site can be attained with a corneal traction suture of 6/0–7/0 polyglactin or silk to infraduct the eye [12]. A standard fornix or limbal conjunctival incision in an upper quadrant allows access to the scleral bed, which is gently cauterized for hemostasis. The scleral flap can be shaped to the surgeon’s preference (square, rectangular, triangular, or trapezoidal), although shape is not as important as extension anteriorly to clear cornea. The flap should be at least 2.5 × 2.5 mm to cover the implant well by at least 1 mm around the plate [34]. Alternatively, a 5 × 5 mm limbus-based scleral flap of 50–60 % depth can be fashioned, with the dissection plane forward into clear cornea. At the surgeon’s discretion, an anti-fibrotic agent can be applied to the scleral flap and sub-Tenon’s tissue. The type, concentration, and exposure time of an anti-fibrotic agent will vary according to the patient’s individual needs.
A 26–27-gauge needle is used to create an ostium into the anterior chamber under the scleral flap. This incision should be placed in the center of the blue-grey transition zone between the sclera and cornea, approximately 1–2 mm from the surgical limbus to allow scleral reinforcement for the implanted device. The needle should be passed parallel to the iris plane and aimed at the center of the pupil. This avoids the device touching the iris or corneal endothelium in a normal depth anterior chamber. Any lateral movement as the needle perforates should be avoided to minimize the risk of aqueous leak around the implant [2]. A temporal limbal paracentesis facilitates ophthalmic visco-surgical insertion into the anterior chamber and/or the placement of an anterior chamber maintainer [33].
The Ex-Press glaucoma shunt, mounted on its introducer (Fig. 18.2), is inserted tip first, on its side, into the anterior chamber, radial to the limbus and parallel to the iris, through the perforation site. The shunt should be inserted all the way into the wound until the plate is flush with the scleral bed and then rotated through 90° so the plate lies flush with the scleral bed beneath the trapdoor (Fig. 18.3). The injector is depressed to retract the wire introducer, separate the inserter from the shunt, leaving the shunt in situ [35]. The scleral flap is sutured securely with 10/0 nylon sutures to cover the flange on the Ex-Press device. As in a trabeculectomy, sutures are placed in the scleral flap according to the surgeon’s preferred technique. The conjunctiva is replaced and sutured to prevent wound edge leakage.
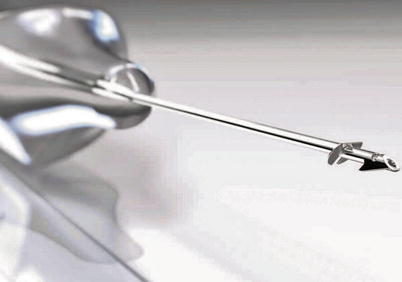

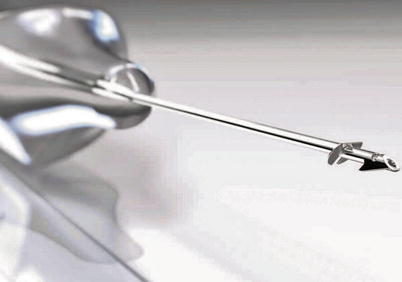
Fig. 18.2
Ex-Press shunt mounted on wire introducer

Fig. 18.3
Appearance of Ex-Press plate flush with the scleral bed, under the trapdoor
Modifications to Surgical Technique
Some authors have modified implantation techniques to enhance IOP reduction with the Ex-Press shunt. Mermoud described the use of a deep sclerectomy to simplify the difficult dissection of Schlemm’s canal and trabeculo-Descemet’s membrane [36]. He found that by performing a partial posterior deep sclerectomy and inserting an Ex-Press implant into the anterior portion under the superficial scleral flap, there were fewer postoperative complications.
In 2010 in 27 eyes, Bissig and colleagues [19] described a 4 × 5 mm limbus-based superficial scleral flap of 300-μm thickness and then removal of a rectangle of deep sclera (4 × 2 × 0.5 mm) in the posterior part of the scleral bed behind Schlemm’s canal, taking care not to open it [19]. A 21-gauge needle was used to enter the anterior chamber, through which an Ex-Press device of 200-μm lumen diameter was inserted. At 40.1 ± 10.8 months post-combined Ex-Press implantation in modified deep sclerectomy with phacoemulsification, Gindroz et al. reported complete (IOP <18 mmHg without medication) and qualified success rates (IOP <18 mmHg with medication) of 45.6 and 85.2 % respectively [37]. Modified deep sclerectomy possibly creates new outflow pathways for aqueous drainage through the suprachoroidal space as well as intrasclerally and subconjunctivally. This technique may be less technically demanding than the traditional non-penetrating procedure and may protect against device erosion, obstruction, or dislocation [19, 36, 37].
An Ex-Press shunt can be implanted at the same time as phacoemulsification surgery. Rivier and coworkers found a cumulative qualified success rate (IOP 6–18 mmHg with or without medication) of 53.7 % at 48 months (p < 0.05) [35]. Kanner and colleagues examined a further 114 eyes treated with Ex-Press implant under a scleral flap combined with phacoemulsification [38]. Their findings showed slightly worse long-term IOP control than trabeculectomy alone [38]. Three years after surgery, the authors found a surgical success (IOP 5–21 mmHg) of 95.6 % (with or without medications), with the most common device-related complication reported as tube obstruction by inflammatory matter.
Postoperative Management
Similar to trabeculectomy, postoperative topical treatment consists of frequent steroids and a prophylactic antibiotic. Most studies advocate these drops for at least 4 weeks, with or without tapering [24, 35, 39]. Cycloplegics can also be used for anterior chamber maintenance, especially in phakic eyes [7]. On the first postoperative day, the IOP can vary widely. There have been reports of increased IOP at 2–4 weeks postimplantation [3, 4, 33, 39]. This is usually self-limiting; however, interventions such as cessation of topical steroidal agents, suture lysis, suture release, or bleb needling can be performed as required. When an Ex-Press shunt bleb is needled, the anterior chamber cannot be entered and the needle should never be passed under the scleral flap radially as there is a risk of dislodging the shunt into the anterior chamber. Instead, the needle should be passed parallel to the limbus to elevate the scleral flap, and tactile feedback permits navigation over the base of the device [40].
Outcomes
The success rates of Ex-Press implantation in studies of greater than 20 subjects have been summarized in Table 18.1. The first publication detailing the short-term results of the Ex-Press glaucoma shunt, implanted subconjunctivally, reported a mean IOP reduction of 36 % from baseline with a 67 % probability of maintaining an IOP of 16 mmHg without medication [47]. Dahan and Carmichael pioneered the subscleral placement of the Ex-Press shunt in 2005, reporting significant reduction in IOP from 27.2 ± 7.1 mmHg preoperatively to 14.2 ± 4.2 mmHg after 24 months [11]. They found this technique of implantation to be safe with minimal side effects compared with previous reports of subconjunctival placement. Coupin and colleagues reported a short-term surgical success in 87 % of 99 eyes with an Ex-Press shunt placed under a scleral flap [48]. A longer-term study (follow-up 25.7 ± 11.1 months) of subscleral shunt placement found surgical success (IOP 5–21 mmHg) of 94.8 %, with a decrease in glaucoma medications from 3.7 ± 1.0 to 1.0 ± 1.4 at 42 months post-surgery [38].
Table 18.1
The success rates of Ex-Press implantation in published studies of greater than 20 subjects
Investigator | No. eyes | Study design | Type shunt | Definition of IOP reduction success | Types of glaucoma | % success | Follow-up (months) | Significant complications |
|---|---|---|---|---|---|---|---|---|
24 | Prospective | Prototype | ≥50 % | POAG (22), PXFG (2) | 41 % 1 year, 45 % 2 years | 17.8 (6.5–26) | Iris touch (1) | |
Traverso et al. [5] | 26 | Prospective multicenter | R50 | ≤21 mmHg with or without medication | POAG | 76.9 % | 23.9 ± 10.4 | Rotation (2) Erosion (3) |
Rivier et al. [35] | 35 | Prospective | R50 | Complete: 6–18 mmHg with no medications. Qualified: IOP 6–18 mmHG with or without medication | POAG (22), PXFG (13) | Complete: 32.7 % Qualified: 53.7 % | 36.9 ± 18.2 | Erosion (4) |
Maris et al. [16] | 50 | Retrospective | R50 | 5–21 mmHg with or without medication | POAG (37), PXFG (2), other (11) | 85.6 % | 10.8 (3.5–18) | Endophthalmitis (1) |
Gallego-Pinazo et al. [41] | 20 | Prospective | R50 | 5–21 mmHg without medication | POAG (14), PXFG (6) | 90 % | 9.7 (4.5–15) | N/K |
Kanner et al. [38] | 231 | Retrospective | T-50, R-50, X-50 | 5–21 mmHg with or without medication | POAG (157), PXFG (4), NVG (6), uveitic (11), CACG (7), other (46) | 94.8 % | 25.7 ± 11.1 (1–46.2) | Erosion (1) Dislocation (1) |
De Feo et al. [39] | 37 | Prospective | X-200 | <18 mmHg without medications | POAG | 78.4 % | 18 (12–24) | N/K |
De Jong et al. [43] | 40 | Prospective Randomized | Not stated | 4–18 mmHg without medication | POAG (38), PXFG (1), other (1) | 84.6 % | 12.4 ± 2.7 (0.3–13) | Iris touch (1) |
Bissig et al. [19] | 26 | Prospective | X-200 | Complete: 6–18 mmHg without medication Qualified: 6–18 mmHg with or without medication | POAG (8), PXFG (7), uveitic (2), CACG (1), other (8) | Complete: 69 % Qualified: 85 % | 18.6 ± 2.4 | N/K |
Good and Kahook [3] | 35 | Retrospective case control series | P-50 | Complete: 5–18 mmHg and 30 % decrease without medication Qualified: 5–18 mmHg and 30 % decrease with or without medication | POAG (21), CACG (5), PXFG (5), other (4) | Unqualified: 77.14 % Qualified: 82.85 % | 28 ± 3.2 | N/K |
Seider et al. [44] | 36 | Retrospective | R-50 (22), X-50 (11), not stated (3) | Complete: 6–21 mmHg with no medication Qualified: 6–21 mmHg with or without medication | POAG (28), PXFG (1), CACG (1), other (6) | Complete: 48 % Qualified: 91 % | 6–12 | Hypotony (1) |
Lankaranian et al. [17] | 100 | Retrospective | R-50, T-50 | Complete: 5–21 mmHg without medications Qualified: 5–21 mmHg with or without medications | POAG (67), CACG (13), PXFG (20) | Complete: 60 % Qualified: 24 % | 27 ± 13.2 (12–66) | Wound leak (1) Choroidal effusion (1) |
Marzette and Herndon [45] | 76 | Retrospective | Not stated | Complete: 5–21 mmHg without medications Qualified: 5–21 mmHg with or without medications | POAG (62), PXFG (3), other (11) | Complete: 69 % Qualified: 12 % | 9.1 ± 3.5 | Further glaucoma surgery (8) |
De Jong et al. [22] | 39 | Prospective Randomized | Not stated | Complete: ≤15 mmHg without medication Qualified: ≤15 mmHg with or without medication | POAG (37), PXFG (1), other (1) | Complete: 59.0 %
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|