Fig. 3.1
(a) Funduscopic view of right optic nerve. (b) Funduscopic view of left optic nerve
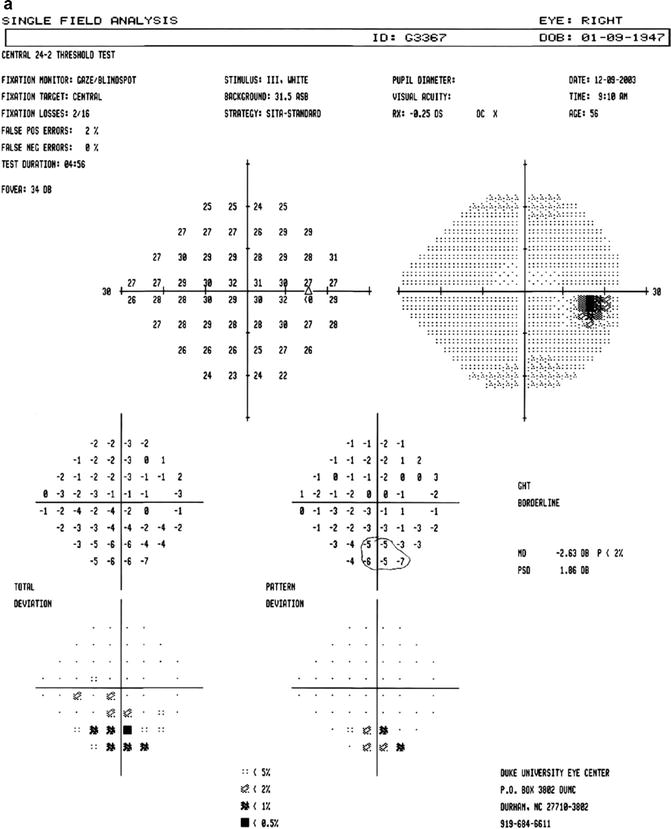
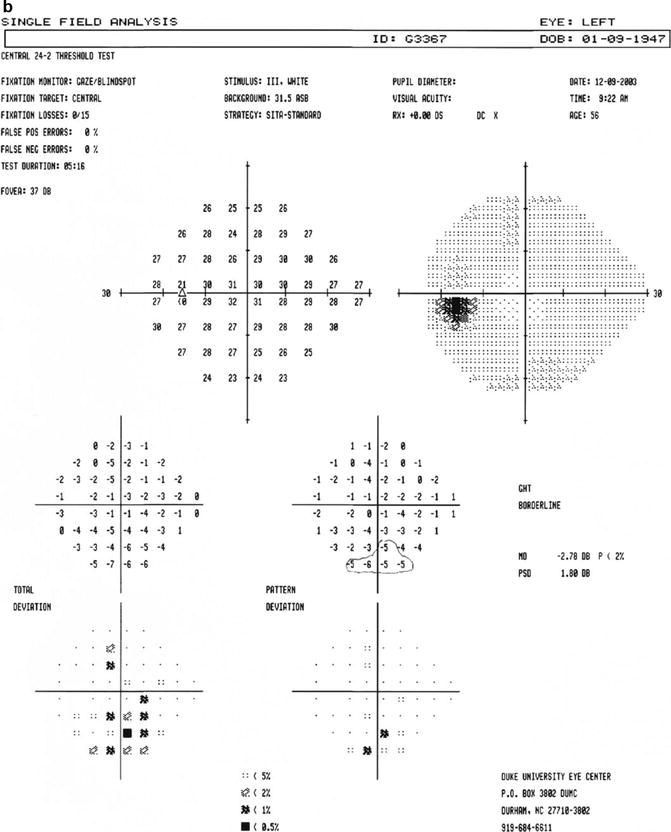
Fig. 3.2
(a) Humphrey visual field of right eye. (b) Humphrey visual field of left eye
The landmark Ocular Hypertension Treatment Study [2] (OHTS) was the first to prospectively demonstrate that a decreased CCT predicts the development of primary open-angle glaucoma (POAG). Ocular hypertensive participants with a CCT of 555 μm or less were three times more likely to progress to glaucoma than those with a CCT of greater than 588 μm. The OHTS also supported other clinical investigations that showed significant racial differences in CCT 3–6. There are no significant gender differences in the CCT of men and women.
In the 1970s, Ehlers et al. [3–5] performed a number of studies assessing the effect of CCT on IOP. They cannulated 29 otherwise normal eyes undergoing cataract surgery and correlated corneal thickness with errors in GAT. They found that GAT most accurately reflected “true” intracameral IOP when CCT was 520 μm and that deviations from this value resulted in an over-or underestimation of IOP by as much as 7 mmHg per 100 μm.
Across populations, patients with normal eyes have a CCT of approximately 540 μm. Patients with ocular hypertension have been found to have CCT values that are increased about 50 μm compared to glaucoma patients or controls [6, 7]. This means that many individuals have been falsely labeled as having ocular hypertension, when in fact they have normal IOP once CCT is taken into account.
Several studies have shown that some patients with normal tension glaucoma have thinner corneas than patients with normal eyes [8, 9]. Therefore, if CCT is taken into account, these patients may have elevated IOP with “high pressure” glaucoma. This underscores the importance of taking CCT measurements in all patients who have ocular hypertension or glaucoma.
Differences in CCT
Racial Differences
Blacks with glaucoma have CCT values that are on the order of 20 μm less than that of whites. Blacks have a six times higher incidence of POAG than whites. It is also known that the disease has an earlier onset in life and is more aggressive in its course among blacks. These differences in CCT may explain the more advanced progression of glaucomatous disease at a relatively lower measured IOP among blacks. Other evidence supports that this racial difference is not just among glaucoma patients but also among normal subjects. LaRosa et al. [10] reported thinner CCT values among normal black male veterans (mean thickness 530 μm) compared to their white counterparts (545 μm). In another study of patients at a large refractive surgery center, black patients also had thinner CCT values than white patients seeking surgery [11]. Further support of the racial differences can be found in one study that showed subjects who were of mixed black and white descent had CCT values that were intermediate between blacks and whites [12]. Hispanics [13] and Mongolians [14] have also been shown to have lower CCT values than their white counterparts.
Age-Related Differences
CCT increases beginning at infancy up to ages 2–4, at which time it reaches its adult thickness [15]. At some point in adulthood, CCT begins to decrease in at least some individuals [16]. The decrease appears to occur more markedly in glaucoma patients than in the normal population. One longitudinal study showed up to a 23 μm decrease over an 8-year period in glaucoma patients [17]. Therefore, not only should CCT be measured at the onset of suspicion or diagnosis of glaucoma, consideration should be given to measuring it approximately every 5 years thereafter to ensure proper management.
Corneal Refractive Surgery
At least one million LASIK surgeries are performed each year on predominately young- to middle-aged myopic patients. Myopia is recognized to be a strong risk factor for glaucoma [18]. Many of these LASIK patients are therefore genetically destined to develop glaucoma within a few decades of their procedure. In a patient who has had his cornea artificially thinned by a corneal refractive procedure, an IOP measurement taken by GAT can grossly underestimate the true value, hence the importance of doing CCT measurements on glaucoma patients and repeating them if a patient has any procedure that may compromise the CCT, such as LASIK. Tonometers that measure IOP independently of corneal thickness are generally more accurate than GAT in taking IOP in patients with corneas thinned by LASIK. One such tonometer is the dynamic contour tonometer (DCT; Ophthalmic Development Company (ODC) AG Zurich, Switzerland). DCT (Fig. 3.3) is a continuously recording type of tonometry that gives IOP and ocular pulse amplitude (OPA) [19]. The OPA is a measurement of blood flow entering the eye. The OPA is pulsatile and has maximum and minimum measurements, in association with the heart’s pumping action.


Fig. 3.3
The dynamic contour tonometer (DCT) (Ophthalmic Development Company (ODC) AG Zurich, Switzerland)
This DCT has a central gauge surrounded by a contoured plastic tip. This tip contacts the cornea and creates a tight-fitting shell, but does not applanate the cornea. The DCT compensates for all forces exerted upon the cornea. An electronic sensor measures IOP independently of corneal properties. A pilot study [20] was conducted that compared IOP measurements using GAT with DCT in patients who had undergone first-time LASIK with a median ablation of 90 μm. Preoperative and postoperative IOPs were measured. GAT was found to postoperatively underestimate IOP by as much as 5 mmHg, whereas DCT measurements did not change from the pre- to postoperative periods.
Other Factors
CCT may show diurnal variations with values highest in the mornings and progressively decreasing throughout the day. A single measurement taken between 11 a.m. and 2 p.m. captures the best estimate of a patient’s mean CCT [21].
Despite earlier concerns, CCT does not appear to be significantly affected in the long term by either phacoemulsification [22] or trabeculectomy [23].
CCT may be influenced by estrogen. Estrogen receptors are found in the human cornea. One study showed that CCT was thickest in women at the time of ovulation and at the end of the menstrual cycle than it was at the beginning [24, 25]. There is also evidence that CCT increases during pregnancy, another time when estrogen levels are elevated.
Disease processes can sometimes affect CCT. In the OHTS, subjects with diabetes were found to have slightly increased CCT values compared to their nondiabetic counterparts [17]. Diabetic patients who have had the disease for greater than 10 years may have abnormalities of the corneal endothelium, including a lower cell density and a greater variation of cell size than normal [26]. Diabetes may also cause corneal edema that can also contribute to an increased CCT.
Lamina Cribrosa
The lamina cribrosa is a sieve-like cartilaginous tissue in the posterior portion of the sclera through which the optic nerve and retinal vessels traverse. It is thought to be the site where damage from glaucoma primarily occurs [27]. Patients with larger optic discs also have a larger lamina cribrosa. Axonal damage and excavation of the inferior and superior disc areas are associated with higher lamina cribrosa pore-to-disc area ratio and thinner connective tissue support [28]. When the disc size is smaller, the pore-to-disc area ratio is also smaller, which allows for greater tissue support.
In addition, with all other factors being equal, the deformability of the optic disc with a smaller radius is less than that of one with a larger radius, in accordance with Laplace’s law. A study by Pakaravan et al. found that eyes with increased CCT were associated with smaller discs and thus a more robust optic nerve head [29]. It can therefore be implied that patients with lamina cribrosa with high pore-to-disc ratios (and greater lamina tissue) have thinner CCT values. This may make such patients more susceptible to glaucoma. However, this is an area where more research should be conducted before any firm conclusions can be drawn. A study of 111 enucleated eyes in patients without glaucoma showed no association between corneal thickness and lamina cribrosa thickness [30]. However, the lack of association may be secondary to postmortem- and preparation-induced changes. The cornea and the lamina cribrosa arise from similar tissues embryologically (the ectoderm). It therefore stands to reason that pathogenetic influences might affect them both [31].
Present Methods of Measuring CCT
Ultrasonic pachymetry is currently the most commonly used method for measuring the CCT. It entails the use of a probe that makes contact with the cornea and sends out an ultrasound signal that ultimately returns to the probe for analysis of corneal thickness. This technique has been shown to be both accurate and reliable [32]. Since the probe must come into contact with the cornea, local anesthesia is required. Also, there is a risk of infection and corneal indentation. Ultrasound measurements can be affected by the fluctuations in corneal hydration.
Modern methods of optical pachymetry use a camera that takes a series of three-dimensional images of the cornea to calculate the CCT. One example of this is the Oculus Pentacam (Oculus Inc. Lynnwood, Washington), which uses a rotating Scheimpflug camera that yields the CCT and other information from the anterior corneal surface to the posterior crystalline capsule [33].
The Orbscan system (Bausch and Lomb Inc., Rochester, New York) is another type of noncontact pachymetry that scans the anterior segment to provide maps that give CCT as well as anterior and posterior corneal topography measurements and elevation maps. The Orbscan has been shown to underestimate CCT in corneas with haze, particularly after LASIK [34].
Anterior segment optical coherence tomography (AS-OCT) obtains high-resolution cross-sectional images of the cornea and anterior segment. It allows for both central and regional pachymetry and for assessment of other anterior segment structures. It has been found to consistently give decreased CCT values relative to ultrasound pachymetry [35] (see Sidebar 3.1).
Sidebar 3.1. Pachymeters for Measuring Central Corneal Thickness
Odette V. Callender3
(3)
Chief of Ophthalmology, Wilmington VA Medical Center, Wilmington, DE, USA
Pachymetry is an important piece of the puzzle in evaluating glaucoma suspects and is recommended by the American Academy of Ophthalmology (Primary Open-angle Glaucoma Suspect Preferred Practice Pattern). A thin central corneal thickness (CCT) was found to be an independent risk factor for the development of glaucoma in the Ocular Hypertension Treatment Study (OHTS), European Glaucoma Prevention Study (EGPS), and the Barbados Eye Study. Ocular hypertensive patients with visual field loss, detected by either frequency doubling technology perimetry (FDT) or short-wavelength automated perimetry (SWAP), have significantly thinner corneas than those without such defects, and in a study by Meideros et al. a thin CCT was a significant predictor for the development of visual field loss in patients with preperimetric glaucomatous optic neuropathy.
Pachymetry may also be important in patients already diagnosed with glaucoma as some studies suggest that a thin CCT is a risk factor for the severity of glaucomatous disease. Glaucoma patients with thinner corneas have been reported to be more likely to present with more advanced glaucomatous optic nerve damage, increased vertical cup-to-disc ratios, greater visual field changes including more negative mean deviation, and higher Advanced Glaucoma Intervention Study (AGIS) score and use more glaucoma medications. This may be secondary to the higher risk of progression from ocular hypertension to glaucoma in patients with thinner corneas or it may represent a selection artifact in that patients with thinner corneas tend to have lower intraocular pressures and are therefore at greater risk for delayed detection of glaucomatous disease. Of five population-based studies, including the Barbados Eye Study, only the Rotterdam Study demonstrated an association between CCT and glaucoma suggesting that pachymetry is likely not a good screening tool for the presence of disease. Once present, progression of glaucomatous disease appears to be independent of central corneal thickness.
In summary, a thin CCT is associated with an increased risk of developing glaucoma (from ocular hypertension) and perhaps the severity of glaucoma at the time of presentation but not with the progression of glaucoma.
There are numerous pachymetry techniques available – ultrasound, Orbscan, partial coherence interferometry (PCI), the Pentacam Scheimpflug imaging system (Oculus), optical low-coherence reflectometer (OLCR), and anterior segment optical coherence tomography (AS-OCT). Of these, ultrasound is the current gold standard and is the technique utilized in OHTS, EGPS, and Barbados Eye Study. The results of these devices are not interchangeable as there may be significant differences in the pachymetry measurements obtained with each.
Measurements with optical pachymetry are generally thinner than with ultrasound. While multiple studies have shown that readings obtained with Orbscan are significantly thicker than ultrasound, one study found the opposite to be true.
Dedicated noncontact anterior segment optical coherence tomography (AS-OCT) devices produce high-resolution cross-sectional imaging of the cornea and can be used for pachymetry (in either automatic or manual modes). The SL-OCT (Heidelberg Engineering, Heidelberg, Germany) and Visante (Carl Zeiss Meditec, Dublin, California) are the two AS-OCT devices currently available and although similar in design and working principles differ in their CCT results and from ultrasound pachymeter readings. Studies by Kima et al. and Zhaoa et al. found that CCT with either the SL-OCT or the Visante OCT was significantly thinner that CCT obtained with ultrasound. Li et al. further demonstrated that results with these instruments can vary depending on whether measurements are obtained in automatic vs. manual mode. In their study, there was no significant difference in CCT between ultrasound and SL-OCT automatic or manual measurements. However, automatic Visante results were significantly less than ultrasound measurements, while the manual Visante numbers were significantly higher than ultrasound.
Partial coherence interferometry and Pentacam Scheimpflug imaging system produce smaller measurements than ultrasound. Rainer et al. found that even with ultrasound technology, different units can produce different results. They evaluated three different ultrasound pachymeters (DGH 500, DGH Technology Inc.; SP 2000, Tomey Inc.; Paxis, Biovision Inc.), and although the differences among the three devices were within 6.0 μm, they were statistically significant. The mean CCT values with the DGH 500, SP 2000, and Paxis were 541.0, 539.2, and 545.1 μm, respectively.
In the OHTS study, patients with a CCT < 555 μm (<558 μm in EGPS) were at greater risk for progressing to glaucoma irregardless of intraocular pressure or vertical cup-to-disc ratio. However, a value of 555 with Orbscan, anterior segment OCT, or optical pachymetry is not the same as a value of 555 with ultrasound. There is no known conversion factor to extrapolate measurements with one technique to a predicted value with ultrasound. Given the differences in results from the various pachymetry techniques, to interpret central corneal thickness measurements based on OHTS or EGPS data, you must use an ultrasound pachymeter realizing that even different ultrasound units can produce dissimilar results. If you have multiple offices, you should use the same type and brand of pachymeter throughout for consistency.
Despite the use of ultrasound pachymetry, the 555 μm OHTS or 558 μm EGPS threshold should only be applied to patients who meet the same criteria as participants of either study. The mean central corneal thickness of OHTS patients was 573 μm, with 24 % of them having a CCT > 600 μm. Doughty et al. showed that the average CCT in the normal population is 535–545 μm with only approximately 5 % patients having a CCT > 600 μm. The patient in your chair with a CCT of 540 mm may just be normal and not necessarily at increased risk of progressing to glaucoma.
In addition to method of measurement induced differences, pachymetry results are affected by refractive surgery, after contact lens wear for up to 2 weeks, and corneal drying decreasing by 3.0 % after 60 s of non-blinking. There are conflicting reports as to whether or not there is significant diurnal or long-term variation in CCT. Falsely increased measurements can result with ultrasound pachymetry if the probe tip is not placed straight and in the center of the cornea.
It is generally accepted that when using Goldmann applanation tonometry (GAT), IOP will tend to be higher than measured in thicker corneas and lower in thinner ones. In light of this, many have tried to correct IOP based on CCT readings. However, the Barbados Eye Study did not reveal clear trends in the relationship between corneal thickness and increasing IOP. In that study, there was a significant positive correlation between CCT and IOP in the white participants but not in the black and mixed race participants (even after omitting patients with OAG) who tended to have a thinner CCT but a higher IOP. A review of the literature reveals that the relationship of CCT on IOP is not linear with proposed correction factors varying from 1.1 to 7.14 mmHg IOP for every 100 mm in CCT. There is currently no standard nomogram for correcting applanation IOP measurements for central corneal thickness that has been fully validated. Even if there were a validated algorithm to correct IOP for CCT, recent work suggests that the effect of corneal thickness is less important than corneal elasticity on IOP measurements. Work by Liu and Roberts shows that while CCT accounts for 2.87 mmHg difference in predicted IOP readings, corneal elasticity accounts 17.26 mmHg. According to Dr. James Brandt, “two individuals can have the same pachymetry but one with a stiff cornea and the other with a soft cornea. Each has a large error, but in opposite directions; it is therefore possible to adjust IOP in the wrong direction in individuals with the same pachymetry measurement.” The amount of corneal elasticity/stiffness (corneal hysteresis) can be measured by the Reichert Ocular Response Analyzer, a bidirectional applanation process that utilizes a rapid air impulse to apply force to the cornea. The resultant amount of corneal deformation is then measured by an electro-optical system. Glaucoma patients have significantly lower corneal hysteresis and a much wider range than normals. Corneal hysteresis is only weakly correlated with CCT and is independent of IOP, and a lower corneal hysteresis was associated with VF progression in a recent study at Wilmer.
Glaucoma can occur with both low and high eye pressures, and patients with similar values do not progress in the same way. Our treatment goal is a percentage reduction (30–50 %) in IOP (irregardless of the starting pressure) not an absolute IOP number. Therefore, correcting the pressure, by whatever influence the corneal thickness may have on measured GAT IOP, generally will not significantly alter our treatment strategies. “Additionally, in the vast majority of patients, the ‘rule of thumb’ correction factor for CCT is only 1 or 2 mmHg, within the range of the repeatability of tonometry.”
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


