Glaucoma: Introduction
Glaucoma is an acquired chronic optic neuropathy characterized by optic disk cupping and visual field loss. It is usually associated with elevated intraocular pressure. There are different types of glaucoma (Table 11–1), which helps to explain, for example, why one patient with glaucoma may have no symptoms, while another experiences sudden pain and inflammation. In the majority of cases, there is no associated ocular disease (primary glaucoma).
| A. Primary glaucoma |
| 1. Open-angle glaucoma |
| a. Primary open-angle glaucoma (chronic open-angle glaucoma, chronic simple glaucoma) |
| b. Normal-tension glaucoma (low-tension glaucoma) |
| 2. Angle-closure glaucoma |
| B. Congenital glaucoma |
| 1. Primary congenital glaucoma |
| 2. Glaucoma associated with other developmental ocular abnormalities |
| a. Anterior chamber cleavage syndromes |
| Axenfeld-Rieger syndrome |
| Peters’ syndrome |
| b. Aniridia |
| 3. Glaucoma associated with extraocular developmental abnormalities |
| a. Sturge-Weber syndrome |
| b. Marfan’s syndrome |
| c. Neurofibromatosis 1 |
| d. Lowe’s syndrome |
| e. Congenital rubella |
| C. Secondary glaucoma |
| 1. Pigmentary glaucoma |
| 2. Exfoliation syndrome |
| 3. Due to lens changes (phacogenic) |
| a. Dislocation |
| b. Intumescence |
| c. Phacolytic |
| 4. Due to uveal tract changes |
| a. Uveitis |
| b. Posterior synechiae (seclusio pupillae) |
| c. Tumor |
| d. Ciliary body swelling |
| 5. Iridocorneoendothelial (ICE) syndrome |
| 6. Trauma |
| a. Hyphema |
| b. Angle contusion/recession |
| c. Peripheral anterior synechiae |
| 7. Postoperative |
| a. Ciliary block glaucoma (malignant glaucoma) |
| b. Peripheral anterior synechiae |
| c. Epithelial downgrowth |
| d. Following corneal graft surgery |
| e. Following retinal detachment surgery |
| 8. Neovascular glaucoma |
| a. Diabetes mellitus |
| b. Central retinal vein occlusion |
| c. Intraocular tumor |
| 9. Raised episcleral venous pressure |
| a. Carotid-cavernous fistula |
| b. Sturge-Weber syndrome |
| 10. Steroid-induced |
| D. Absolute glaucoma: The end result of any uncontrolled glaucoma is a hard, sightless, and often painful eye. |
About 60 million people have glaucoma. An estimated 3 million Americans are affected, and of these cases, about 50% are undiagnosed. About 6 million people are blind from glaucoma, including approximately 100,000 Americans, making it the leading cause of preventable blindness in the United States. Primary open-angle glaucoma, the most common form among blacks and whites, causes insidious asymptomatic progressive bilateral visual loss that is often not detected until extensive field loss has already occurred. Blacks are at greater risk than whites for early onset, delayed diagnosis, and severe visual loss. Angle-closure glaucoma accounts for 10%–15% of cases in whites. This percentage is much higher in Asians and Inuit. Primary angle-closure glaucoma may account for over 90% of bilateral blindness due to glaucoma in China. Normal-tension glaucoma is the most common type in Japan.
The mechanism of raised intraocular pressure in glaucoma is impaired outflow of aqueous resulting from abnormalities within the drainage system of the anterior chamber angle (open-angle glaucoma) or impaired access of aqueous to the drainage system (angle-closure glaucoma) (Table 11–2). Treatment is directed toward reducing the intraocular pressure and, when possible, correcting the underlying cause. Although in normal-tension glaucoma intraocular pressure is within the normal range, reduction of intraocular pressure may still be beneficial.
| A. Open-angle glaucoma |
| 1. Pretrabecular membranes: All of these may progress to angle-closure glaucoma due to contraction of the pretrabecular membranes. |
| a. Neovascular glaucoma |
| b. Epithelial downgrowth |
| c. ICE syndrome |
| 2. Trabecular abnormalities |
| a. Primary open-angle glaucoma |
| b. Congenital glaucoma |
| c. Pigmentary glaucoma |
| d. Exfoliation syndrome |
| e. Steroid-induced glaucoma |
| f. Hyphema |
| g. Angle contusion or recession |
| h. Iridocyclitis (uveitis) |
| i. Phacolytic glaucoma |
| 3. Posttrabecular abnormalities |
| a. Raised episcleral venous pressure |
| B. Angle-closure glaucoma |
| 1. Pupillary block (iris bombé) |
| a. Primary angle-closure glaucoma |
| b. Seclusio pupillae (posterior synechiae) |
| c. Intumescent lens |
| d. Anterior lens dislocation |
| e. Hyphema |
| 2. Anterior lens displacement |
| a. Ciliary block glaucoma |
| b. Central retinal vein occlusion |
| c. Posterior scleritis |
| d. Following retinal detachment surgery |
| 3. Angle crowding |
| a. Plateau iris |
| b. Intumescent lens |
| c. Mydriasis for fundal examination |
| 4. Peripheral anterior synechiae |
| a. Chronic angle closure |
| b. Secondary to flat anterior chamber |
| c. Secondary to iris bombé |
| d. Contraction of pretrabecular membranes |
Intraocular pressure can be reduced by decreasing aqueous production or increasing aqueous outflow, using medical, laser, or surgical treatments. Medications, usually administered topically, are available to reduce aqueous production or increase aqueous outflow. Surgically bypassing the drainage system is useful in most forms of glaucoma if there is a failure to respond to medical treatment. In recalcitrant cases, laser or cryotherapy can be used to ablate the ciliary body to reduce aqueous production. Improving access of aqueous to the anterior chamber angle in angle-closure glaucoma may be achieved by peripheral laser iridotomy or surgical iridectomy if the cause is pupillary block, miosis if there is angle crowding, or cycloplegia if there is anterior lens displacement. In the secondary glaucomas, consideration must always be given to treating the primary abnormality.
In all patients with glaucoma, the necessity for treatment and its effectiveness are assessed by regular determination of intraocular pressure (tonometry), inspection of optic disks, and measurement of visual fields.
The management of glaucoma is best undertaken by an ophthalmologist, but detection of asymptomatic cases is dependent on the cooperation and assistance of all medical personnel, particularly optometrists. Ophthalmoscopy to detect optic disk cupping and tonometry to measure intraocular pressure should be part of the routine ophthalmologic examination of all patients over 35 years of age. This is especially important in patients with a family history of glaucoma and in high-risk groups such as blacks, who should undergo regular screening every 2 years from age 35 and annually from age 50.
Intraocular pressure is determined by the rate of aqueous production and the resistance to outflow of aqueous from the eye.
The aqueous is a clear liquid that fills the anterior and posterior chambers of the eye. Its volume is about 250 μL, and its rate of production, which is subject to diurnal variation, is about 2.5 μL/min. The osmotic pressure is slightly higher than that of plasma. The composition of aqueous is similar to that of plasma except for much higher concentrations of ascorbate, pyruvate, and lactate and lower concentrations of protein, urea, and glucose.
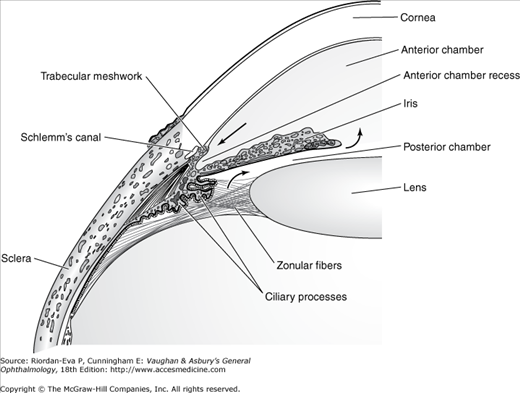
Aqueous is produced by the ciliary body. An ultrafiltrate of plasma produced in the stroma of the ciliary processes is modified by the barrier function and secretory processes of the ciliary epithelium. Entering the posterior chamber, the aqueous passes through the pupil into the anterior chamber (Figure 11–1) and then to the trabecular meshwork in the anterior chamber angle. During this period, there is some differential exchange of components with the blood in the iris.
Intraocular inflammation or trauma causes an increase in the protein concentration. This is called plasmoid aqueous and closely resembles blood serum.
The trabecular meshwork is composed of beams of collagen and elastic tissue covered by trabecular cells that form a filter with a decreasing pore size as the canal of Schlemm is approached. Contraction of the ciliary muscle through its insertion into the trabecular meshwork increases pore size in the meshwork, and hence the rate of aqueous drainage. Passage of aqueous into Schlemm’s canal depends on cyclic formation of transcellular channels in the endothelial lining. Efferent channels from Schlemm’s canal (about 30 collector channels and 12 aqueous veins) conduct the fluid directly into the venous system. Some aqueous passes between the bundles of the ciliary muscle into the suprachoroidal space and then into the venous system of the ciliary body, choroid, and sclera (uveoscleral flow) (Figure 11–1).
The major resistance to aqueous outflow from the anterior chamber is the juxtacanalicular tissue adjacent to the endothelial lining of Schlemm’s canal, rather than the venous system. But the pressure in the episcleral venous network determines the minimum level of intraocular pressure that can be achieved by medical therapy.
The major mechanism of visual loss in glaucoma is retinal ganglion cell apoptosis, leading to thinning of the inner nuclear and nerve fiber layers of the retina and axonal loss in the optic nerve. The optic disk becomes atrophic, with enlargement of the optic cup (see later in the chapter).
The pathophysiology of intraocular pressure elevation—whether due to open-angle or to angle-closure mechanisms—will be discussed as each disease entity is considered (see later in the chapter). The effects of raised intraocular pressure are influenced by the time course and magnitude of the rise in intraocular pressure. In acute angle-closure glaucoma, the intraocular pressure reaches 60–80 mm Hg, resulting in acute ischemic damage to the iris with associated corneal edema and optic nerve damage. In primary open-angle glaucoma, the intraocular pressure does not usually rise above 30 mm Hg and retinal ganglion cell damage develops over a prolonged period, often many years. In normal-tension glaucoma, retinal ganglion cells may be susceptible to damage from intraocular pressures in the normal range, or the major mechanism of damage may be optic nerve head ischemia.
Tonometry is measurement of intraocular pressure. The most widely used instrument is the Goldmann applanation tonometer, which is attached to the slitlamp and measures the force required to flatten a fixed area of the cornea. Corneal thickness influences the accuracy of measurement. Intraocular pressure is overestimated in eyes with thick corneas and underestimated in eyes with thin corneas. This difficulty may be overcome by the Pascal dynamic contour tonometer. Other applanation tonometers are the Perkins tonometer and the Tono-Pen, both of which are portable, and the pneumatotonometer, which can be used with a soft contact lens in place when the cornea has an irregular surface. The Schiotz tonometer is portable and measures the corneal indentation produced by a known weight. (For further discussion of tonometry, see Chapter 2; for tonometer disinfection techniques, see Chapter 20.)
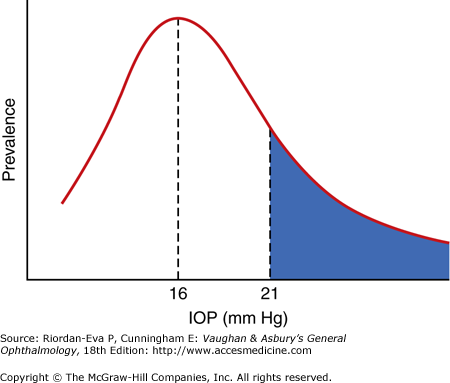
The normal range of intraocular pressure is 11–21 mm Hg (Figure 11–2). The distribution is Gaussian, but with the curve skewed to the right. In the elderly, average intraocular pressure is higher, giving an upper limit of 24 mm Hg. The intraocular pressure is subject to diurnal fluctuation throughout the day. In primary open-angle glaucoma, 32%–50% of affected individuals will have a normal intraocular pressure when first measured. Conversely, isolated raised intraocular pressure does not necessarily mean that the patient has primary open-angle glaucoma, since other evidence in the form of a glaucomatous optic disk or visual field changes is necessary for diagnosis. If the intraocular pressure is consistently elevated in the presence of normal optic disks and visual fields (ocular hypertension), the patient should be observed periodically as a glaucoma suspect.
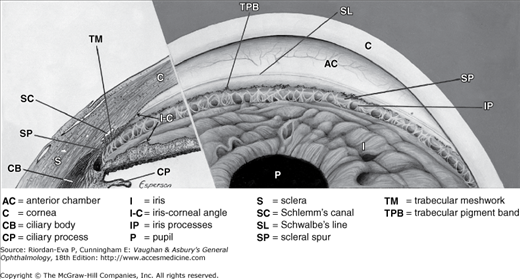
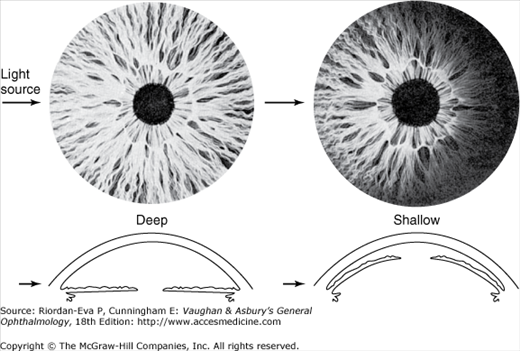
The anterior chamber angle is formed by the junction of the peripheral cornea and the iris, between which lies the trabecular meshwork (Figure 11–3). The configuration of this angle—that is whether it is wide (open), narrow, or closed—has an important bearing on the outflow of aqueous. The anterior chamber angle width can be estimated by oblique illumination with a penlight (Figure 11–4) or by slitlamp observation of the depth of the peripheral anterior chamber, but it is best determined by gonioscopy, which allows direct visualization of the angle structures (Figure 11–3). If it is possible to visualize the full extent of the trabecular meshwork, the scleral spur, and the iris processes, the angle is open. Being able to see only Schwalbe’s line or a small portion of the trabecular meshwork means that the angle is narrow. Being unable to see Schwalbe’s line means that the angle is closed.
Large myopic eyes have wide angles, and small hyperopic eyes have narrow angles. Enlargement of the lens with age narrows the angle and accounts for some cases of angle-closure glaucoma.
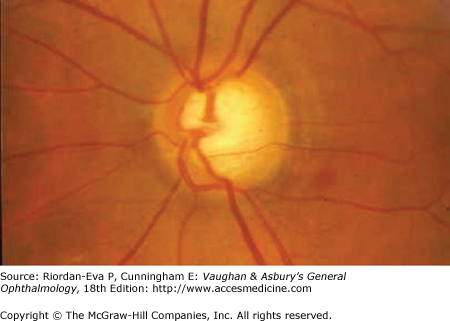
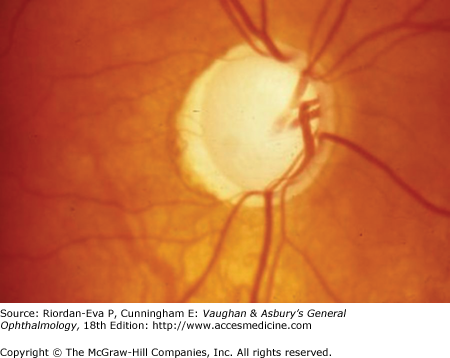
The normal optic disk has a central depression—the physiologic cup—whose size depends on the bulk of the fibers that form the optic nerve relative to the size of the scleral opening through which they must pass. In hyperopic eyes, the scleral opening is small, and thus the optic cup is small; the reverse is true in myopic eyes. Glaucomatous optic atrophy produces specific disk changes characterized chiefly by loss of disk substance—detectable as enlargement of the optic disk cup—associated with disk pallor in the area of cupping. Other forms of optic atrophy cause widespread pallor without increased disk cupping.
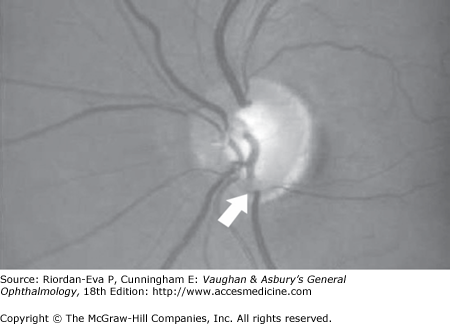
In glaucoma, there may be concentric enlargement of the optic cup or preferential superior and inferior cupping with focal notching of the rim of the optic disk (Figure 11–5). The optic cup also increases in depth as the lamina cribrosa is displaced backward. As cupping develops, the retinal vessels on the disk are displaced nasally (Figure 11–6). The end result of glaucomatous cupping is the so-called “bean-pot” cup in which no neural rim tissue is apparent (Figure 11–7).
The “cup–disk ratio” is a useful way of recording the size of the optic disk in glaucoma patients. It is the ratio of cup size to disk diameter, for example, a small cup is 0.1 and a large cup 0.9. In the presence of visual field loss or elevated intraocular pressure, a cup–disk ratio greater than 0.5 or significant asymmetry between the two eyes is highly suggestive of glaucomatous atrophy.
Clinical assessment of the optic disk can be performed by direct ophthalmoscopy or by examination with the 78-diopter lens or special corneal contact lenses that give a three-dimensional view (see Chapter 2).
Other clinical evidence of neuronal damage in glaucoma is atrophy of the retinal nerve fiber layer, which precedes the development of optic disk changes. It is detectable by ophthalmoscopy or fundal photography, both aided by using red-free light, optical coherence tomography, scanning laser polarimetry, or scanning laser tomography (see Chapter 2).
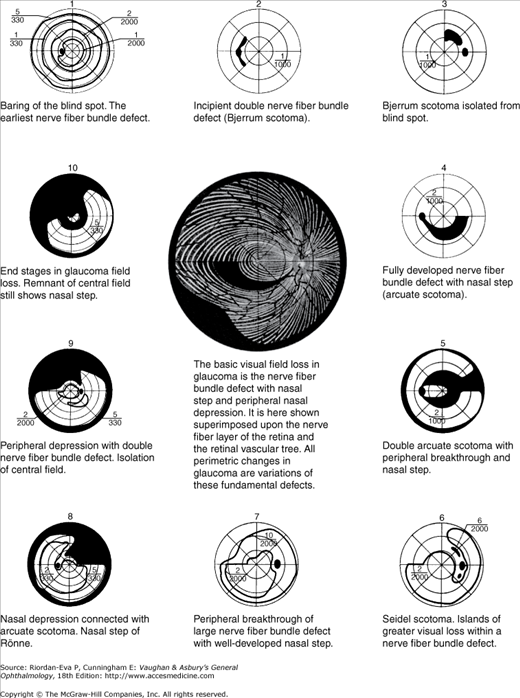
Regular visual field examination is essential to the diagnosis and follow-up of glaucoma. Glaucomatous field loss is not in itself specific, since it consists of nerve fiber bundle defects that may be seen in other forms of optic nerve disease; but the pattern of field loss, the nature of its progression, and the correlation with changes in the optic disk are characteristic of the disease.
Glaucomatous field loss involves mainly the central 30° of field (Figure 11–8). Contiguous extension of the blind spot into Bjerrum’s area of the visual field—at 15° from fixation—produces a Bjerrum scotoma and then an arcuate scotoma. Focal areas of more pronounced loss within Bjerrum’s area are known as Seidel scotomas. Double arcuate scotomas—above and below the horizontal meridian—are often accompanied by a nasal step (of Roenne) because of differences in size of the two arcuate defects. Peripheral field loss tends to start in the nasal periphery as a constriction of the isopters. Subsequently, there may be connection to an arcuate defect, producing peripheral breakthrough. The temporal peripheral field and the central 5°–10° are affected late in the disease. Central visual acuity is not a reliable index of progress of the disease. In end-stage disease, there may be normal central acuity but only 5° of visual field in each eye. The patient may have 20/20 visual acuity but be legally blind.
Various ways of testing the visual fields in glaucoma include the automated perimeter (for example, Humphrey, Octopus, or Henson), the Goldmann perimeter, the Friedman field analyzer, and the tangent screen. (For testing techniques, see Chapter 2.) Conventional automated perimetry, most commonly using the Humphrey perimeter, employs a white stimulus on a white background (white-on-white perimetry). Visual field defects are not detected until there is about 40% retinal ganglion loss. Refinements to detect earlier visual field changes include blue-on-yellow perimetry, also known as short-wavelength automated perimetry (SWAP), frequency-doubling perimetry (FDP), and high-pass resolution perimetry.
Topical beta-adrenergic blocking agents may be used alone or in combination with other drugs. Timolol maleate 0.25% and 0.5%, betaxolol 0.25% and 0.5%, levobunolol 0.25% and 0.5%, metipranolol 0.3%, and carteolol 1% solutions twice daily and timolol maleate 0.1%, 0.25%, and 0.5% gel once daily in the morning, some formulated without preservatives (preservative-free), are the currently available preparations. The major contraindications to their use are chronic obstructive airway disease—particularly asthma—and cardiac conduction defects. Betaxolol, with its relatively greater selectivity for β1 receptors, less often produces respiratory side effects, but it is also less effective at reducing intraocular pressure. Depression, confusion, and fatigue may occur with the topical beta-blocking agents. The frequency of systemic effects and the availability of other agents have reduced the popularity of the beta-adrenergic blocking agents.
Apraclonidine (0.5% solution three times daily and 1% solution before and after laser treatment) is an α2-adrenergic agonist that decreases aqueous humor formation without effect on outflow. It is particularly useful for preventing rise of intraocular pressure after anterior segment laser treatment and can be used on a short-term basis in refractory cases. It is not suitable for long-term use because of tachyphylaxis (loss of therapeutic effect over time) and a high incidence of allergic reactions. Epinephrine and dipivefrin have some effect on aqueous production but are rarely used these days.
Brimonidine (0.2% solution twice daily) is an α-adrenergic agonist that primarily inhibits aqueous production and secondarily increases aqueous outflow. It may be used as a first-line or adjunctive agent, but allergic reactions are common. It is available combined with timolol in the same solution.
Dorzolamide hydrochloride 2% solution, including a preservative-free preparation, and brinzolamide 1% (two or three times daily) are topical carbonic anhydrase inhibitors that are especially effective when employed adjunctively, although not as effective as systemic carbonic anhydrase inhibitors. The main side-effects are a transient bitter taste and allergic blepharoconjunctivitis. Dorzolamide is also available combined with timolol in the same solution, including a preservative-free preparation. Outside the United States, brinzolamide is available combined with timolol in the same solution.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree